|
|
|
Indian Pediatr 2020;57: 959-962 |
 |
Identification, Evaluation, and Management of Children With
Autism Spectrum Disorder: American Academy of Pediatrics 2020
Clinical Guidelines
|
Sharmila Banerjee Mukherjee
From Department of Pediatrics, Kalawati Saran Children’s
Hospital, New Delhi, India.
Correspondence to:Dr. Sharmila B. Mukherjee, Department
of Pediatrics, Kalawati Saran Children’s Hospital, New
Delhi. India.
Email:
[email protected]
|
|
The American Academy of
Pediatrics recently published clinical guidelines for
evaluation and management of children and adolescents with
Autism Spectrum Disorder (ASD), nearly 12 years after the
previous version. This article outlines salient features,
highlights significant differences from the 2007 version,
and discusses implications for Indian professionals dealing
with affected families.
Keywords: Dignostic tools,
Investigations, Neuroimaging, Screening.
|
|
T
he American Academy of Pediatrics (AAP) recently
released clinical guidelines for the evaluation and management of
children and adolescents with autism spectrum disorder (ASD) [1]. The
previous 2007 guidelines covered both separately [2,3]. Many changes
have occurred over the last 12 years: increasing prevalence; revised
nomen-clature and diagnostic criteria of Diagnostic and Statistical
Manual of Mental Disorders, fifth edition (DSM-5) [4,5]; greater
understanding of clinical profile [6], neurobiology and etiopathogenesis;
advances in genetic testing [7]; evidence-based interventions; and a
paradigm shift to family-centred therapy and holistic management
throughout life. Understandably, there was a strong need for an update.
The increasing worldwide prevalence of ASD means
primary care service providers (PCP) and pediatricians will encounter
ASD routinely. Not only should we be competent enough to recognize,
evaluate and establish diagnosis, we should be empowered to counsel,
help families in decision making, and provide continual support. After
outlining salient features of the 2020 guidelines and highlighting
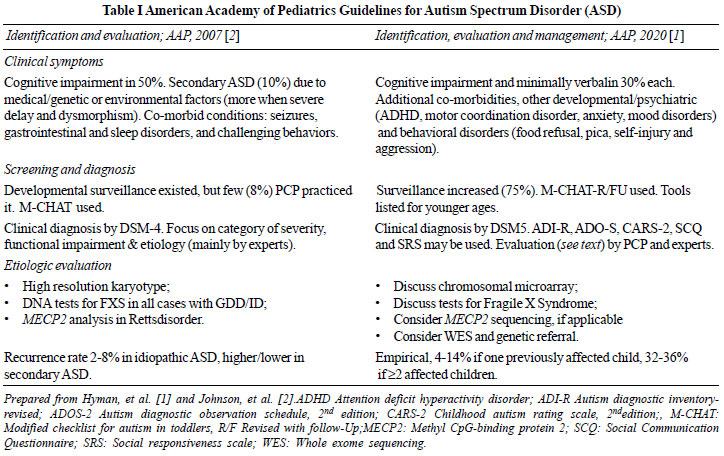
differences from the last one (Tables I and II),
implications for Indian professionals will be discussed.
 |
| |
 |
| |
Previously, increasing prevalence was attributed to
growing awareness, improving surveillance and less misdiagnoses [2]. The
present status (1in 59) of ASD in the US is also probably due to
broadening of phenotype by DSM-5, universal surveillance and increased
availability of services. Whether biological risk factors contribute to
etiopathogenesis remains uncertain [1]. Earlier diagnosis is more common
in higher socio-economic strata who have better access to services,
while later identification is associated with milder manifestations.
Clinical symptoms include core symptoms and co-existing conditions
(medical, genetic, neuro-developmental, psychiatric and/or behavioral),
the cumulative effect of which influence extent of social and functional
impairment. The guidelines described these in-depth. They also emphasize
the need for holistic evaluation and management to achieve best possible
outcomes.
Screening and Diagnosis
The USA health system practices universal
developmental surveillance with ASD-specific screening at 18 and 24/30
months. Earlier screening is indicated in high-risk individuals or when
red flags for ASD are identified. Suspicion or parental concerns warrant
in-depth evaluation. Establishment of diagnosis is primarily clinical,
based on parental interview, personal observations and DSM-5 criteria.
Though diagnostic tools are not mandatory, they help in extracting
clinical information. Structured evaluation of behaviour, cognition,
language, adaptive function, motor function, hearing, vision and sensory
processing is recommended. Diagnoses established by the aforementioned
compre-hensive assessment in children under 30 months remain stable in
³80% in
adulthood.
Etiologic evaluation comprises of detailed
history-taking and examination (anthropometry, dysmorphism, skin,
neurologic and systemic). The indications for magnetic resonance imaging
(MRI), electroencephalo-graphy (EEG) and metabolic testing remain
individualized, with provision of more details. Genetic evaluation is
recommended in all. The advantages of establishing genetic etiology
include accuracy in counselling, possible specific therapy, avoiding
unnecessary testing, and increased family acceptance.
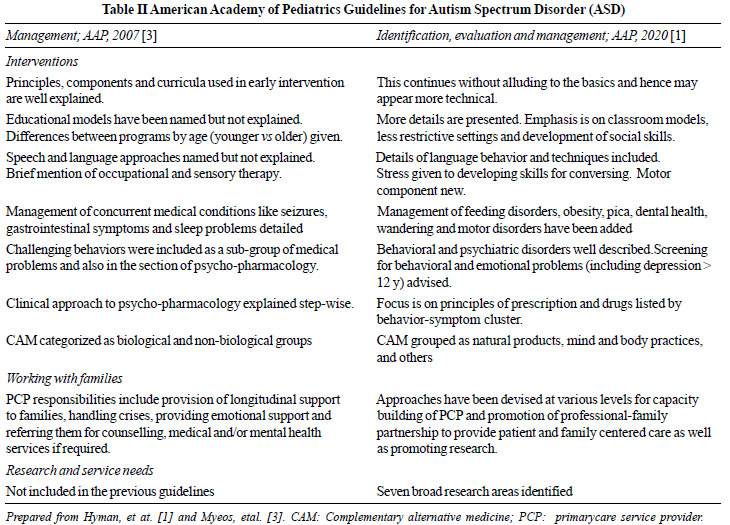
Interventions
The goals remain minimizing core deficits,
eliminating maladaptive behaviour, and maximizing functional
independence. Intervention should be "individualized, developmentally
appropriate and intensive" [1]. Periodic documentation of performance is
required for monitoring response. The caveat that all interventions
should be evidence-based has been added, with enumeration of
characteristics of effective intervention.
Some sections i.e., models of early
intervention and education, psychopharmacology and complementary
alternative therapy (CAM) are quite technical, since the basics were
extensively explained in the previous guidelines. Hence, non-experts may
not understand them unless they read the earlier version. Management of
medical conditions, social skill instruction, speech and language
therapy, motor therapy (including occupational therapy) and sensory
therapies (the supportive evidence of which is still low) are given in
greater detail.
Evaluation of maladaptive behavior and psychiatric
conditions are separate and described with respect to the atypical
development of ASD. The psychopharmacology section details principles of
prescription and lists medications according to behavior-symptom
cluster. The emerging role of psycho-pharmacogenetic testing is
mentioned. According to the new guidelines, if a family opts for CAM,
safety and effectiveness requires monitoring.
Working with Families
The USA‘Medical home’ model for primary care aims at
"accessible, continuous, comprehensive, family centred, coordinated,
compassionate, and culturally sensitive health care for all children and
youth, including those with special needs" [8]. Though recommended for
ASD since 2007, the process was not well-defined. The latest guidelines
aim at better PCP and caregiver partnership, revolving around shared
decision-making. Resources have been developed for pediatricians to
enable them to deal with emerging issues, counsel effectively, provide
parents with information and direct them towards advocacy and support
groups. It is envisioned that this will result in easier handling of
challenges, smoother transitions during adolescence (higher
education/vocation, sexuality) and adulthood (employment readiness,
medical care, legal guardianship and living arrangements), and better
understanding of ASD related rights and laws.
Research and Service Needs
Key areas identified to direct focus of funding
include, basic and translational science (genetics, epigenetics,
neurobiology, psychopharmacology), clinical trials for focussed
interventions, epidemiological surveillance and implementation research
for health care services.
Implications for the Indian Setting
These guidelines have brought our existing lacunae to
the forefront. Few pediatricians routinely practice developmental
surveillance. Though DSM-5 and indigenous Indian tools are used for
diagnosis, and intervention centres have been established all over the
country, there is wide variability in skills and availability of
multi-disciplinary professionals dealing with ASD, inconsistency in
practice protocols, and minimal quality checking. National Trust
workshops are infrequent and primarily related to disability
certification. Consensus statements and clinical practice guidelines
framed by expert bodies [9,10] sensitize professionals, but do not focus
on capacity-building.
Given these challenges, the provision of easily
accessible, family centred, individualized and intensive,
multi-disciplinary intervention according to these recommendations (but
tailored to Indian settings) to all affected families is still a distant
goal. The need of the hour is planning and implementing evidence-based
concrete strategies that will enable professionals dealing with ASD to
provide global standards of care to these children and their families.
Quality improvement, collaboration and integration is
required among the health, education, social welfare and public health
systems to provide evidence-based, universal care to
children/adolescents and families affected by ASD. The 2020 guidelines
outline strategies for capacity building of PCP to support this
vulnerable population from suspicion of ASD, through diagnosis and
service provision, to adulthood.
REFERENCES
1. Hyman SL, Levy SE, Myers SM. AAP Council on
Children with Disabilities, Section on Developmental and Behavioural
Pediatrics. Identification, Evaluation, and Management of Children with
Autism Spectrum Disorder. Pediatrics. 2020;145:e20193447.
2. Johnson CP, Myers SM, and the Council on Children
with Disabilities. Identification and Evaluation of Children with Autism
Spectrum Disorders. Pediatrics. 2007;120:1183-215.
3. Myers SM, Johnson CP, and the Council on Children
with Disabilities. Management of Children with Autism Spectrum
Disorders. Pediatrics. 2007;120:1162-82.
4. American Psychiatry Association. Diagnostic and
Statistical Manual of Mental Disorders, 5th ed. Arlington, VA: American
Psychiatric Publishers; 2013.
5. Sharma N, Mishra R, Mishra D. The fifth edition of
diagnostic and statistical manual of mental disorders (DSM-5): What is
new for the pediatrician? Indian Pediatr. 2015;52:141-3.
6. Hodges H, Fealko C, Soares N. Autism spectrum
disorder: Definition, epidemiology, causes, and clinical evaluation.
TranslPediatr. 2020;9(Suppl 1):S55-S65.
7. Schaefer GB, Mendelsohn NJ. Clinical genetics
evaluation in identifying the etiology of autism spectrum disorders:
2013 guideline revisions. Genet Med. 2013:15:399-407.
8. AAP Medical Home Initiatives for Children with
Special Needs Project Advisory Committee. The Medical Home. Pediatrics.
2002;110:184-6.
9. Dalwai S, Ahmed S, Udani V, Mundkur N, Kamath SS,
Nair MKC. Consensus Statement of the Indian Academy of Pediatrics on
Evaluation and Management of Autism Spectrum Disorder. Indian Pediatr.
2017;54:385-93.
10. Subramanyam AA, Mukherjee A, Dave M, Chavda K.
Clinical Practice Guidelines for Autism Spectrum Disorders. Indian J
Psychiatry. 2019;61:254-69.
|
|
|
 |
|

