|
|
|
Indian Pediatr 2020;57:
975-976 |
 |
NeoBox - A Multipurpose Aerosol Box for Neonatal Care
DuringCOVID-19 Pandemic
|
|
Shilpa Kalane, 1*
Niranjan Khambete2
and Rajan Joshi3
Departments of 1Neonatology and 3Pediatrics,
and 2Clinical Eningeering,
DeenanathMangeshkar Hospital, Pune 411004,
Maharashtra, India.
Email:
[email protected]
Published Online: August 10, 2020;
PII: S097475591600228.
|
Safety of the newborn and the protection
of healthcare workers (HCWs) from aerosol exposure are
extremely important during the current severe acute
respiratory illness coronavirus 2 (SARS-CoV-2) pandemic. Use
of personal protective equipment (PPE) has been shown to be
associated with a reduced risk of infection [1]. As per WHO
guidelines, it is mandatory to use personal protective
equipment (PPE) while performing aerosol-generating
procedures like suction, intubation, chest compression
etc. [2,3]. However, despite the use of PPE,
there remains a possibility that aerosols can contaminate
nearby surfaces [4]. An aerosol box acts as a
physical barrier against the aerosol spread [4,5]. PPE with
a barrier enclosure like an aerosol box can be an effective
measure to minimize aerosol spread and exposure during this
pandemic [2,4].
Recent literature reports that when an
aerosol box was used for airway management, the inner
surface of the box and the laryngoscopist’s gloves and
gowned forearms were observed to be contaminated [4], but no
macroscopic contamination outside the box was observed [4].
Unlike adult resuscitation, the focus of newborn
resuscitation is effective ventilation of baby’s lungs which
includes aerosol-generating procedures like suction, PPV,
using continuous positive airway pressure, intubation, chest
compression, etc. [6,4]. To see the feasibility of using the
standard aerosol box as a barrier enclosure while performing
aerosol-generating procedures on neonates, a novel
simulation session integrating a newborn delivery of a
suspect or confirmed COVID-19 mother with a subsequent need
for neonatal resuscitation was developed. The 15-minute
simulation was run with two resident doctors, an embedded
simulation nurse, and a low fidelity manikin in the delivery
room setting. The ‘newborn’ was a low fidelity simulator (Laerdal
Medical). During simulation sessions, accessing the neonate
and performing resuscitation steps in the squared aerosol
box was observed to be impossible. After completion of each
session, the learners were debriefed using the PEARLS
Healthcare Debriefing Tool with plus/delta and advocacy
enquiry format by a trained simulation leader [8,9].
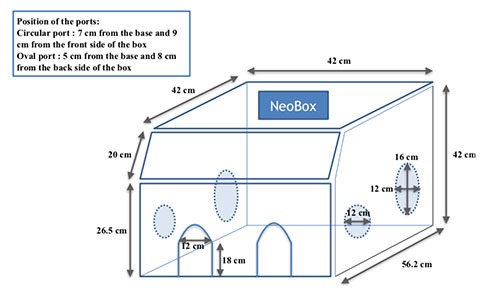
Difficulties were encountered at all steps of resuscitation
like - attaching pulse oximeter, performing positive
pressure ventilation, intubation, chest compression and
umbilical catheterization, etc. These difficulties were
addressed and the need for a modified aerosol box for
neonates was informed to the biomedical department of our
institute. The box underwent multiple modifications based on
the feedbacks received. The final design specifications were
given (Web Table I) and the NeoBox was
developed (Fig.1).
 |
|
Fig. 1 NeoBox with
dimensions.
|
 |
|
Fig.2 NeoBox in delivery
room – resuscitator managing airway.
|
The NeoBox is made up of a transparent
polycarbonate (3 mm thick). The material required was
procured and necessary fabrications were done by the local
acrylic / polycarbonate sheet fabricator. The average time
required to make one NeoBox was approximately 4 hours. The
cost was Rs 6500. An alcohol based disinfectant (Ethanol
70%) with a contact time of minimum 1 minute is used to
clean the NeoBox [10].
The NeoBox was primarily designed as a
physical barrier to prevent aerosol exposure and spread
while performing aerosol-generating procedures during
resuscitation in delivery room. While running simulation
sessions, its wider application for neonatal care like
transporting a suspected or confirmed COVID-19 neonate from
one place to another (intra hospital transport) and caring
for them in the neonatal intensive care unit (NICU) while
performing aerosol-generating procedures was recognized. Use
of NeoBox in addition to PPE helped boosting HCWs confidence
for managing suspected or confirmed COVID-19 neonates. We
found that the NeoBox would require training before use in
the treatment of patients. Wearing PPE is must for HCWs
while performing aerosol-generating procedures in a
suspected or confirmed COVID-19 neonate. NeoBox works as a
physical barrier to prevent aerosol spread. However, in case
of difficulty it is advised to remove the NeoBox and perform
intubation.
We propose the NeoBox as an additional
protection, and suggest that it may be considered to be an
adjunct to standard PPE for managing suspected COVID-19
newborns in delivery room (Fig. 2). It can
also be used as a barrier enclosure during intrahospital
transport and while performing aerosol-generating procedures
in the NICU.
Acknowledgment: Dr Vaibhavi Upadhye,
DrArti Rajhans and DrDhananjay Kelkar from Deenanath
Mangeshkar Hospital for their support and guidance.
REFERENCES
1. Chou R, Dana T, Buckley DI, Selph S,
Fu R, Totten AM. Epidemiology of and risk factors for
coronavirus infection in health care workers: A living rapid
review. Ann Intern Med. 2020;173:120-36.
2. World Health Organization. Infection
Prevention and Control During Health Care When COVID-19 is
Suspected: Interim Guidance. 19 March 2020. Available from:
https://www.who.int/publications-detail/
infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125.
Accessed May 23, 2020.
3. Harding H, Broom A, Broom J. Aerosol
generating procedures and infective risk to healthcare
workers: SARS-CoV-2 - the limits of the evidence. J Hosp
Infect. 2020;105:717-25. Epub ahead of print.
4. Canelli R, Connor CW, Gonzalez M,
Nozari A, Ortega R. Barrier enclosure during endotracheal
intubation. N Engl J Med. 2020;382:1957 8.
5. Motara F, Laher AE, Du Plessis J,
Moolla M. The "Intubox": Enhancing Frontline Healthcare
Worker Safety During Coronavirus Disease 2019 (COVID-19).
Cureus. 2020;12:e8530.
6. Chandrasekharan P, Vento M,
Trevisanuto D, Partridge E, Underwood MA, Wiedeman J, et
al. Neonatal resuscitation and postresuscitation care of
infants born to mothers with suspected or confirmed
SARS-CoV-2 infection. Am J Perinatol 2020;37:e3-e3.
7. Edelson DP, Sasson C, Chan PS, Atkins
DL, Aziz K, Becker LB, et al. American Heart Association ECC
Interim COVID Guidance Authors. Interim Guidance for Basic
and Advanced Life Support in Adults, Children, and Neonates
With Suspected or Confirmed COVID-19: From the Emergency
Cardiovascular Care Committee and Get With The
Guidelines-Resuscitation Adult and Pediatric Task Forces of
the American Heart Association. Circulation.
2020;141:e933-43.
8. Bajaj K, Meguerdichian M, Thoma B,
Huang S, Eppich W, Cheng A. The PEARLS healthcare debriefing
tool. Acad Med. 2018;93:336.
9. Rudolph JW, Simon R, Rivard P,
Dufresne RL, Raemer DB. Debriefing with good judgment:
Combining rigorous feedback with genuine inquiry.
Anesthesiol Clin. 2007;25:361 76.
10. World Health organization. Cleaning and Disinfection
of Environmental Surfaces in the Context of COVID-19.https://www.who.int/publications-detail/cleaning-and-disinfection-of-environmental-surfaces-inthe-context-of-covid-19.
Accessed May 23, 2020.
|
|
|
 |
|

