V
isiting memory lane back to
the days of an undergraduate medical student, the first visuals
appearing in flash-back of most medical graduate are those of clinical
classes, held during the evening hours, conducted by residents, where
one used to have in-depth discussion on clinical cases and used to
finalize a work-up; where one could elicit sign and symptoms freely and
in a non-threatening environment; where probably one was more
comfortable in admitting mistakes and looking for ways to correct them.
Those sessions by residents and demonstrators helped medical
undergraduates immensely in honing their clinical reasoning and
psychomotor skills.
Residents and demonstrators are involved in routine
teaching activities in most of the departments. It has been estimated
that residents spend approximately 25% of their time teaching medical
students [1]. Another study found that residents spent 19% of their
total time in teaching activities, with 90% of this effort devoted to
teaching associated with patient care and 10% spent in classroom
teaching [2]. Even medical graduates perceive that 18% of the knowledge
they gained during clinical clerkships came from residents and 13% from
interns, compared with 25% from attending physicians and 43% from the
students’ own initiative [3]. As evident, residents have always been
involved in the departmental teaching activities. Of course, all these
figures are from other countries and no such data could be found from
India.
Is the picture same in India? Yes, to a large extent.
Residents are being used in departmental teaching activities without
being formally trained for the same in most of the non-clinical
subjects. We don’t have a data for clinical subjects either, but it
seems that utilization is suboptimal. With the introduction of
competency-based curriculum at undergraduate level there will be
paradigm shift and residents will be increasingly used for formal
teaching activities in India without any formal training. Should we not
have tailor-made faculty development activities for residents, both
senior residents as well as post-graduate students, in order to tap
their full potential in the conduct of the teaching activities in the
department? We are discussing some of these issues here.
RESIDENTS AS TEACHERS
Literature is full of the reasons and means of
involving residents-as-teachers in various medical disciplines, as
explained here.
Regulatory Obligations
The literal meaning of word doctor is – to teach
(derived from Latin verb docere). Being christened with the title
‘doctor’, residents are licensed to teach. Various regulatory bodies
also make it mandatory for residents to teach the undergraduate medical
students as they are given teaching experience certificate for the same,
which is counted for career progression. As per Medical Council of India
(MCI) regulations, three-year experience as Junior Residents and one
year experience as Senior Resident in a recognized medical college in
concerned subject is necessary to be appointed as Assistant Professor
[4]. Naturally residents, who are given teaching experience, must teach
as per regulatory and statutory provisions.
Institutional Requirements
Regulatory bodies have also mandated certain number
of senior and junior residents (tutors in pre- and para-clinical
subjects) to be appointed in medical colleges in all clinical
disciplines. These staffed residents will certainly be utilized for the
teaching purposes of undergraduate students.
Moreover, with the implementation of competency based
medical curriculum in India from the admission session 2019, it has
become imperative to use the services of residents in the teaching – as
more hands are needed for ‘assessment for learning’ purposes [5].
Refining Residents’ Own Competencies
Teaching is the highest form of understanding. As is
often quoted, ‘to teach is to learn twice.’ Being involved in teaching
process in the department provides residents opportunities to improve
their own perceived professio-nal competencies. Over the time, residents
have opined that teaching helps them in being good clinicians – as
teaching stimulates critical thinking and reflection on knowledge,
besides enhancing self-learning [6,7].
In another study, attending doctors expressed the
opinion that students and residents both are benefitted due to teaching
by residents and teaching by residents should be regarded as an integral
part of residency program [8].Thus involving residents in the
departmental teaching activities improve residents’ professional and
clinical competencies, as perceived by them.
BENEFITS OF USING RESIDENTS AS TEACHERS
Students often rate teaching by residents higher than
faculty teaching; and often view residents as more approachable, thus
encouraging them to acknowledge their mistakes easily and accept
feedback readily [9-11]. Residents-as-teachers also provide a kind of
support system for the students by acting as near-peer mentors.
When residents are used as teachers, it is not only
beneficial for the professional development of the students and the
residents but for the overall growth of the institutions also, thus
paving the way for the ultimate improvement in patient care outcomes (Fig.
1).
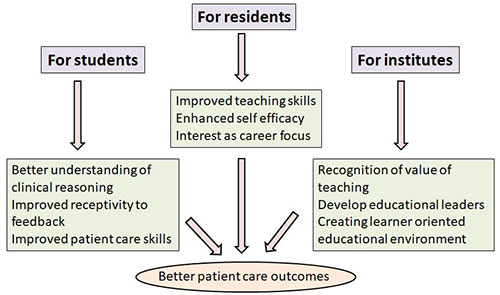 |
|
Fig. 1 Beneficial effects of using
residents as teacher.
|
NEED AND IMPACT OF EDUCATIONAL TRAINING PROGRAM FOR
RESIDENTS
For generations, residents teach the way they saw
their teachers do that and imbibe skills through ‘role modeling’.
However, learning the art and science of teaching through role modeling
alone is not the correct and optimal way of learning; one needs to have
formal experiential learning through formal training. Only a formally
trained resident in teaching technology will be motivated and dedicated
enough to have overall professional development. There are many reports
of formal residents-as-teachers program from many universities
worldwide. However, considering the unique and contextual nature of
educational content and environment, it may be worthwhile formulating
our own program. Residents and demonstrators are usually involved in
practical demonstrations, bedside teaching and sometimes in assessment
activities like conduct of objective structured clinical/practical
examinations (OSCE/OSPE). They are also increasingly being used for
skill development in the skill labs and other simulated environments.
Medical post-graduates are inherently trained to be
competent in-patient care; they are not trained as ‘medical teachers’.
Unlike requirements of having an educational degree in the field of
humanities and arts, there is no specialized degree in the field of
medicine which they must acquire in order to be medical teachers. This
precise reason has forced regulatory bodies to start faculty development
programs in medical educational techno-logies for the benefit of the
medical faculties. In India, Medical Council of India (MCI) has
developed two such structured programs –Basic Course Workshop in Medical
Educational Technologies and Advance Course in Medical Education [12].
If tailor-made faculty develop-ment programs are required to be
structured for medical faculty, the logic weighs-in on the side of
structuring and implementing such a training program in educational
technologies for residents also.
Literature has evidence that the training improves
the didactic, cognitive and clinical skills of the trainees [13]. Some
qualitative and quantitative studies have provided evidence of utility
of training for residents in educational technologies [6,14,15].
Morrison, et al. by using the Objective Structure Teaching
Examination to determine the impact of a 13-hour teaching training
program for residents found that compared to a control group, residents’
having undergone training had an overall improvement in teaching scores
by 28% [15]. However, Dunnington and DaRosa found minimal changes in
resident teaching behavior by using OSTE, after introducing a
residents-as-teachers intervention [16].
In another study, Snell by using triangulation of
data method tried to evaluate the effectiveness of a training program
for residents-as-teachers, which included five three-hour sessions. She
proved that trained residents had improved resident teaching skills,
showed better application of those skills and maintained those skills
over the academic year [17]. This is perhaps the only kind of study
using data from multi-sources to establish the effectiveness of training
programs for residents in educational technologies.
It is also pertinent to note that many of these
residents would be joining medical colleges as faculty. Others may end
up teaching DNB residents. It would thus be a useful intervention to
change the mindset towards teaching at an early stage of post-graduate
career.
TRAINING PROGRAM - DOCUMENTED EFFORTS
Training modules for the formal training of residents
in educational technologies and principles have been developed and
implemented by various universities and colleges, ranging from 2 hour
modules to workshops for 2-3 days to weekly / fortnightly one hour
training for up to six months duration [15,16]. Longitudinal training
programs in the form of electives for residents have also been designed,
implemented and evaluated [18-20]. In most of these training programs
and workshops, the most commonly used instruction methods were -
lectures, small group interactive sessions and role-play. Large group
interactive discussions and standardized students were the least
commonly used methods [21].
A literature search could retrieve very few studies
having used the concept of resident-as-teachers in India [22-24].Of
these studies, only Senior Resident Training on Educational Principles
(STEP) study has described a structured training module in the form of
workshop delivered to senior residents for enhancing their teaching
skills [22]. Maharashtra University of Health Sciences also started
‘resident as teacher’ program.[25] All such programs started at various
institutes could not sustain for various reasons; one of them possibly
being lack of conviction about utility of such an exercise. As
literature shows content, structure, duration and delivery variability
of different workshops/training programs designed for
residents-as-teachers, with hardly any visibility of such training
modules and programs in India and as the use of residents-as-teachers is
in transient phase in congruence with the paradigm shifts in the medical
education and undergraduate and post-graduate medical curriculum in
India. It is imperative that a structured training program in medical
education technologies for residents’ training in India be designed.
PROPOSED TRAINING MODULE
Though the need and effectiveness of a structured
program in educational technologies for residents is self-explanatory,
less than 10% of residents and interns reported to have undergone any
sort of training in teaching. This fact alone emphasizes the need to
design and implement a structured program for residents-as-teachers,
particularly tailor-made for our needs and requirements. Due to
differences in teaching-job profile, the structured module used for
training of the medical faculty can’t be used for the residents also.
Accordingly, a ‘Training-module for Residents’ in
India in Medical education technologies (TRIM)’ in the form of workshop,
based on some fundamental assumptions has been proposed here (Box
1).
|
Box 1 Fundamental Assumptions for Designing
Training Module for Residents
• Residents will be involved in teaching of
cognitive, psychomotor and affective domains to undergraduates
(UGs) including professionalism and ethics.
• Residents will be mainly involved in
interactive small group teaching and bedside teaching.
• Residents will act as role models for UGs,
thereby affecting soft skills including professionalism, ethics,
communication of UGs.
• Residents will act as mentors for UGs.
• Residents will be used for assessment of
UGs, of all domains, including assessment of knowledge.
• Residents will be particularly used for
assessment in simulated conditions, and more for formative
purposes.
• Residents will not be used for curriculum design or
curriculum evaluation.
|
The goal of the proposed program is to orient the
residents to the use of medical education teaching and assessment tools.
The content of the proposed program has been designed by extracting data
from three sources – previous experience of institutes in designing and
implementing such programs; MCI requirements for residents in India; and
curricular mandates requiring use of residents in students’ teaching as
per authors own experiences. Three main areas identified for training
and orientation of residents are – teaching principles and tools,
assessment and assessment tools, mentoring and teamwork.
The training module has been structured with the
objectives of sensitizing and training residents in the concepts of –
group dynamics and team-based learning, small group teaching, bedside
teaching, simulation based teaching and assessment, assessment of
learning and assessment for learning, and mentoring. These focused areas
align well with the teaching job profile of the residents. However,
efforts must be made to sustain this training through reinforcements
during residency as well as during working period as faculty, as and
when a resident joins as faculty in any institute. The description of
the sessions and the instructional strategies proposed for delivery of
those sessions has been briefed in Web Table I.
This workshop of 22 hours can be conducted over three
days, with 30-35 residents. If three-day continuous workshop is not
possible, the institute concerned can distribute sessions daily, as
appropriate.Trained faculty members from all departments can be
involved. A self-explanatory and most-appropriate instructional method
for the conduct of each session has been recommended; however local
factors like available infrastructure, availability of time, expertise
of facilitators will ultimately decide the choice of any of these
methods.
Local planners may consider adding sessions on –
appropriate use of multimedia, integrated teaching, assessment in
integrated teaching-learning, self-directed learning – if their local
needs direct the same. Similarly, based upon expertise of the faculty
other instructional strategies like – cine-meducation, team-based
learning, team objective structured clinical examination – can be used
[27-29]. One can also explore the possibility of using online platforms
and educational strategies for the delivery of the content; even
partially, if not fully. Combination of synchronous and face-to-face
training followed by asynchronous or synchronous online training can be
a viable option in institutes with heavy patient footfall, making time
constraints for residents a real issue.
EXPECTED OUTCOMES
What is expected to be achieved with this module? It
is not expected that with this training module the residents will be
fully equipped with all the teaching and assessment tools available in
the armamentarium. Only expectation is that the sensitized residents
after the training will start applying these concepts in their teaching
activities. They are expected to be handy resources as facilitators in
the conduct of Objective structured clinical examination/Objective
structured practical examination (OSCE/OSPE) in the department. After
the training, they must be field-ready to act as instructors in the
upcoming skill labs.
It is further expected that residents teaching skills
will evolve and will improve from ‘being novice’ to at least ‘advance
beginners’. More importantly residents are expected to build the concept
of ‘transfer of training’ at their young age as teachers and understand
the utility of having a learner-oriented educational environment in the
institute.
PROGRAM EVALUATION
A detailed plan of action for program evaluation of
the proposed "Training-module for Residents’ in India in Medical
education technologies (TRIM)" is out of the scope of this paper.
However, we are trying to issue generalized suggestions, so that the
program is evaluated and monitored continuously for refinement as well
as for ensuring accountability. The evaluation must include both process
evaluation and outcome evaluation. While outcome evaluation will measure
if the desired change has been achieved or not, the process evaluation
will measure how the desired change was achieved – that is if the
program was carried out as planned. Typically, a combination of logic
and Kirkpatrick’s model will be good enough for such a program
evaluation.
CHALLENGES IN IMPLEMENTING TRAINING PROGRAM
First challenge will be to find trained faculty for
the conduct of the training program of the residents as teacher. The
faculty needs to be trained themselves. The Medical Council of India’s
new guidelines, making revised basic course workshop as mandatory
requirement for promotion of faculty will result in many trained faculty
members. Faculty inertia and resistance will be the next big challenge
in the implementation of teachers training program for residents. The
resistance is not baseless even. Faculty in medical colleges is already
involved in multitasking – patient care, teaching postgraduates and
undergraduates, curriculum development, administrative duties to name a
few. Making arrangements and then conducting a workshop for residents
will be labor intensive; though the very incentive that the trained
residents will ultimately prove helping hands for these faculty members
for undergraduate teaching will motivate faculty to plan and conduct
such teachers training programs for residents.
Residents have multiple tasks to do – patient care,
research, participation in continued medical education programs
including training in research methodologies; so tapping their full
potential as teachers is a challenge in itself. Consequently, many
residents might be reluctant to attend teachers training
program.However, owing to the huge personal and professional benefits of
teaching undergraduate students, residents will get enough sensitization
to attend such a training program.
The training program needs to be monitored also, at
all levels, not only for continuous refinement and support but also for
seamless implementation. Monitoring any program is a challenge in
itself. Program evaluation and monitoring demands trained manpower,
infrastructure, time and coordination among different stakeholders.
Program evaluation plan, as proposed above, will be required to be
designed, once such a program is adopted for implementation.
CONCLUSIONS
There is huge man-power and potential available with
us in medical institute in India in the form of junior and senior
residents. Though routinely used in patient care, they must be used as
facilitators and instructors for departmental teaching and assessment
activities. It is logical to assume that orientation and training of
residents in the form of a workshop module will improve their acumen for
teaching activities. An informed, sensitized, oriented and trained
resident will prove to be a useful and productive resource for any
institute.
Contributors: TS: conceptualized the paper; RM:
prepared the initial manuscript:PG: finalized it; All authors provided
critical inputs and approved the final manuscript.
Funding: None; Competing interests: None
stated.
REFERENCES
1. Jarvis-Selinger S, Halwani Y, Joughin K, Pratt D,
Scott T, Snell L. Supporting the development of residents as teachers:
Current practices and emerging trends. Members of the FMEC PG
consortium; 2011.
2. Sheets KJ, Hankin FM, Schwenk TL. Preparing
surgery house officers for their teaching role. American Journal of
Surgery 1991;161;443-49.
3. Barrow MV. Medical student opinions of the house
officer as a medical educator. J Med Educ.1966; 41:807-10.
4. Medical Council of India. Minimum Qualification of
Teachers in Medical Institutions Regulations, 1998. Available from:https://www.mciindia.org/documents/rules
AndRegulations/Teachers-Eligibility-Qualifications-Rgulations-1998.pdf.
Accessed January 10, 2020.
5. Singh T, Anshu, Modi JN. The Quarter Model: A
Proposed Approach for In-training Assessment of Undergraduate Students
in Indian Medical Schools. Indian Pediatr. 2012; 49:871-76.
6. Busari JO, Prince KA, Scherpbier AJ, Van der
Vleuten CP, Essed GG. How residents perceive their teaching role in the
clinical setting – a qualitative study. Medical Teacher 2002; 24:57-61.
7. Sheets KJ, Hankin FM, Schwenk TL. Preparing
surgery house officers for their teaching role. Am JSurg1991;
161:443-49.
8. Busari JO, Scherpbier AJ, Van der Vleuten CP,
Essed GG. The perception of attending doctors of the role of residents
as teachers of undergraduate clinical students. Med Educ. 2003;
37:241-47.
9. Whittaker LD Jr, Estes NC, Ash J, Meyer LE. The
value of residentteaching to improve student perceptions of surgery
clerkships andsurgical career choices. Am J Surg.2006; 191:320-24.
10. Tolsgaard MG, Gustafsson A, Rasmussen MB, Hoiby
P, Muller CG,Ringsted C. Student teachers can be as good as associate
professorsin teaching clinical skills. Med Teach 2007; 29:553-57.
11. Ross MT, Cameron HS.Peer assisted learning: a
planning andimplementation framework: AMEE Guide no. 30. Med Teach.2007;
29:527-45.
12. Medical Council of India. Decisions of the
council regarding faculty development programmes. Available from:
https://mciindia.org/CMS/wp-content/uploads/2019/10/3_MCI_
decisions_on_MET.pdf. Accessed February 03, 2020.
13. Irby DM. What Clinical Teachers in Medicine Need
to Know?Acad Med. 1994:610:333-42.
14. Khera N, Stroobant J, Primhak RA, Gupta R, Davies
H. Training the ideal hospitaldoctor: The specialist registrars’
perspective. Medical Education 2001; 35:957-66.
15. Morrison EH, Rucker L, Boker JR, Hollingshead J,
Hitchcock MA, Prislin MD, et al. A pilot randomized,controlled
trial of a longitudinal residents-as-teachers curriculum. Acad
Med.2003;78:722-29.
16. Dunnington GL, DaRosa D. A prospective randomized
trial of a residents-as-teachers training program.Acad Med.1998;
73:696-700.
17. Snell L. Improving medical residents’ teaching
skills. Ann R Coll of PhysSurg Can.1989; 22:125-28.
18. Bharel M, Jain S. A longitudinal curriculum to
improve resident teachingskills. Med Teach. 2005; 27:564-66.
19. Mann KV, Sutton E, Frank B. Twelve tips for
preparing residents as teachers. Med Teach. 2007;29:301-06.
20. Weissman MA, Bensinger L, Koestler JL. Resident
as teacher: educatingthe educators. Mt Sinai J Med. 2006; 73:1165-69.
21. Morrison EH, Friedland JA, Boker J, Rucker L,
Hollingshead J, Murata P.Residents-as-teachers training in U.S.
residency programs and offices ofgraduate medical education. Acad Med.
2001;76: S1-S4.
22. Singh S. Senior resident training on educational
principles (STEP): A proposed innovative step from a developing nation.
J EducEval Health Prof.2010;7:3 (online). Available from:
https://www.jeehp.org/DOIx.php?number=45. Accessed February 03,
2020.
23. Kumar A, Agarwal D. Resident-to-resident bedside
teaching: An innovative concept. Indian J Ophthalmol. 2019; 67:1901-02.
24. Ghosh SK. Resident doctors: Keystone of anatomy
teaching. Clin Teach.2014; 11:461-62.
25. Homeo Book [Page on internet]. MUHS Master of
Science (Health Professions Education) 2016 admission. Available from:
https://www.homeobook.com/muhs-master-of-science-health-professions-education-2016-admission/.
Accessed May 04, 2020.
26. Wilkinson M. Team building activity – Crossing
the river. Available from:
https://www.leadstrat.com/leadership-strategy-resources/team-building-activity-crossing-the-river/.
Accessed February 04, 2020.
27. Kadeangadi DM, Mudigunda SS. Cinemeducation:
Using films to teach medical students. J SciSoc.2019;46:73-74.
28. Chhabra N, Kukreja S, Chhabra S, Khodabux S,
Sabane H. Team based learning strategy in biochemistry: Perceptions and
attitudes of faculty and 1st year medical students. Int J Appl Basic Med
Res. 2017;7:72-7.
29. Amini M, Moghadami M, Kojuri J, Abbasi H, Abadi
AA, Molaee NA, et al. Using TOSCE (Team Objective Structured
Clinical Examination) in the second national medical sciences Olympiad
in Iran. J Res Med Sci. 2012; 17:975-8.

