Toddlers and even infants, while enjoying their
newfound freedom of movement are frequently at risk of accidental injury
caused by household items. We report a young boy who accidentally
aspirated and was severely asphyxiated by aspiration of a massive amount
of ‘kolam’ (limestone) powder used commonly in Tamilnadu for drawing
floral and other designs on the space leading to their house.
Case report
An 18-month-old male child accidentally tripped and
fell backwards while running carrying a bag containing nearly ½ kg of
kolam powder. The contents of the bag fell heaped on his nose and face,
he became unresponsive and was unable to breathe for a few seconds.
Choking cough, labored noisy respirations, vomiting and cyanosis
followed. He did not develop any seizures. He was brought to the
emergency department of our hospital three hours after the aspiration.
On examination, he was a well nourished child, had
central cyanosis and gasping, irregular respirations. He had severe
supra-sternal and intercostal retractions. There was no stridor. The
chest was hyperinflated and silent bilaterally on auscultation. He was
drowsy but arousable with a Glasgow coma scale of 11/15. His heart rate
was 160 per minute, respiratory rate 36 per minute, and blood pressure
was 82/60 mmHg.
He was intubated and endotracheal suction performed
to remove frothy secretions containing chalky white powder. Stomach wash
was given with saline. He was mechanically ventilated while awaiting
bronchoscopy. Despite high peak inspiratory airway pressures, feeble
breath sounds were heard anteriorly with no breath sounds posteriorly. A
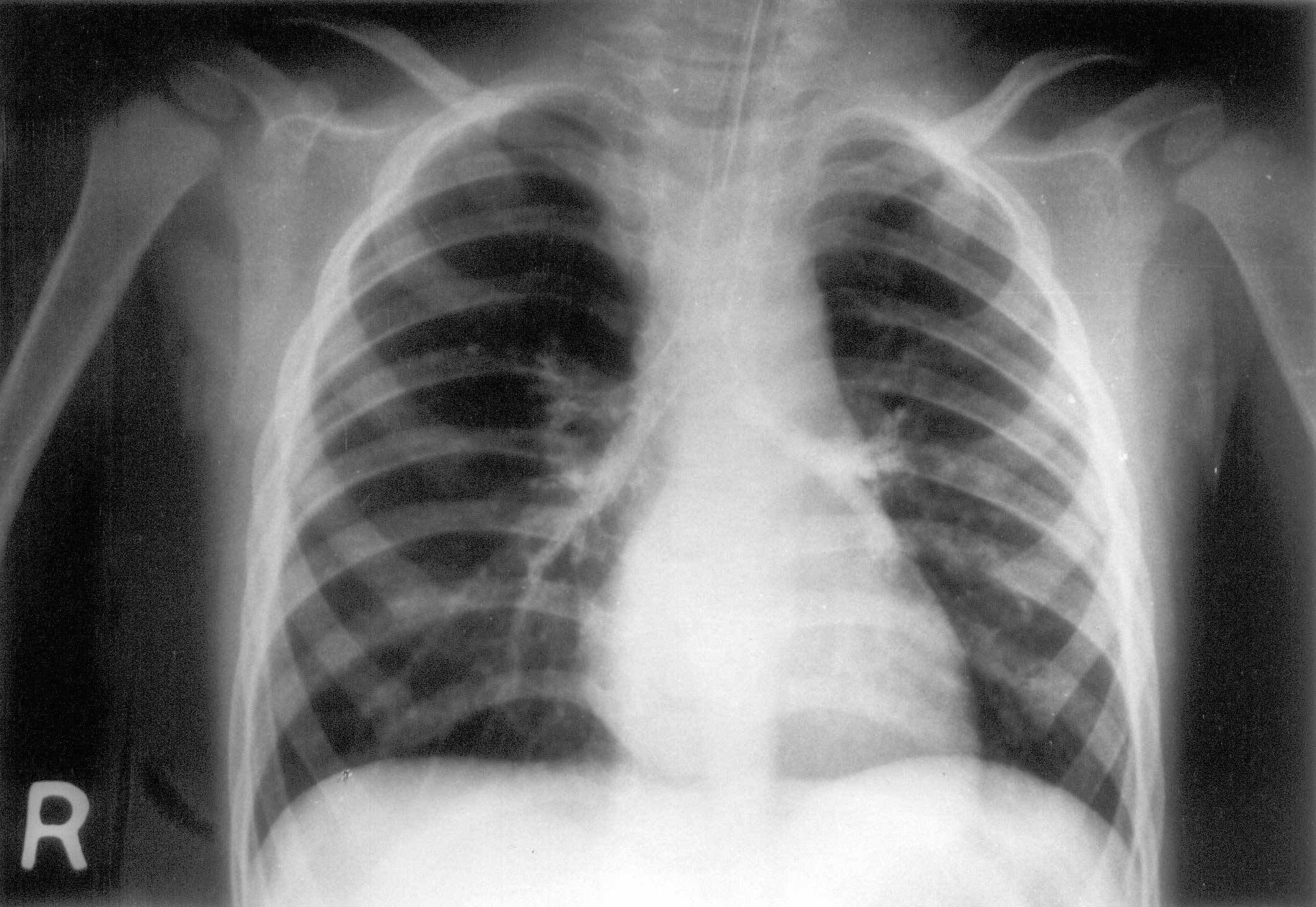
chest X-ray resembled a bronchogram with the trachea and bronchi
being clearly outlined by the calcium content of the inhaled powder (Fig.
1). He was given nebulised terbutaline, intravenous amino-phylline
infusion 0.6 mg/kg/h, 10 mg/kg of hydrocortisone bolus and subsequently
10 mg/kg/day in four divided doses. Parenteral cefotaxime and
metronidazole were also administered.
 |
|
Fig. 1. Chest X-ray following powder
aspiration. |
Bronchoscopy done 30 minutes after admission using a
rigid bronchoscope yielded inhaled kolam powder in the trachea and both
major bronchi. There was edema and redness of the bronchial mucosa. The
bulk of the aspirated chalky material was removed by bronchial lavage
with normal saline and suction using a wide bore suction catheter. The
remaining clumps sticking to the bronchial walls were removed with an
extraction forceps. Two mL of adrenaline 1:2,00,000 dilution was
instilled locally in each major bronchus and trachea to reduce post-bronchoscopic
bleeding and reactive bronchospasm.
Following bronchoscopic lavage, the patient was
ventilated mechanically for 15 hours during which period chest physiotherapy
followed by endotracheal suctioning was carried out every 15 minutes.
The air entry in the lower lobes improved signi-ficantly following the
bronchoscopy and later he showed clinical improvement. Serial arterial
blood gas estimation revealed moderate metabolic acidosis that resolved
within a few hours of mechanical ventilation. Repeat skiagram six hours
after bronchoscopy showed evidence of bronchiolar obstruction with
perihilar flaring. He was weaned off oxygen over the next 24 hours and
discharged on the fourth day. Biochemical analysis confirmed the
aspirated powder to be calcium carbonate.
At discharge, the child had regular respirations at a
rate of 38 per minute with no chest recession or hyperinflation and
vesicular breath sounds were audible equally. On follow-up at two and
six weeks after discharge, he was asymptomatic with no recurrence of
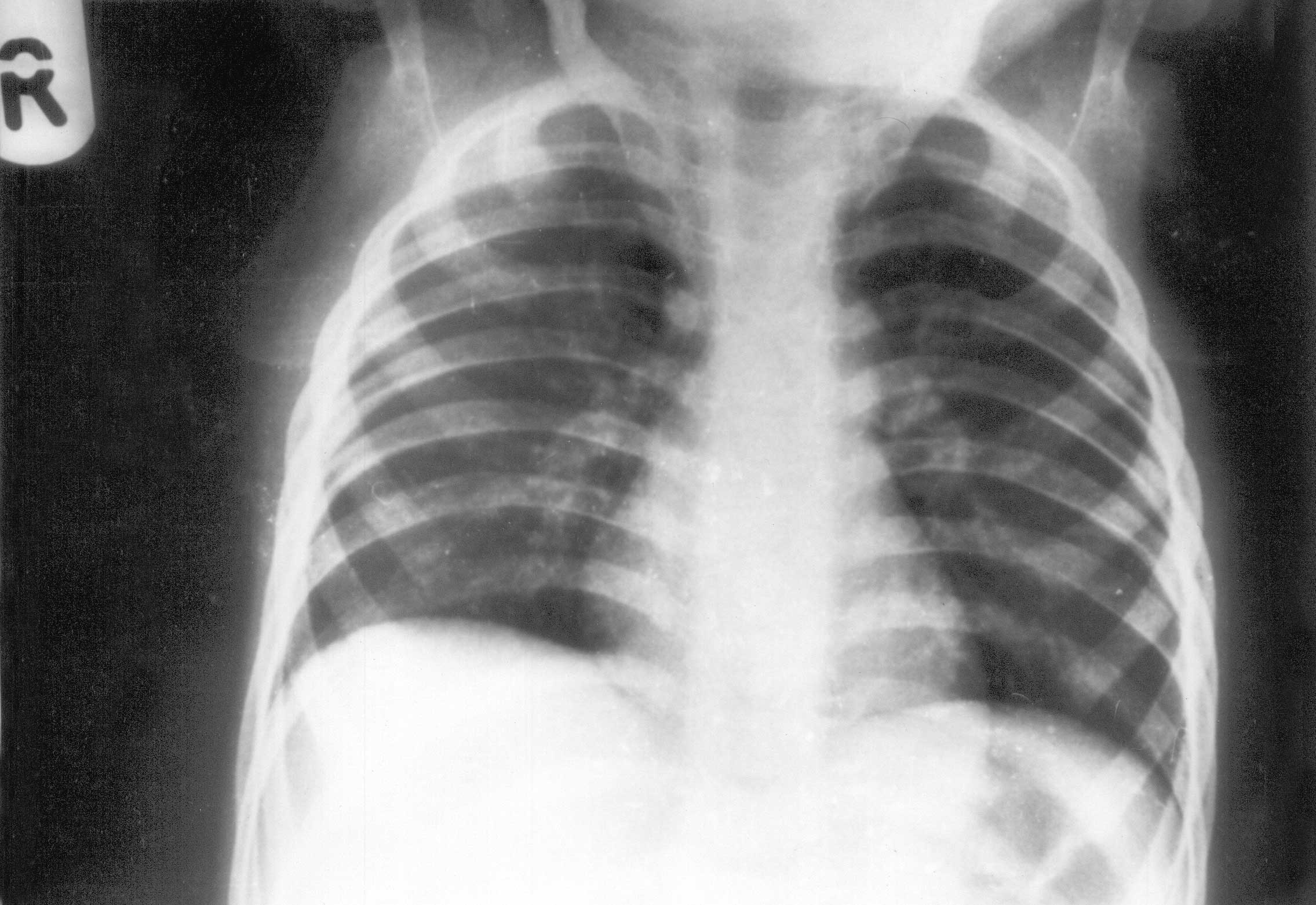
respiratory distress. The chest radiograph at discharge and at follow-up
(Fig. 2) showed normal lung markings. His serum calcium was 9.4
mg/dL, serum phosphorus was 5.8 mg/dl and serum alkaline phosphatase was
313 U/L at follow up. Ultrasound abdomen showed no evidence of
nephrocalcinosis or urinary tract lithiasis and urinary spot calcium/creatinine
ratio was 0.173.
 |
|
Fig. 2. Chest X-ray 3 weeks after discharge. |
Discussion
Accidental aspiration of food objects such as nuts
and seeds are common in young children and may result in death if not
promptly removed. Inedible objects such as balloons(1), coins, pills,
sticks, safety pins, ball bearings, metallic objects, marbles, and baby
powder may also be fatally aspirated.
Though aspiration of ‘kolam’ powder is uncommon,
there are reports of massive talcum powder aspiration from the
West(2-4). Consequences of massive powder aspiration vary from being
asymptomatic to more severe complications such as mild to severe
aspiration pneumonia(2), adult respiratory distress syndrome(5), severe
bronchiolar obstruction, massive bronchitis with pulmonary edema,
atelectasis and compensatory emphysema, acute respiratory
insufficiency/failure needing tracheotomy and mechanical ventilation(4),
progressive diffuse pulmonary fibrosis(3), and increased mortality
(23%). Outcome and prognosis depend on the time interval between the
occurrence of the accident and the hospitalization of the child or
institution of appropriate mode of therapy(4).
Calcium carbonate is insoluble in water, but absorbs
water and tends to form thick flakes on mixing with water(6). This
probably resulted in difficulty in clearing the aspirated material from
the airways in our patient .
An important point to note is that there is usually a
characteristic silent period of several hours between the initial event
of powder aspiration and onset of severe respiratory distress. This
asymptomatic period can lead to wrong parental and medical decisions
resulting in increased morbidity and mortality. The best results in
treatment are obtained by immediate intubation and bronchial wash even
in the absence of respiratory symptoms. Artificial ventilation may be
necessary to overcome very high airway resistance as encountered in our
patient. Corticosteroids and bronchodilators may be helpful(4).
Acknowledgement
We thank Dr. Geethanjali A., Department of Clinical
Biochemistry, Christian Medical College Hospital, Vellore, for the
chemical analysis of the aspirated powder.
Contributors: ACP was involved in the care of
this patient and drafted the report, under the supervision of R P. GT
did the bronchoscopy. SGV evaluated serial radiographs and provided the
illustrations.
Funding: None.
Competing interests: None stated.
