I
mmune thrombocytopenia (ITP)
is an acquired autoimmune disease characterized by a low platelet count
(<100,000/mm3) due to
‘antibody mediated’ destruction of platelets and impaired mega-karyopoiesis
with peak incidence in 2-5 years old [1]. Despite being the commonest
cause of thrombocytopenia in children, there have been more
controversies than consensus in its diagnosis and management. The
American Society of Hematology first published guidelines on ITP in 1996
with updates published in 2011 and now in December, 2019 to answer the
relevant questions in wake of new available evidence. The highlights of
the latest update are listed in Table I. The definitions
of ‘grades of recommendation’ may be referred to in the respective
guidelines [1,2]
|
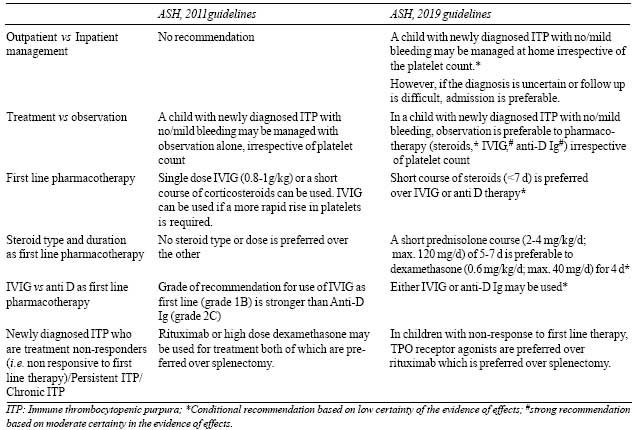
Table I Highlights of Updates From the
Previous ASH, 2011 and Current ASH, 2019 ITP Guidelines
|
 |
ITP is termed acute/newly diagnosed, if lasting less
than 3 months; persistent, if lasting 3-12 months, and chronic, if
persisting beyond 12 months. Majority of children (60-75%) have acute
ITP that resolves within 2-3 months of diagnosis, regardless of therapy.
ITP may be primary (where no cause is found) or secondary to other
conditions like infections (HIV, Hepatitis C, H. pylori),
autoimmune syndromes (SLE, APLA syndrome), primary immunodeficiency
(common variable immune-deficiency i.e. CVID) and drugs (valproate,
heparin). As per the latest ASH 2019 guidelines, routine testing for
bone marrow aspirate/bone marrow biopsy (Grade 1B), anti-nuclear
antibody (grade 2C) and H. pylori (grade 2C) is not recommended
unless there are clinical pointers. The utility of screening all ITP
patients for CVID, hepatitis C, HIV and Hepatitis B is still unclear
[1]. Thrombocytopenic syndromes (like Wiskott–Aldrich syndrome) and CVID
are important masqueraders of immune thrombocytopenia. While a detailed
family history and a meticulous examination may diagnose these mimickers
at outset, at times these syndromes are recognized later in cases
mislabelled as ITP, who fail to respond to all therapy [3].
Clinically, ITP is characterized by bleeding events
that show no linear correlation with the severity of thrombocytopenia
[4]. Most of children (62-74%) with ITP spontaneously remit within a
year [5]. Therefore, the decision regarding use of platelet enhancing
therapy should be based on multiple factors (access to care, patient and
provider preferences, risk of bleeding, duration of disease,
co-morbidities and age at presentation). In newly diagnosed ITP with
no/mild bleeding, the ASH 2019 guidelines recommend observation over
treatment irrespective of the platelet count. Moreover, they suggest
observation at home is preferable to hospital admission. However, they
add that if a decision to observe on outpatient basis is made, it is
desirable for the patient to be seen by a pediatrician within 24-72
hours [2]. In those set-ups, where patient follow-up is uncertain due to
social/financial concerns or residence is in remote areas which are far
from hospitals, admission to the hospital and treatment is preferable.
Similar recommendations have been stated by the Joint working group
(JWG) of several European hematology societies (Germany, Austria, and
Switzerland) published in 2018, wherein special emphasis has been placed
on the patient’s choice of therapy [6].
Minimizing the risk of hemorrhage and decreasing the
long-term side effects of treatment are the goals of therapy. Treatment
is guided by the severity of bleeding rather than on the platelet count.
The ASH 2019 guidelines have defined major bleeding as any one of the
following (i) WHO grade 3 or 4 bleeding, (ii) Buchanan
severe grade, (iii) Bolton-Maggs and Moon major bleeding, (iv)
IBLS grade 2 or higher, or (v) life-threatening bleeding or
intracerebral hemorrhage. Minor bleeding is any bleeding not meeting the
criteria for major bleeding. Adolescents with ITP are treated as per
pediatric guidelines [1].
Acute/newly diagnosed ITP: In a child with newly
diagnosed ITP with no/mild bleeding, ASH continues to recommend
observation over pharmacotherapy irrespective of the platelet count.
However, in a child with moderate to severe bleeding and/or a diminished
health related quality of life, a short course of corticosteroids (<7
days) is preferred over intravenous immunoglobulin (IVIG) or anti-D
immunoglobulin (anti-D Ig) therapy [2]. A short prednisolone course (2-4
mg/kg/day; maximum 120 mg/day) of 5-7 days is preferable to
dexamethasone (0.6 mg/kg/day; maximum 40 mg/day) for 4 days. The
European joint working group (JWG) has also endorsed a shorter course of
steroids less than 2 weeks, without specifying the preferred type of
steroid [6]. ASH 2019 states that as per limited available data IVIG and
anti-D Ig have similar benefits, and both are associated with rare but
potential black box warnings. Thus, either of them may be used. In
practice, the choice between the three available treatments is usually
guided by cost, availability and adverse effects [7].
Persistent ITP: If treatment with steroids, IVIG
or anti-D Ig has been successful, these options may be used to prevent
bleeding as needed, especially in the first 12 months of diagnosis when
the possibility of spontaneous remission is high [1].
Chronic ITP: In children with "newly diagnosed"
ITP or persistent ITP with non-response to first line pharmacotherapy or
those with chronic ITP, second line pharmacotherapy is suggested wherein
thrombopoietin receptor agonists (TPO-RAs) (romiplostim, eltrombopag
etc.) are preferred over rituximab. This is premised on acceptable
response to TPO-RA with low side effects and avoidance of
immunosuppression. Similar views were given by the European JWG [6].
Other treatment options include high dose dexamethasone (0.6 mg/kg/d for
4 days every 4 weeks for 6 cycles) [1]. Use of alternate
immunosuppressive agents (dapsone, azathioprine, danazol, mycophenolate
mofetil, cyclosporine, cyclophosphamide, anti-CD52 monoclonal antibody,
vinca alkaloids) and combination of different agents has been tried but
data are sparse and hence ASH 2019 categorically mentions that
recommendations were not feasible. Splenectomy should be deferred, if
possible, to beyond 12 months from disease onset. It may be the last
resort in situations where ITP is unresponsive to all other therapy, the
child shows intolerance to other drugs and quality of life is impaired.
These recommendations are in concurrence with those of the European JWG
[6].
In the Indian scenario, the cost and availability of
TPO-RAs is prohibitive which makes them unsuitable as a frontline
therapy [7]. Rituximab is promising with a median response duration of
12.8 months, relative ease of availability and tolerable side effects
[8]. In cases where there is non-response to rituximab or availability
is an issue, high dose dexamethasone and dapsone have been used as
alternatives. Although high dose steroids have a good efficacy, their
long-term use is associated with significant adverse effects. Dapsone is
an easily available low-cost drug with response rates of around 50%;
hemolysis and methemoglobinemia being important side effects and to be
avoided in G6PD deficient individuals [9].
Secondary ITP: Treatment is directed towards the
underlying cause [1]. Withdrawal of the causative drug results in
remission of drug-induced ITP. ASH 2019 reiterates that children with
ITP should receive first MMR vaccine per routine schedule (grade1B).
Those who have already received MMR previously can get a vaccine titre
done to assess need for booster dose [1]. A summary of available
treatment options is given in Table II.
|
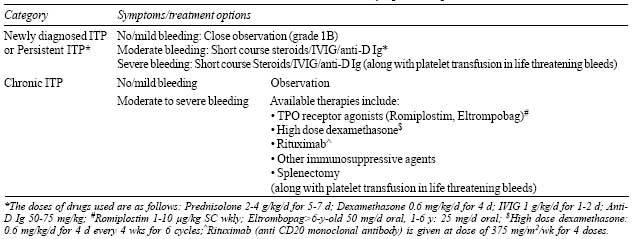
Table II Treatment of Immune Thrombocytopenic
Purpura
|
 |
Assessment of response to treatment: The
International working group provides specific recommendations for
assessing the response to ITP treatments [10]. Although not based on
evidence, these thresholds provide a useful standardization that will
allow better comparison of responses between studies and the ASH 2019
endorses the same.
Contributors: PKS and JC: conceptualized and
drafted the manuscript; JC: critically appraised the manuscript.
Funding: None; Competing interests: None
stated.
REFERENCES
1. Neunert C, Lim W, Crowther M, Cohen A, Solberg L
Jr, Crowther MA; American Society of Hematology. The American Society of
Hematology 2011 evidence-based practice guideline for immune
thrombocytopenia. Blood. 2011;117:4190-207.
2. Neunert C, Terrell DR, Donald M. Arnold DM,
Buchanan G, Cines DB, Cooper N, et al. American Society of
Hematology 2019 Guidelines for Immune Thrombo-cytopenia. Blood
Adv. 2019;3:3829-66.
3. Bryant N, Watts R. Thrombocytopenic syndromes
masquerading as childhood immune thrombocytopenic purpura. Clin Pediatr
(Phila). 2011;50:225-30.
4. Neunert C, Noroozi N, Norman G, Buchanan GR, Goy
J, Nazi I, et al. Severe bleeding events in adults and children
with primary immune thrombocytopenia: A systematic review. J Thromb
Haemost. 2015;13:457-64.
5. Bennett CM, Neunert C, Grace RF, Buchanan G,
Imbach P, Vesely SK, et al. Predictors of remission in children
with newly diagnosed immune thrombocytopenia: Data from the
Intercontinental Cooperative ITP Study Group Registry II participants.
Pediatr Blood Cancer. 2018;65:.
6. Matzdorff A, Meyer O, Ostermann H, et al.
Immune Thrombocytopenia - Current Diagnostics and Therapy:
Recommendations of a Joint Working Group of DGHO, OGHO, SGH, GPOH, and
DGTI.¨ Oncol Res Treat. 2018;41:1-30.
7. Liang Y, Zhang L, Gao J, Hu D, Ai Y. Rituximab for
children with immune thrombocytopenia: A systematic review. PLoS One.
2012;7:e36698
8. Patel AP, Patil AS. Dapsone for immune
thrombocytopenic purpura in children and adults. Platelets.
2015;26:164-7
9. Rodeghiero F, Stasi R, Gernsheimer T, Micheal M,
Provan D, Arnold DM, et al. Standardization of Terminology,
Definitions and Outcome Criteria in Immune Thrombocytopenic Purpura of
Adults and Children: Report from an International Working Group. Blood.
2009;113:2386-93.

