|
|
|
Indian Pediatr 2020;57:
950-956 |
 |
A Road Map for Simulation Based Medical Students Training
in Pediatrics: Preparing the Next Generation of Doctors
|
|
Geethanjali Ramachandra, 1,2
Ellen S Deutsch,2,3
and Vinay M Nadkarni2,3
From 1Krishna Institute of Medical Science
Secunderabad, Telangana, India; 2Pediatric Simulation
Training and Research Society (PediSTARS), India; and 3Children’s
Hospital of Philadelphia, University of Pennsylvania, Perelman School of
Medicine, USA.
Correspondence to: Dr Geethanjali Ramachandra, Department of
Pediatric Intensive Care, Krishna Institute of Medical Science, Minister
Road, Secunderabad 500 003, Telangana, India.
Email: [email protected]
|
|
Current Medical training in India is
generally didactic and pedagogical, and often does not systematically
prepare newly graduated doctors to be competent, confident and
compassionate. After much deliberation, the Medical Council of India
(MCI) has recently introduced a new outcome-driven curriculum for
undergraduate medical student training with specific milestones and an
emphasis on simulation-based learning and guided reflection.
Simulation-based education and debriefing (guided reflection) has
transformed medical training in many countries by accelerating learning
curves, improving team skills and behavior, and enhancing provider
confidence and competence. In this article, we provide a broad framework
and roadmap suggesting how simulation-based education might be
incorporated and contextualized by undergraduate medical institutions,
especially for pediatric training, using local resources to achieve the
goals of the new MCI competency-based and simulation-enhanced
undergraduate curriculum
Keywords: Competency,
Integration, Medical education, Undergraduate.
|
|
G raduates, through didactic
training and apprenticeships, focus on improving knowledge. However,
graduates often have gaps in skills, behaviors and attitudes, so
alternative forms of education are necessary to support competence,
confidence, communication skills, and compassion in caring for children.
Entering internship after the final year of medical school, students are
required to perform many critical actions independently. Most of the
students in the Indian subcontinent learn clinical care by practicing on
real patients which may result in physiological and psychological harm
to the patients and families, as well as excessive stress to the new
graduate. Simulation is a powerful tool that can facilitate learning in
a safe environment by deliberate practice and facilitated reflection.
Using simulation to address individual and team skills, behaviors and
attitudes was addressed previously in the journal [1] – we add to it in
the light of the new MCI curriculum.
New MCI Curriculum
The Medical Council of India (MCI) has proposed an
exciting new initiative to revamp medical training by creating a
competency based undergraduate curriculum for the Indian medical
graduate [2,3]. The new curriculum focuses on Attitude, Ethics and
Communication (AETCOM); calls for preparing students to face India’s
health needs by training to be a "Clinician, Communicator, Team leader,
Professional and Lifelong Learner"; emphasizes collaborative and
inter-disciplinary teamwork, professionalism, respect and responsiveness
to the needs of the patient; limits didactic lectures to less than a
third of total schedule; integrates communication skills training; and
uses simulation training and guided reflection
The new MCI competency-based pediatric medical
graduate curriculum is based on seven core competencies (Box I).
MCI emphasises that the teaching should be aligned and integrated both
horizontally (across disciplines in a given phase of the course) and
vertically (across different phases of the course). This will allow
graduates to provide comprehensive care for neonates, infants, children
and adolescents based on a sound knowledge of growth, development,
disease and their clinical, social, emotional, and psychological
correlates in the context of national health priorities [4]. MCI has
directed individual undergraduate medical institutes to form their own
curriculum committees to implement these standards [5].
|
Box I The New Medical Council of India
Competency-based Pediatric Curriculum of the Indian Medical
Graduate Program [4]
Pediatric Competencies students must
demonstrate
1. Ability to assess and promote optimal
growth, development and nutrition of children and adolescents
and identify deviations from normal.
2. Ability to recognize and provide emergency
and routine ambulatory and First Level Referral Unit care for
neonates, infants, children and adolescents and refer as may be
appropriate.
3. Ability to perform procedures as indicated
for children of all ages in the primary care setting.
4. Ability to recognize children with special
needs and refer appropriately.
5. Ability to promote health and prevent
diseases in children.
6. Ability to participate in National
Programmes related to child health and in conformation with the
Integrated Management of Neonatal and Childhood Illnesses
(IMNCI) Strategy.
7. Ability to communicate appropriately and effectively.
|
Can Simulation Bridge Current Gaps in Training?
The new MCI curriculum aspires to ensure that the
medical graduate meets or exceeds global benchmarks in knowledge,
attitudes, behaviors, skills and communi-cation abilities, and is able
to provide holistic care with compassion. How do we achieve this goal?
Didactic education will help the learner to gain
knowledge, whereas simulation-based education (SBE) will help the
learner to apply their knowledge by creating realistic experiences in a
controlled, low risk and interactive environment. Debriefing, which is
an integral component of the simulation experience, facilitates mindful
reflection, active learning, abstraction, conceptualisation, and
application of theory to real events. Integrating didactic teaching and
SBE will provide shorter learning curves, higher retention and improved
behavior in future patient care encounters, helping learners emerge as
leaders, communicators, professionals and health advocates [1,6-8].
Studies have shown that pediatric trainees become more confident in
recognising, assessing, managing sick children, and in communicating
after simulation-based training [9-12].
Progress Towards SBE in India
It is encouraging to see a few institutions in India
already taking an active interest in incorporating simulation for
undergraduate training. At the All India Institute of Medical Science
(AIIMS) Delhi, and many other institutions, skills are taught using a
blended learning technique with both online and hands-on teaching
sessions. The online segment consists of a brief description of the
standard operating procedure (SOP) and a video of skills such as
intravenous (IV) cannulation, hand washing, gowning and gloving,
glucometer use, bag and mask ventilation, chest compressions,
endotracheal intubation, laryngeal mask airway (LMA) insertion, basic
suturing, and episiotomy suturing. The students need to answer a few
multiple-choice questions based on the information given in the SOP and
video and then they are allowed to come for hands-on sessions. Apart
from the above, a simulation-based neonatal resuscitation program (NRP)
is being run for the students during their 6th semester. Future steps
include incorporating team training and human factors in simulation.
Centres such as Father Muller Simulation and Skills Centre; DY Patil
Medical Simulation Laboratory; Kasturba Medical College (KMC), Manipal;
and GSL smart lab, Andhra Pradesh have already commenced incorporating
simulation in pediatric undergraduate training.
OVERVIEW IN OTHER COUNTRIES
Use of simulation-based education in pediatrics is
used in majority of institutions in USA [13]. SBE is based on 13 core
‘Entrustable professional activities for entering residency’ from the
Association of American Medical Colleges [14]. Most centres in USA,
Canada, United Kingdom and New Zealand introduce simulation to students
in the first year of medical training and gradually increase the
duration and complexity from year 2 onwards using both skill
laboratories and in-hospital simulation.
Typically, students learn various procedural skills
(such as cannulation, blood sampling, suturing, intubation,
thoracentesis, aseptic precautions), history taking, basic life support,
airway, focussed examination, leadership, handover, interprofessional
and family communication in simulation centres, and management of
emergencies with team training at hospital. Combinations of task
trainers, manikins with varying amounts of technology (low, medium,
high), virtual reality (VR) simulations, and standardized patients (SP)
are used for training at simulation centres. Simulation is also used as
an evaluation tool and to assess knowledge e.g., Objective
Structured Clinical Examination (OSCE) stations [15,16].
At the Children’s Hospital of Philadelphia (CHOP),
medical students undergo pediatric simulation training at a simulation
centre at the University of Pennsylvania Perelman College of Medicine.
In addition, during year 3 and 4 they undergo in situ simulation
training at CHOP. Small batches of five third year students participate
in simulation once-a-week to learn team training, neonatal apnea,
asthma, croup, febrile seizure, hypoglycemic seizures for 5 weeks.
Similarly, fourth-year students visit once-a-week to learn team
training, identification of sick child, high quality resuscitation,
cardiac arrhythmias, anaphylaxis and septic shock using scripted
scenarios and high technology manikins. Debriefing normally takes twice
the time of conducting the scenario. Prior to commencing internship,
medical students participate in a 5-day intense pediatric boot camp. The
boot camp is structured to mimic real work in a Pediatric ward and
emergency room involving allied professionals such as radiology,
physiotherapy, occupational therapy, speech therapy, child life and
lactation specialists. Emphasis on personal wellbeing in addition to
skills such as PALS emergencies and handoff communication has made this
boot camp a great success [11,17]. CHOP is also helping overseas centres
conduct team training and debriefing through tele-simulation.
WHAT IS NEEDED FOR SIMULATION-BASED TRAINING?
To succeed in our mission to provide SBE, we need
commitment by the faculty and administration, a clear roadmap, passion
to succeed and, willingness to invest for our new generation of young
doctors. Now that the need for SBE has been identified [2-5], next steps
will be to develop faculty, secure funding, identify space for
simulations, procure manikins and other equipment, train personnel,
design curricula and script scenarios. Ongoing research and feedback to
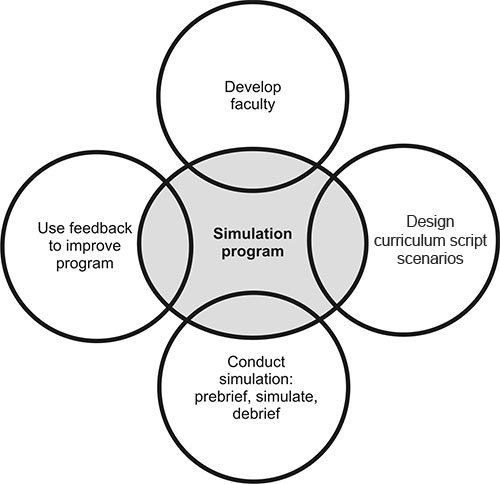
refine the curriculum will lead to high quality training (Fig.
1 and 2).
 |
|
Fig. 1 Designing a simulation program.
|
Faculty development: This is the most vital part
of a simulation program. There are 2 or 3-day simulation faculty
development courses available, emphasizing curriculum development and
debriefing followed by ongoing audit and mentorship.
Access to resources: Funding, identifying space,
manikins, audio-visual aids, appropriate equipment to create a realistic
patient-care environment, an enclosed observation room, debriefing room
and personnel to manage the program are some of the resources required
for a successful simulation program.
Curriculum design: SBE design involves
appropriate needs analysis, clearly defined objectives, selection of the
type of simulation, descriptions of learner and trainers, determination
of place (simulation laboratory/in situ/other), identification of most
appropriate simulation modality, decision about the duration of
simulation, contextualized and validated evaluation tools, and any
assessment needed. It is important to have specific and measurable
objectives [17-19].
Scenario development: It involves scripting the
scenario with a title, learning objectives, case history ‘stem’ to be
told to the learners, manikin, props and moulages needed, additional
background information for facilitators, scenario flow and debriefing
script.
Delivering simulation: Prebriefing for
psychological safety of the learners, introduction of the environment,
parameters of simulation, capabilities of manikin, and suspension of
disbelief about manikin is the key to facilitate learning during
formative simulations. For immersive simulation, it is desirable that
room should match the clinical area and instructors stay out of sight of
the learners during the scenario. Appropriate audio-visual aids add
realism to the scenario [18,19].
Debriefing: This is the heart of simulation and
converts experience into learning. Learners are guided by a facilitator
to reflect on their actions, reinforce correct responses, and plan for
better performance. There are various types of debriefing techniques,
including direct feedback, plus delta, pause and debrief, rapid cycle
deliberate practice (RCDP) and advocacy inquiry [20-22]. Studies have
shown that scripted debriefing might be more beneficial to novice
faculty [23]. Attention is focused not only on ‘what could be improved’
but also ‘what went well’, and often asks learners to develop their own
insights into ‘why’ processes went well or needed improvement.
Research, feedback and refinement: Research into
the program to measure the impact of training and ongoing feedback to
refine the curriculum and scripts are key for a successful simulation
program, but must be carefully implemented to preserve psychological
safety for learning.
A Framework to Implement Simulation-based-training in
Pediatrics
MCI 2018 guidelines describe several competencies in
the pediatric curriculum for medical students [4]. A stepwise approach
starting with simpler skills in year 1, and adding more complex skills
and scenarios in subsequent years would allow learners to build on
skills they have developed (Fig. 3). This will also allow
trainers with specific skill sets to support skill training and reserve
highly trained simulation educators for more complex simulation
scenarios.
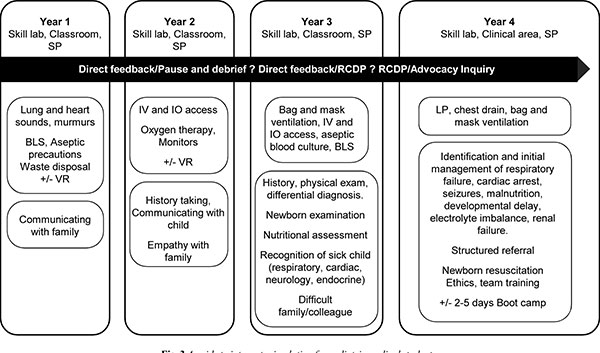
SP: Standardized patient; BLS: Basic life
support; VR: Virtual reality; IV: Intravenous; IO: Intra
osseous; LP: Lumbar puncture; RCDP: Rapid cycle deliberate
practice [21].
|
|
Fig. 3 A guide to integrate simulation for pediatric
medical students.
|
It is desirable to start with the highest priority
competencies, such as identifying a sick child, performing basic
procedures such as cannulation, intraosseous (IO) access, handwashing,
aseptic precautions, waste disposal, and communicating effectively with
families. Other competencies can be gradually integrated as a multistep
process. Simulations such as history taking, airway management, basic
life support (BLS), lumbar puncture, newborn examination, and
nutritional assessment can focus on individual learning. However,
emergency scenarios such as management of respiratory distress, cardiac
arrest, septic shock, and seizures, and dealing with challenging
families should be conducted as team training exercises so students can
also develop skills in leadership, role allocation, calling for help,
resource utilisation and providing clear instruction to colleagues [20].
Challenges
Faculty comfort will be a major challenge, because of
the huge volume of students, the need for specialized training in
simulation and a lack of time. Faculty development, manikin
availability, cost, and access to space can be a burden unless
management and infrastructure support is available. Psychological safety
for the students is extremely important to ensure learning from
simulation, and this also applies to faculty who are developing their
own simulation skills. Without psychological safety, both the learner
and the program may be damaged.
Overcoming Barriers
A previous publication [1] called for exploring and
embracing SBE in Indian subcontinent. After 4 years, it is exciting to
witness incorporation of simulation by MCI in undergraduate curriculum
and watch the breakthrough happening at some of the leading institutions
in India. India is one of the most cost-effective countries when it
comes to healthcare [24]. It is only a question of time for SBE to be
applied across the country in medical education.
Creating a pool of highly trained faculty, optimizing
low cost simulation opportunities, sharing resources, combining
simulation with didactic classroom lectures [25,26], encouraging
development of 3D printing, virtual reality [27], collaborating with
simulation training organizations [28-30], and research into the impact
of high-quality simulation-based training are some of the answers.
Indian students deserve the best education platforms. Table I
provides some insights into how we can make substantial progress.
CONCLUSION
It is now time for the much-needed paradigm shift –
the time to incorporate simulation in medical education countrywide. It
is no longer acceptable for our medical students to learn and practice
on real patients, without first learning and training on simulated
patients and situations. Simulation will never replace learning based
upon exposure to real patients but will increasingly supplement and
augment medical education in India. We need to think differently and be
constructively disruptive as we develop simulation-based medical student
curricula. The cost of integrating simulation into medical student
education is modest compared to the potential number of lives saved and
the joy of learning provided to our new generation of caring, able,
deserving, and intelligent doctors.
Acknowledgements: Ashok Deorari, All India
institute of Medical Science, Delhi. India; Rashmi Ramachandran, All
India Institute of Medical Science, Delhi, India; Adam Cheng, KidSIM
Simulation Program, Alberta, Canada; Gregg Lipschik, Life Support
Training and Undergraduate Curriculum Simulation at Penn Medicine
Philadelphia, USA; Erin Pete Devon, The Children’s Hospital of
Philadelphia, University of Pennsylvania. USA; Harsh Bhoopatka, Clinical
Skills Centre, University of Auckland New Zealand; Evan Sanders, Harvard
Medical School. USA; Malcolm Smith, Department of Simulation, University
of Leicester, UK; Jane Torrie, Faculty of Medical and Health Sciences,
University of Auckland, New Zealand.
Contributors: GR: reviewed the literature,
drafted and finalized the manuscript. ED, VN: reviewed, revised and
finalized the manuscript.
Funding: None; Competing interests: None
stated.
REFERENCES
1. Kalaniti K, Campbell DM. Simulation-based medical
education: Time for a pedagogical shift. Indian Pediatr. 2015;52:41-5.
2. Medical Council of India. Competency based
Undergraduate Curriculum for the Indian Medical Graduate, 2018. Vol 1,
pages 1-251. Available from:
https://www.mciindia.org/CMS/wp-content/uploads/2019/01/UG-Curriculum-Vol-I.pdf.
Accessed August 31, 2019.
3. Medical Council of India. Competency Based
Assessment Module for Undergraduate Medical Education Training Program,
2019: pages 1-30 Available from: https://mciindia.org/CMS/ wpcontent/uploads/2019/10/Module_
Competence_based_02.09.2019.pdf. Accessed August 31, 2019.
4. Medical Council of India, Competency based
Undergraduate curriculum for the Indian Medical Graduate, 2018. Vol II –
Pediatrics: pages 150-201. Available from: https://www.mciindia.org/
CMS/wp-content/uploads/2019/01/UG-Curriculum-Vol-II.pdf. Accessed
August 31, 2019.
5. Medical Council of India, Curriculum
Implementation Support Program of the Competency Based Undergraduate
Medical Education Curriculum 2019. p. 1-188.
6. So HY, Chen PP, Wong GKC, Chan TTN. Simulation in
medical education. JR Coll Physicians Edinb. 2019; 49:52-7.
7. Okuda Y, Bryson EO, DeMaria S Jr, Jacobson L,
Quinones J, Shen B, et al. The utility of simulation in medical
education: what is the evidence? Mt Sinai J Med. 2009; 76:330-43.
8. Cheng A, Lang TR, Starr SR, Pusic M, Cook DA.
Technology-enhanced simulation and pediatric education: A meta-analysis.
Pediatrics. 2014;133:e1313-23.
9. Ooi A, Hambidge J, Wallace A. Developing an
undergraduate paediatric simulation workshop in a resource constrained
setting: A practical ‘how to’ guide. J Paediatr Child Health.
2019;55:737-42.
10. Morrissey B, Jacob H, Harnik E, Mackay K,
Moreiras J. Simulation in undergraduate paediatrics: A
cluster-randomised trial. Clin Teach. 2016;13:337-42.
11. Pete Devon E, Tenney-Soeiro R, Ronan J, Balmer
DF. A pediatric preintern boot camp: Program development and evaluation
informed by a conceptual framework. Acad Pediatr. 2019;19:165-9.
12. Stone K, Reid J, Caglar D, Christensen A,
Strelitz B, Zhou L, et al. Increasing pediatric resident
simulated resuscitation performance: A standardized simulation-based
curriculum. Resuscitation. 2014;85:1099-105.
13. Vukin E, Greenberg R, Auerbach M, Chang L,
Scotten M, Tenney-Soeiro R, et al. Use of simulation-based
education: A national survey of pediatric clerkship directors. Acad
Pediatr. 2014;14:369-74.
14. Association of American Medical Colleges (AAMC).
Core entrustable professional activities for entering Residency:
Toolkits for the 13 Core EPAs. Jan 2017. p. 1-20. Available from:
https://www.aamc.org/system/files/c/2/484778-epa13toolkit.pdf.
Accessed August 31, 2019.
15. Nadkarni LD, Roskind CG, Auerbach MA, Calhoun AW,
Adler MD, Kessler DO. The development and validation of a concise
instrument for formative assessment of team leader performance during
simulated pediatric resuscita-tions. Simul Healthc. 2018;13:77-82.
16. Ryall T, Judd BK, Gordon CJ. Simulation-based
assessments in health professional education: A systematic review. J
Multidiscip Health. 2016;9:69-82.
17. Hartke A, Pete Devon E, Burns R, Rideout M.
Building a boot camp: Pediatric residency preparatory course design
workshop and tool kit. MedEdPORTAL. 2019;15:10860. Available from:
https://doi.org/10.15766/mep_2374-8265.10860. Accessed August 31,
2019.
18. Cheng A, Duff J, Grant E, Kissoon N, Grant VJ.
Simulation in paediatrics: An educational revolution. Paediatr Child
Health. 2007;12:465-8.
19. Lopreiato JO, Sawyer T. Simulation-based medical
education in paediatrics Acad Pediatr. 2015;15:134-42.
20. Roussin CJ, Weinstock P. SimZones: An
organizational innovation for simulation programs and centers. Acad Med.
2017;92:1114-20.
21. Hunt EA, Duval-Arnould JM, Nelson-McMillan KL,
Bradshaw JH, Diener-West M, Perretta JS et al. Pediatric resident
resuscitation skills improve after ‘‘rapid cycle deliberate practice’’
training. Resuscitation. 2014;85:945-51.
22. Rudolph JW, Simon R, Dufresne RL, Raemer DB.
There’s no such thing as "nonjudgmental" debriefing: A theory and method
for debriefing with good judgment. Simul Healthc. 2006;1:49-55 .
23. Cheng A, Hunt EA, Donoghue A, Nelson-McMillan K,
Nishisaki A, Leflore J, et al. Examining pediatric resuscitation
education using simulation and scripted debriefing: A multicenter
randomized trial. JAMA Pediatr. 2013;167:528-3.
24. Govindarajan V, Ramamurti R. India’s secret to
low-cost health care. Harvard Business Review. Available from:
https://hbr.org/2013/10/indias-secret-to-low-cost-healthcare.
Accessed August 31, 2019.
25. Fitch MT. Using high-fidelity emergency
simulation with large groups of preclinical medical students in a basic
science course. Med Teach. 2007;29:261-3.
26. Heitz C, Brown A, Johnson JE, Fitch MT. Large
group high-fidelity simulation enhances medical student learning. Med
Teach. 2009;31:e206-10.
27. Vincent DS, Sherstyuk A, Burgess L, Connolly KK.
Teaching mass casualty triage skills using immersive three-dimensional
virtual reality. Acad Emerg Med. 2008; 15:1160-5.
28. International Network for Simulation-based
Pediatric Innovation, Research and Education (INSPIRE). Available from:
http://www.inspiresim.com/. Accessed August 31, 2019.
29. International Pediatric Simulation Society
(IPSS). Available from: http://ipssglobal.org/. Accessed
August 31, 2019.
30. Society for Simulation in Healthcare. Available from:
https://www.ssih.org/. Accessed August 31, 2019.
|
|
|
 |
|

