|
|
|
Indian Pediatr 2020;57: 815-819 |
 |
Effect of Delayed Versus Early Cord
Clamping on Improving Anemia in Term Infants Aged Two Months or
Older - A Meta-analysis
|
|
Xin Fu, Dan Dang, Siwen Li, Zhiyan Xu and Hui Wu
From Department of Neonatology, The First Hospital of
Jilin University, Changchun 130021, China.
*Correspondence to: Dr Hui Wu, Department of
Neonatology, The First Hospital of Jilin University,NO.71 Xinmin Street,
Changchun, China 130 021.
Email: [email protected]
|
|
Objective: To assess the
effects of delayed cord clamping (DCC) on hemoglobin (Hb), mean
corpuscular volume (MCV) and ferritin level in infants 2 months
or older.
Evidence acquisition:
Meta-analysis of randomized control trials searched
systematically from PubMed, Cochrane and Web of science. Trials
published from Jan 1,1975 to Mar 12, 2018, no language and
country restrictions. Twelve studies were included in this
meta-analysis. In total, 993 infants were treated with DCC,
while 989 cases received early cord clamping. Delayed cord
clamping was defined as umbilical cord clamping time greater
than 60s after delivery. Outcomes assed were (i)
hemoglobin (Hb), (ii) mean corpuscular volume (MCV) and
ferritin level.
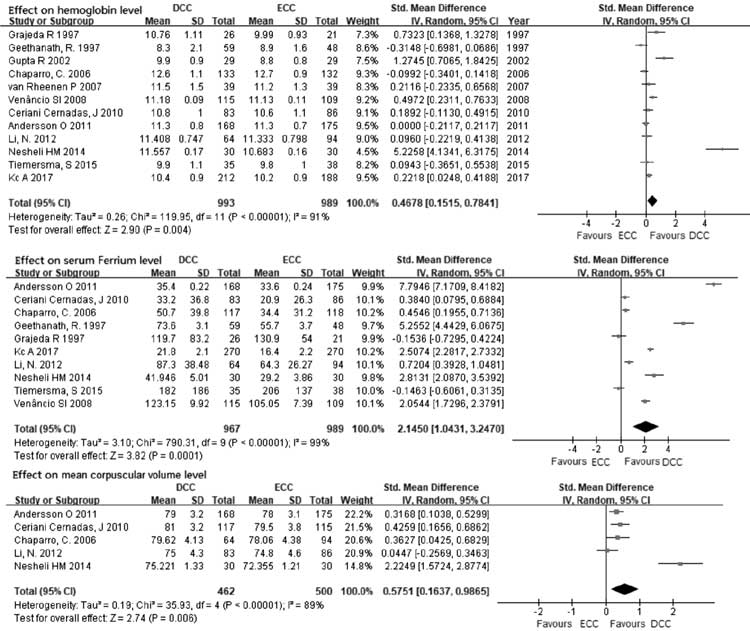
Results: The results show
that DCC increased hemoglobin level (SMD=0.4678 95%CI: [0.1515,
0.7841]), Ferritin level (SMD=2.1450 95%CI: [1.0431, 3.2470])
and MCV (SMD=0.5751 95%CI: [0.1637, 0.9865]) in infants between
2-12 months compared to ECC subject analysis noted the effects
of Hb increase was greater in Asian infants.
Conclusions: Delayed cord
clamping improved the Hb, MCV and ferritin level of infants
after birth.
Keywords: Hemoglobin, Infant,
Meta-analysis, Umbilical cord.
|
|
T
he appropriate timing of umbilical cord clamping
has been a matter of debate for long. Early umbilical cord clamping
(ECC) was standard practice but with emerging evidence it has started to
shift to delaying cord clamping (DCC) to beyond 30-60 secs. In term
infants, placental transfusion contributes between one-quarter and
one-third of total potential blood volume at birth [1]. At 1-minute,
newborn infants receives about 80 mL of blood while at 2-3 minutes it is
about 100 mL [2].
The American Association of Obstetricians guideline,
2017, states that DCC can increase hemoglobin levels at birth, and early
iron stores [3]. The guideline also recommends a delay in umbilical cord
clamping in vigorous term and preterm infants for at least 30–60 seconds
after birth. In addition, it can also benefit the preterm infants by
decreasing the need for blood transfusion, lowering incidence of
necrotizing enterocolitis and intraventricular hemorrhage. Previous
systematic reviews [4,5] have reported the advantages of DCC, but mainly
as a dichotomous variable, and mainly during the neonatal period [6].
The present systematic review and meta-analysis reports change in
hemoglobin between ECC and DCC in infants 2 months or older.
METHODS
All relevant studies published between January 1,
1975 and March 8, 2018 were identified by searching PubMed, Cochrane
reviews and Web of science. The Search strategy used the terms
(((delayed cord clamping [Title/Abstract]) OR delayed cord ligation
[Title/Abstract])) OR ((late cord clamping [Title/Abstract]) OR late
cord ligation [Title/Abstract]))) Filters: Randomized Controlled Trial.
There was no language limitation in the selection.
Studies were screened and selected by the following
criteria: (a) randomized controlled trials (except quasi
randomized study); (b) singleton newborns, no developmental
deformity, no gestational age limit; (c) clinical trial data
included hemoglobin, mean corpuscular volume
(MCV) and ferritin; (d) delayed cord
clamping was in intervention group, and early cord clamping was in
control group; (e) the outcomes’ were measured at 2 months or
more after birth. Articles were excluded if it was a conference summary;
had Incomplete data; presence of maternal complications (antepartum
blood loss, pregnancy-induced hyper-tension, pre-eclampsia and
gestational diabetes); history of post-partum hemorrhage (PPH), there
was need for neonatal resuscitation, or history of fetal distress.
The following data were extracted from each selected
study: Region where study was performed, total number of participants,
gestational age, follow-up time, and the effect of DCC versus ECC beyond
2 months were also compared; hemoglobin as the main outcome, MCV or
ferritin as a secondary outcome.
For meta-analysis, RevMan 5.3 of the Cochrane
Collaboration and stata 12.0 was used [6]. The Cochrane risk bias
assessment tool was used to assess the bias in the included studies.
Clinical and methodological heterogeneity of the included studies were
analyzed, and subgroup analysis were conducted according to clinical and
methodological heterogeneity. The I 2
index was calculated to assess the degree of
heterogeneity. In the absence of heterogeneity (P³0.05;
I2£50%),
a fixed effect model was used; if there was heterogeneity between
studies (P<0.05; I2>50%),
a random effects model was used. Sensitivity analysis was used to assess
the stability of the results. Continuous data were expressed as Standard
mean difference (IV, Random, 95% CI). Funnel plots was used to analyze
for possible publication bias. Funnel plot asymmetry was assessed using
Egger tests, and significant publication bias was defined as a P
value<0.1. If publication bias existed, the trim-and-fill computation
was used to estimate the effect of publication bias on the
interpretation of the results.
The entire process was completed by two independent
investigators, and the disagreement if any, was resolved by a third
investigator.
RESULTS
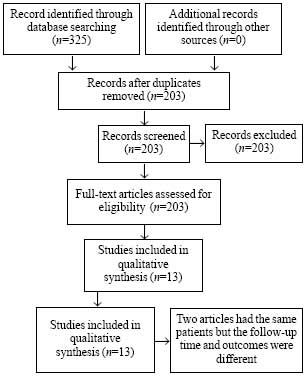
A total of 325 studies was identified, with 13
publications fulfilling eligibility for inclusion. [7-19] (Fig.
1). Two articles written by Andersson, et al. [9,19] have the
same patients but the follow-up time and outcomes were different. So
these two articles were regarded as one trial and outcomes extracted
accordingly. The characteristics of all included trials is presented in
Table I. Follow-up time was between 2 months and 12 months.
The effect of ECC and DCC on hemoglobin was assessed in 12 trials,
ferritin in 10 trials and MCV in 5 trials. In total, 993 infants were
treated with DCC, while 989 cases received ECC. All of these infants
were term infants. These trials used different definition of DCC, but
all were pooled, and DCC was redefined as umbilical cord clamping time
greater than 60s after delivery.
 |
|
Fig.1 Study selection for the
meta-analysis.
|
Table I Characteristics of Included Studies Comparing Early and Delayed Cord Clamping
|
Study; place, year |
Sample
|
Gestational age |
Intervention method
|
Outcomes
|
|
(DCC/ECC) |
(DCC/ECC) |
DCC/ECC |
|
|
KC, et al. [7]; Nepal, 2017 |
212/188 |
38/38 median |
³180s/£60s |
Hb and ferriten level at 8-mo
|
|
Tiemersma, et al. [8]; |
35/38 |
38/38 median |
120-180 s/£30s |
Hb level at 2-3 mo
|
|
South Africa, 2015 |
|
|
|
|
|
Andersson, et al.* [9]; |
168/175
|
40.0/40.1 mean |
³180s/£10s |
Hb and MCV level at 4-mo
|
|
Sweden, 2011-2014
|
150/144
|
|
|
Ferritin level at 12-month |
|
Ceriani Cernadas, et al. [10]; |
83/86 |
39/39 median |
180s/<15s |
Hb and MCV level at 6-mo
|
|
Argentina, 2010
|
|
|
|
Ferritin level at 6-mo
|
|
Chaparro, et al. [11];
|
171/157 |
38.8/39.0 mean |
120s/around 10s |
Hb and MCV level at 6-mo
|
|
Mexico, 2006 |
|
|
|
Ferritin level at 6-mo
|
|
Geethanath, et al. [12]; |
59/48 |
Term infants |
Placenta into
|
Hb level at 3-mo
|
|
India, 1997 |
|
|
vagina/ICC
|
Ferritin level at 3-mo
|
|
Li, et al. [13]; China, 2012 |
64/94 |
38.6/38.7 mean |
60s/15s |
Hb and MCV level at 4-mo Ferritin level at 4-mo
|
|
Nesheli, et al. [14]; Iran, 2014 |
30/30 |
40/40 mean |
50-60s/ICC
|
Hb, ferritin and MCV level at 6-mo
|
|
Venâncio, et al. [15];
|
115/109 |
39.3/39.3
|
60s/ICCh |
Hb level at 3-mo
|
|
Brazil, 2008 |
|
median |
|
Ferritin level at 3-mo
|
|
van Rheenen, et al. [16]; |
39/39 |
40/40 mean |
>60s/20s |
Hb level at 4-mo
|
|
Zambia, 2007 |
|
|
|
|
|
Gupta, et al. [17]; |
29/29 |
39.1/39.4 mean |
Placenta into |
Hb level at 3-mo
|
|
India, 2002 |
|
|
vagina/ICC
|
|
|
Grajeda, et al. [18]; |
26/21 |
38.8/38.5 mean |
Cord stopped |
Hb level at 2-mo
|
|
Guatemala, 1997 |
|
|
pulsating/ICC
|
Ferritin level at 2-mo
|
|
*Includes two articles with the same patients, the sample
168/175 at 4-month, the other at 12-month; DCC-delayed cord
clamping; ECC-early cord clamping; ICC-cords clamped immediately
after the birth ; Hb-hemoglobin; MCV-mean corpuscular
volume. |
Web Fig. I depicts the assessment of risk of
bias in the included trials. Eight studies [7-12,13,16,17] clearly
indicated the method of randomization, 9 studies [7,8,12-18] did not
indicate if the study was blinded.
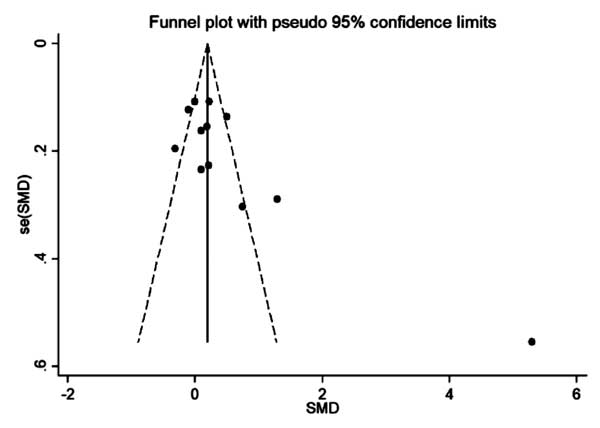
There was little publication bias on funnel plot (Fig.
2) and Egger test (P=0·073) in this analysis. However,
further analysis with trim-and-fill test indicated that this publication
bias could not impact the estimates (no trimming done because data was
unchanged).
 |
|
Fig. 2 Forest plots comparing effect
of early and delayed cord clamping on various hematological
parameters.
|
To study the effect of DCC compared to ECC on
hemoglobin level the sample size varied significantly among the included
studies and there was heterogeneity (I 2=91%),
so a random effects model was used to analyze the results. One trial in
our study did not mention the unit [16], so outcomes have taken SMD to
analyze. The results obtained show that DCC resulted in higher
hemoglobin levels compared to ECC (SMD=0.47; 95% CI: 0.15, 0.78) (Fig.
3). DCC resulted in significantly higher ferritin levels compared to
ECC (SMD=2.14; 95% CI: 1.04, 3.25) (Fig. 3). Similarly DCC
resulted in significantly higher MCV levels compared to ECC (SMD=0.57;
95% CI: 0.16, 0.99) (Fig. 2).
 |
|
Fig. 3 Funnel plot of studies
comparing early and delated cord clamping.
|
Subgroup analysis on effect of DCC and ECC on
hemoglobin was performed by race (Web Fig. 2.1), timing of
DCC (120s as the critical value) (Web Fig. 2.3) and the
follow-up time of DCC (6 months as the critical value) (Web Fig.
2.2). DCC improved Hb significantly compared to ECC in Asian
studies, when follow-up was more than 6 months and when timing cord
clamping was not beyond 120 secs. Accordingly, the race of participants,
timing and follow-up time of DCC can be regarded as a source of
heterogeneity.
DISCUSSION
The results obtained show that DCC could increase the
level of hemoglobin, MCV and especially ferritin when compared with ECC.
The influence could be different based on participants’ regional
distribution, timing of umbilical cord clamping and the age of infants.
The optimal time to delay umbilical cord ligation which impacted
hemoglobin levels is about 60-120s.
Some studies have indicated that the differences in
hematologial variables between DCC and ECC became smaller with the
increased follow-up time [7,9]. A randomized controlled trial in Sweden
demonstrated that DCC significantly increased stored iron at 4 months,
but the effect on hemoglobin was not significantly different from ECC.
When the follow-up reached 12 months, the beneficial effect on iron
storage disappeared. This might be related to the postnatal iron
supplementation. A previous study [11]
showed that during the three-month follow-up, hematologic
improvement was enhanced in iron-deficient mothers, infants with infant
birth weights between 2500 and 3000 grams, and infants who did not
receive infant formula or iron fortified milk. A previous meta-analysis
including 6 trials about hemoglobin level showed no significant
difference in the hemoglobin levels within 6 months.
The study has some limitations. Firstly, the timing
of cord clamping varied from 60 seconds till descent of placenta into
vagina or cord stopped pulsating, and in the latter the means used were
approximate estimates. Secondly, all studies had loss to follow-up.
Since acute inflammatory process could increase the ferritin
concentration, there might be an error in the result of ferritin.
There is also a long way to go in the optimization of
umbilical cord ligation. In addition, countries should develop DCC
guidelines based on race, gender, and physical status of pregnant women
in order to improve the blood volume and iron storage of newborns more
effectively.
As there is a high incidence of anemia and low iron
stores in Asian and African infants [7,12,16], DCC might be an effective
intervention to prevent anemia and iron deficiency in developing
countries.
Contributors: XF: contributed to conception and
design, acquisition, analysis, and interpretation; DD: contributed to
conception and design, acquisition and interpretation; SL: contributed
to conception and design, acquisition; ZX: contributed to conception and
design, analysis; HW: contributed to conception and design, acquisition,
analysis, and interpretation. All authors drafted manuscript, critically
revised manuscript, gave final approval and agree to be accountable for
all aspects of work ensuring integrity and accuracy.
Funding; None; Competing interest: None
stated.
|
WHAT IS ALREADY KNOWN?
• Delayed cord clamping provides adequate
blood volume and birth iron stores, thus decreasing the risk of
iron deficiency anemia during infancy
WHAT THIS STUDY ADDS?
• The optimal time to delay umbilical
cord ligation is about 60-120s and it will be more conducive to
the growth of hemoglobin than the longer umbilical clamping
time. In contrast, Asians might gain more benefits from delayed
umbilical clamping.
|
REFERENCES
1. Farrar D, Airey R, Law GR, Tuffnell D, Cattle B,
Duley L. Measuring placental transfusion for term births: Weighing
babies with cord intact. BJOG.. 2011;118:70-5.
2. Ceriani Cernadas JM. Timing of umbilical cord
clamping of term infants [J]. Arch Argent Pediatr, 2017;115:188-94.
3. Committee on Obstetric Practice, (2017). Committee
Opinion No. 684: Delayed Umbilical Cord Clamping After Birth, Obstet
Gynecol, 2017;129;e5-e10.
4. Hutton EK, Hassan ES. Late vs early
clamping of the umbilical cord in full-term neonates: Systematic review
and meta-analysis of controlled trials. JAMA. 2007; 11:1241-52.
5. Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter
K, Lui K, et al. Delayed versus early umbilical cord clamping for
preterm infants: A systematic review and meta-analysis. Am J Obstet
Gynecol. 2018;218:.
6. McDonald SJ, Middleton P, Dowswell T, Morris PS.
Cochrane in context: Effect of timing of umbilical cord clamping in term
infants on maternal and neonatal outcomes. Evid Based Child Health.
2014;9:398-400.
7. Kc A, Rana N, Malqvist M, Jarawka Ranneberg L,
Subedi K, Andersson O. Effects of delayed umbilical cord clamping vs
early clamping on anemia in infants at 8 and 12 months: A randomized
clinical trial. JAMA Pediatr. 2017;171: 264-70.
8. Tiemersma S, Heistein J, Ruijne R, Lopez G, van
Lobenstein J, van Rheenen P. Delayed cord clamping in South African
neonates with expected low birthweight: A randomised controlled trial.
Trop Med Int Health. 2015;20:177-83.
9. Andersson O, Hellstrom-Westas L, Andersson D,
Domellof M. Effect of delayed versus early umbilical cord clamping on
neonatal outcomes and iron status at 4 months: a randomised controlled
trial. BMJ. 2011;343:d7157.
10. Ceriani Cernadas JM, Carroli G, Pellegrini L,
Ferreira M, Ricci C, Casas O, et al. Efecto del clampeo demorado
del cordón umbilical en la ferritina séricaa los seis meses de vida:
Estudio clínicocontrolado aleatorizado levels in term infants atsix
months of life: A randomized, controlled trial. Arch Argent Pediatr
2010;108:201-8.
11. Chaparro CM, Neufeld LM, Tena AG, Eguia-Líz CR,
Dewey KG. Effect of timing of umbilical cord clamping on iron status in
Mexican infants: a randomized controlled trial. Lancet,
2006;367:1997-2004.
12. Geethanath RM, Ramji S, Thirupuram S, Rao YN.
Effect of timing of cord clamping on the iron status of infants at 3
months. Indian Pediatr. 1997;34:103-6.
13. Li N, Yang LC, Wu Q, Han CC, Wang L, Rong L,
et al. The effects of iron stores and growth of delayed umbilical
cord clamp timing on term breastfed infants at 4 months. Zhonghua Yu
Fang Yi Xue Za Zhi. 2012;46:303-6.
14. Nesheli H, Esmailzadeh S, Haghshenas M, Bijani A,
Moghaddams T. Effect of late vs early clamping of the umbilical
cord (on haemoglobin level) in full-term neonates. J Pak Med Assoc.
2014;64:1303-05.
15. Venâncio SI, Levy RB, Saldiva SR, Mondini L,
Alves MC, Leung SL. Effects of delayed cord clamping on hemoglobin and
ferritin levels in infants at three months of age. Cad Saude Publica,
2008;24:S323-31.
16. Rheenen P, Moor L, Eschbach S, Grooth H, Brabin
B. Delayed cord clamping and haemoglobin levels in infancy: A randomised
controlled trial in term babies. Trop Med Int Health, 2007;12:603-16.
17. Gupta R, Ramji S. Effect of delayed cord clamping
on iron stores in infants born to anemic mothers: A randomized
controlled trial. Indian Pediatr. 2002;39:130-5.
18. Grajeda R, Pérez-Escamilla R, Dewey K. Delayed
clamping of the umbilical cord improves hematologic status of Guatemalan
infants at 2 mo of age. Am J Clin Nutr, 1997;65:425-31.
19. Andersson O, Domellof M, Andersson D, Hellstrom-Westas L. Effect
of delayed vs early umbilical cord clamping on iron status and
neurodevelopment at age 12 months: A randomized clinical trial. JAMA
Pediatr. 2014;168:547-54.
|
|
|
 |
|

