|
|
|
Indian Pediatr 2016;53:
1099-1101 |
 |
A Novel Truncation
Mutation in ATP8B1 Gene in Progressive Familial
Intrahepatic Cholestasis
|
|
Anjali Sharma, #Ujjal
Poddar, $Shikha
Agnihotry and Rakesh Aggarwal
From Department of Gastroenterology, #Department
of Pediatric Gastroenterology, and $Biomedical
Informatics Centre,
Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow,
India.
Correspondence to: Dr Rakesh Aggarwal, Department of
Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical
Sciences, Lucknow 226 014, Uttar Pradesh, India
Received: February 15, 2016;
Initial review: May 03, 2016;
Accepted: July 13, 2016.
|
Background: Progressive familial intrahepatic cholestasis has
been only infrequently reported from India. Case characteristics:
An Indian girl with progressive cholestatic liver disease beginning
during infancy, normal gamma-glutamyl transpeptidase levels, parental
consanguinity, positive family history and a fatal outcome.
Observation: A novel, homozygous mutation
(c.[589_592inv;592_593insA]) in ATP8B1 gene, with a markedly
truncated protein (p.[Gly197LeufsTer10]) was found. Message: The
novel mutation found expands the spectrum of genetic variations
associated with progressive familial intrahepatic cholestasis.
Keywords: Diagnosis, Genetic variation, Neonatal cholestasis,
Protein truncation.
|
|
P
rogressive familial intrahepatic cholestasis
(PFIC), a genetic disorder, accounts for 10%-15% of cholestatic liver
disease in children [1]. The condition is classified into three types,
namely PFIC1, PFIC2 and PFIC3, related to mutations in ATP8B1
gene, ABCB11 gene and ABCB4 gene, respectively [2-4].
PFIC1 and PFIC2 manifest during infancy and progress to end-stage liver
disease during early childhood, whereas the onset of PFIC3 is often
delayed. Despite some phenotypic differences, differentiation is based
primarily on genetic findings.
Some individual cases [5,6] and small case series
[7,8] of suspected PFIC have been reported from India, but there are no
data on genetic variations in this disease.
Case Report
A 4.5-month-old girl, born at term to second-degree
consanguineous parents, presented with jaundice and pruritus for one
month. She was fourth in birth order with one intrauterine death, a
8-year-old healthy sister, and one sister who had died at 5 years of age
of decompensated liver disease (which began with jaundice and pruritus
at 3 months of age). The mother reported intense itching during third
trimester in each pregnancy.
At presentation, she weighed 5.5 kg (5 th-10th
centile), was 59 cm long (10th-25th
centile), and had mild icterus and a soft liver palpable 3 cm below the
costal margin. Conjugated hyperbilirubinemia (total serum bilirubin 7.0
mg/dL, conjugated 5.0 mg/dL), high alkaline phosphatase (630 U/L;
reference range for adults 35-150) normal serum alanine and aspartate
aminotransferases, and low-normal GGT activity (8 U/L) were seen. Serum
albumin level (3.7 g/dL) and prothrombin time (international normalized
ratio = 1.1) were normal. Facility for serum bile acid levels was not
available. Ultrasonography showed normal biliary system. Percutaneous
liver biopsy showed maintained lobular architecture, minimal portal
inflammation and bland cholestasis; immunohistochemistry was not done.
In view of cholestasis with normal GGT, family history of similar
illness, history of cholestasis during pregnancy in the mother, and
consanguinity, a diagnosis of PFIC was made.
Treatment with ursodeoxycholic acid, rifampicin and
cholestyramine, vitamin supplementation, and diet rich in medium-chain
triglycerides did not provide any symptomatic improvement. The parents
declined surgical treatment. Over time, her disease worsened, ascites
and coagulopathy appeared, and serum albumin levels declined. She died
at home at the age of 4 years, with worsening ascites and
encephalopathy.
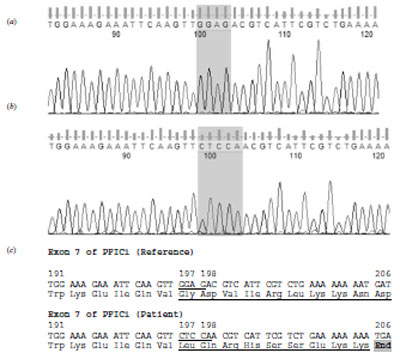
All the coding exons of ATP8B1, ABCB11 and
ABCB4 genes were amplified [2-4] and sequenced. This revealed a
novel, homozygous variation in exon 7 of the ATP8B1 gene
(c.[589_592inv;592_593insA]; Fig. 1a-b), with
replacement of a 4-nucleotide sequence (GGAG) by five nucleotides CTCCA.
It was predicted to lead to a truncated protein with 205 amino acid
instead of a normal protein with 1251 amino acids (Fig. 1c).
The ABCB11 gene also showed a non-synonymous variation in exon 13
(c.1331T>C; rs2287622), which was predicted as unlikely to adversely
affect the protein function (http://snps.biofold.org/meta-snp/index.html).
 |
|
Fig. 1 Sequencing chromatograms from a
part of exon 7 of ATP8B1 gene from a healthy person showing the
reference sequence (a) identical to GenBank accession number
NM_005603.4): and our patient (b) show a c.589_592inv;
592_593insA change. This genomic change leads to a frame shift
with a change in the amino acid sequence and premature
truncation of the protein after amino acid location 205).
Underlining indicates the nucleotides and amino acids that have
changed (c).
|
In addition, there were some previously-known
synonymous variations in the ATP8B1 (c.696T>C [rs319438] and
c.811A>C [rs319443]), ABCB11 (c.3084A>G [rs497692]) and ABCB4
(c.711A>T [rs2109505]) genes. Both the parents had the
c.[589_592inv;592_593insA] frame-shift variation in heterozygous state.
Discussion
This report describes an Indian child who had liver
disease starting in infancy, with clinical features typical of PFIC, and
a strong family history of liver disease. Normal GGT levels indicated
that PFIC3 was unlikely. However, in the absence of extrahepatic
features, it was not possible to distinguish whether she had PFIC1 or
PFIC2. The detection of a major mutation in exon 7 of the ATP8B1
gene, which was expected to severely disrupt the structure of this
gene’s product confirmed that this patient had PFIC1.
Data on PFIC from India are limited [5-8]; there are
no published data from other South Asian countries. Genetic
abnormalities underlying this disease have not been studied. In our
patient, we did consider the possibility of biliary diversion and liver
transplantation. In the literature, symptomatic relief after biliary
diversion has been observed in only a subset of patients, and its
occurrence cannot be predicted in advance [1]. In PFIC1, though liver
transplantation reliably reverses cholestasis, other extrahepatic
manifestations, such as diarrhea and hepatic steatosis may worsen or
appear when not already present, by permitting a larger amount of bile
salts to reach the gut [9]; short stature also does not respond. In
PFIC2 patients with severe disease who need transplantation, the
procedure is often complicated by disease recurrence; this is believed
to be related to development of antibodies to the PFIC2 protein present
in the transplanted organ [10].
In our patient, we were able to show the presence of
a novel mutation in the ATP8B1 gene. This gene encodes a
1251-amino acid long protein which is involved in the transport of
aminophospholipids across cellular membranes. Several mutations in this
gene have been described, including non-sense mutations that alter the
amino acid sequence of the protein, small insertion or deletion
mutations that induce frameshifts, in-frame deletions of variable size,
and mutations that may disrupt splicing [2]. Genotype-phenotype
correlation shows that missense mutations are more common in a condition
known as benign recurrent intrahepatic cholestasis, a mild disease,
whereas nonsense, frame-shift, and large deletion mutations are more
common in patients with PFIC [2]. The novel mutation found in our
patient led to a markedly truncated protein which would lack the active
domain and hence be non-functional; this may explain the severe disease
in this kindred.
Genetic analysis in PFIC is important for accurate
diagnosis and possibility of prenatal diagnosis during subsequent
pregnancies in the family. Such analyses, by providing information on
mutations prevalent in Indian patients with PFIC, may permit a directed
testing for the common mutations rather than using sequencing for
several exons.
Acknowledgement: Our sequencing facility is
supported by FIST Program, Department of Science and Technology,
Government of India, and the Biomedical Informatics Centre is supported
by the Indian Council of Medical Research (ICMR), New Delhi.
Contributors: AS: did the laboratory work
and data analysis; SA: did the bioinformatic analysis; UP: was involved
in clinical work up of the patient; RA: conceived the work, supervised
laboratory work and data analysis, and will be the guarantor. All the
authors were involved in planning of this work, writing of the report,
and approval of the final version of the manuscript.
Funding: During this work, AS and SA were
supported by ICMR. Competing interests: None stated.
References
1. Davit-Spraul A, Gonzales E, Baussan C, Jacquemin
E. Progressive familial intrahepatic cholestasis. Orphanet J Rare Dis.
2009;4:1.
2. Klomp LW, Vargas JC, van Mil SW, Pawlikowska L,
Strautnieks SS, van Eijk MJ, et al. Characterization of mutations
in ATP8B1 associated with hereditary cholestasis. Hepatology.
2004;40:27-38.
3. van Mil SW, van der Woerd WL, van der Brugge G,
Sturm E, Jansen PL, Bull LN, et al. Benign recurrent intrahepatic
cholestasis type 2 is caused by mutations in ABCB11. Gastroenterology.
2004;127:379-84.
4. Lang T, Haberl M, Jung D, Drescher A,
Schlagenhaufer R, Keil A, et al. Genetic variability, haplotype
structures, and ethnic diversity of hepatic transporters MDR3 (ABCB4)
and bile salt export pump (ABCB11). Drug Metab Dispos. 2006;34:1582-99.
5. Koshy A, Ramesh H, Mahadevan P, Francis VJ,
Chettupuzha AP, Mathew PG, et al. Progressive familial
intrahepatic cholestasis: a case with improvement in liver tests and
growth following partial external biliary diversion. Indian J
Gastroenterol. 2009;28:107-8.
6. Sharma D, Shah UH, Sibal A, Chowdhary SK.
Cholecystoappendicostomy for progressive familial intrahepatic
cholestasis. Indian Pediatr. 2010;47: 626-8.
7. Kaur S, Sharma D, Wadhwa N, Gupta S, Chowdhary SK,
Sibal A. Therapeutic interventions in progressive familial intrahepatic
cholestasis: experience from a tertiary care center in north India.
Indian J Pediatr. 2012; 79:270-3.
8. Ramachandran P, Shanmugam NP, Sinani SA, Shanmugam
V, Srinivas S, Sathiyasekaran M, et al. Outcome of partial
internal biliary diversion for intractable pruritus in children with
cholestatic liver disease. Pediatr Surg Int. 2014;30:1045-9.
9. Lykavieris P, van Mil S, Cresteil D, Fabre M,
Hadchouel M, Klomp L, et al. Progressive familial intrahepatic
cholestasis type 1 and extrahepatic features: no catch-up of stature
growth, exacerbation of diarrhea, and appearance of liver steatosis
after liver transplantation. J Hepatol. 2003;39: 447-52.
10. Keitel V, Burdelski M, Vojnisek Z, Schmitt L,
Häussinger D, Kubitz R. De novo bile salt transporter antibodies as a
possible cause of recurrent graft failure after liver transplantation: a
novel mechanism of cholestasis. Hepatology. 2009;50:510-7.
|
|
|
 |
|

