antrell syndrome is a
rare, usually lethal, congenital malformation [1]. In the
complete form, five anomalies exist, namely a midline
supra-umbilical abdominal wall defect, a sternal defect, an
anterior diaphragmatic defect, a diaphragmatic pericardial
defect and a congenital heart defect. However, the extent of
individual defects and their combination varies considerably;
broad spectrum of associated cardiac abnormalities have been
reported in most cases. We describe a neonate presenting with a
pulsatile umbilical swelling and cyanosis since birth, later
confirmed to be due to Cantrell syndrome.
A full term male neonate with uneventful
antenatal and perinatal course, born to a primigravida mother by
normal vaginal delivery, was noted to have a pulsatile umbilical
mass immediately after birth. Antenatal second trimester
sonographic scans were reported normal, but detailed anomaly
scan was not done. Baby was seen at our institute on day seven
of life. He was feeding well, had a capillary filling time <3
second and normal urine output. Examination revealed tachycardia
with a heart rate of 200 beats per minute, and central cyanosis
(oxygen saturation 85% in room air). A peculiar mass arising
from just above the umbilical stump, measuring 5×2×2 cm was
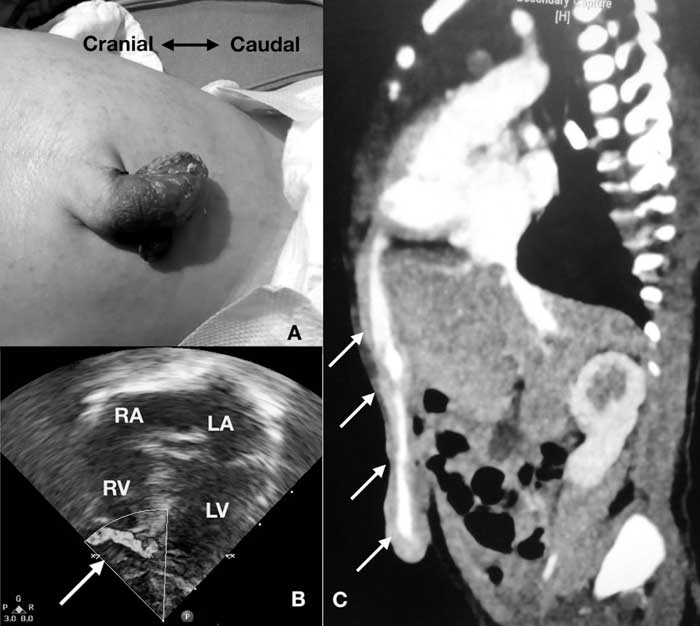
noted. The mass enlarged with each cardiac systole (Fig.
1a). It was covered with skin on its dorsal aspect but its
ventral aspect was devoid of skin. On palpation, the structure
had a forceful impulse and auscultation revealed a loud
to-and-fro murmur over the mass. Cardiovascular examination
revealed no evidence of heart failure, wide split second heart
sound with a soft pulmonic component and a grade 3/6 ejection
systolic murmur at left upper sternal border. A midline defect
was palpable in the anterior abdominal wall.
 |
|
Fig. 1 (a) Clinical
photograph of umbilical swelling; (b) echocardiogram in
four chamber view showing a vascular channel (white
arrow) arising from left ventricle apex; (c) CT
angiographic section in sagittal view showing the
abnormal vascular channel (white arrows) arising from
left ventricle apex.
|
Electrocardiogram revealed atrial flutter
with ventricular rate of 200/min. Chest radiograph showed situs
solitus, levocardia, normal sized heart and pulmonary oligemia.
Ultrasound and Doppler evaluation of the mass revealed normal
umbilical arteries, with a connection between umbilical vein and
left ventricle through falciform ligament, suggestive of left
ventricular diverticulum. Echocardiogram showed double outlet
right ventricle with infundibular pulmonary stenosis. There was
a tubular structure arising from apex of left ventricle which
had a to-and-fro Doppler flow through it (Fig. 1b).
Computed tomography (CT) angiography revealed a dilated vascular
channel beginning from the umbilical outpouching and travelling
cranially within the anterior abdominal wall and along the
falciform ligament to drain into the left ventricular apex
through a 2 mm opening. There were multiple stenosis throughout
its course, confirming the diagnosis of left ventricular
diverticulum (Fig. 1c). Defect in anterior
diaphragm was present, but there was no associated sternal
defect.
In view of atrial flutter, patient was
started on propranolol and digoxin, and good heart rate control
was achieved. After discussion with the cardiac surgical team,
it was decided to close the left ventricular diverticulum, the
cardiac lesion to be addressed later, since the oxygen
saturation of the baby stayed above 85%. Left anterolateral
thoracotomy was done and the fistulous tract arising from
anterior most part of the left ventricular apex was identified.
It was double clamped and divided and both ends were sutured.
Defect in diaphragm was closed. The umbilical swelling was
excised and the skin repaired. Patient had a smooth
post-operative course and recovered well. The cardiac rhythm
reverted to sinus rhythm on postoperative day 6. He was
discharged on ninth post-operative day. Digoxin was stopped at
six-week follow-up. Currently, at one-year follow up, baby is
doing well, his oxygen saturation is 80% and he is in sinus
rhythm. He is planned for Glenn surgery in view of non-committed
muscular VSD, and is awaiting the same.
Only 250 cases of Cantrell syndrome have been
reported in the literature [2]. It has high morbidity and
mortality, with more than half of patients dying, many despite
surgery [3]. Abnormal migration of the splanchnic and somatic
mesoderm (which affects the development of the heart and the
major vessels) with premature breakage of the chorion or
vitelline sac at about day 14 to 18 of gestation, may lead to a
mid-line defect [4] Congenital cardiac malformations are
associated in majority, ventricular septal defect is the
commonest abnormality. Association with double outlet right
ventricle has also been previously reported [5].
Over 70% of patients with left ventricular
diverticulum have Cantrell syndrome. The diverticulum originates
from the left ventricular apex in these cases and may be
associated with umbilical hernia and complex cardiac
abnormalities. Ventricular aneurysm must be differentiated from
diverticulum. A narrow mouth and synchronous contractility
characterize a diverticulum. On the other hand, aneurysms show
akinesia or paradoxic contractility of the outpouching, which is
asynchronous with the rest of heart.
Early surgical repair is indicated in cases
of left ventricular diverticulum, as it may rupture
spontaneously, thrombose or produce arrhythmias. It is generally
recommended that the midline thoraco-abdominal defect is treated
first and heart defects be corrected later [6]. We present this
case in view of the interesting presentation in a neonate with a
pulsatile umbilical swelling and cyanosis, and a good outcome
after surgery.
REFERENCES
1. Cantrell JR, Haller JA, Ravitch MM. A
syndrome of congenital defects involving the abdominal wall,
sternum, diaphragm, pericardium and heart. Surg Gynecol Obstet.
1958;107:602-14.
2. Jnah AJ, Newberry DM, England A. Pentalogy
of Cantrell: Case report with review of the literature. Adv
Neonatal Care. 2015;15:261-8.
3. O’gorman CS, Tortoriello TA, McMahon CJ.
Outcome of children with pentalogy of Cantrell following cardiac
surgery. Pediatr Cardiol. 2009;30:426-30.
4. Amato JJ, Douglas WI, Desai U, Burke S.
Ectopia cordis. Chest Surg Clin North Am. 2000;10:297-316.
5. Singh N, Bera ML, Sachdev MS, Aggarwal N,
Joshi R, Kohli V. Pentalogy of Cantrell with left ventricular
diverticulum: A case report and review of literature. Congenital
Heart Dis. 2010;5:454-7.
6. Williams AP, Marayati R, Beierle EA. Pentalogy of
Cantrell. Semin Pediatr Surg. 2019;28:106-10.

