|
|
|
Indian Pediatr 2015;52:
893-895 |
 |
Ex-utero Intrapartum Treatment (EXIT)
Procedure for Giant Fetal Epignathus
|
|
Pooja Agarwal Jayagobi, Suresh Chandran, Bhavani
Sriram and *Kenneth TE Chang
From Departments of Neonatology and *Pathology &
Laboratory Medicine, Kandang Kerbau Women’s and Children’s Hospital,
Singapore.
Correspondence to: Dr Pooja Agarwal Jayagobi,
Associate Consultant, Department of Neonatology, Kandang Kerbau Women’s
and Children’s Hospital, 100 Bukit Timah Road, Singapore 229899.
Email:
[email protected]
Received: February 05, 2015;
Initial review: April 14, 2015:
Accepted: July 15, 2015.
|
|
Background: Large fetal oropharyngeal tumors are rare, and have the
potential to cause airway obstruction during birth. Case
characteristics: A 35-year-old woman with antenatally diagnosed
large heterogenous mass in fetal neck displacing trachea and filling up
the orophanygeal space. Intervention: The infant was delivered at
31 weeks of gestation by ex-utero intrapartum therapy procedure to
secure the airway. Outcome: Tumor was resected successfully on
day 8 of life. Histopathology revealed mixed teratoma. Message:
Ex-utero intrapartum therapy for fetuses with severe upper airway
compromise may prove life-saving.
Keywords: Antenatal diagnosis, Fetus,
Orolpharynx, Teratoma.
|
|
E
pignathus, a teratoma arising from the oral
cavity or pharynx, is rare in neonates. The estimated incidence is
1:35,000 to 1:200,000 live births with a female preponderance [1,2].
Arising from pluripotent cells, they contain all
three germ cell lines, and range from benign, well-differentiated cystic
lesions to those that are solid and malignant [3]. Large oropharyngeal
epignathi have the potential to cause life-threatening airway
obstruction and even death during or shortly after birth [1]. Antenatal
diagnosis gives the managing team an opportunity to perform an ex-utero
intrapartum treatment (EXIT) procedure to secure the airway. We report a
case of giant fetal epignathus delivered successfully by EXIT procedure
at 31 weeks of gestation.
Case Report
A 35-year-old woman was referred to us at 26 weeks of
gestation with threatened labor. Fetal scans were unremarkable at the
referral center. Ultrasound scan revealed a homogeneous mass 4.8 x 4.4 x
3.7 cm in the fetal neck along with polyhdramnios (amniotic fluid index
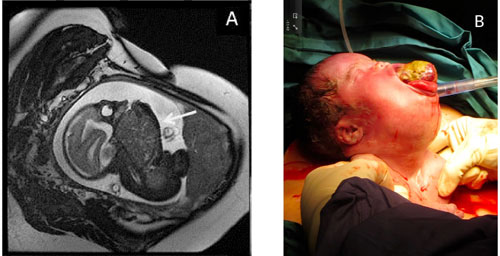
of 24 cm) necessitating an amnioreduction. Fetal magnetic resonance
imaging revealed a large heterogeneous mass in the anterior part of the
fetal neck posterior to the trachea, displacing it to the left, filling
up the oropharyngeal space, and infiltrating the floor of the mouth (Fig.
1a). This was suggestive of a teratoma with significant airway
compromise. There was no intrathoracic or intracranial extension. The
case was discussed at the multidisciplinary birth defect meeting and the
need for an EXIT procedure was felt. A team having obstetrician,
neonatologist, otolaryngologist, pediatric surgeon and anesthetists was
formed. They planned to secure the airway by EXIT procedure and resect
the mass after stabilization following imaging to delineate the anatomy
at 34 weeks of gestation. Serial scans showed a gradual increase in mass
size. A second amnioreduction was needed at 29 weeks.
 |
|
Fig. 1 (a) T2-weighted sagittal MRI
image showing a large mass in the anterior part of the fetal
neck, displacing the trachea (arrow); and (b) the neonate after
delivery of the head and shoulders showing the presence of the
large oral teratoma necessitating a tracheostomy.
|
An emergent delivery was needed at 31 weeks due to
rupture of membranes. The EXIT team was mobilized. A caesarean section
was done under deep general anesthesia. The fetal head and shoulders
were delivered. A giant solid mass protruding through the oral cavity
was noted (Fig. 1b), making any attempt at intubation
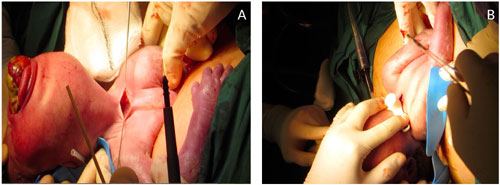
impossible. With the placental circulation still intact, the
otolaryngologist performed a tracheostomy (Fig. 2). Time
to tracheostomy from delivery of the head was 24 minutes. After
suctioning the trachea, surfactant was administered and the umbilical
cord was clamped. The infant weighed 2000 g. A computed tomography of
the neck showed a large heterogeneously enhancing mass distending the
oral cavity and oronasopharynx and abutting against the under surface of
the bony hard palate. Serum alpha-fetoprotein (AFP) level was markedly
elevated. At surgery on day 8 of life, the tumor was noted to be
attached to the anterior surface of the posterior put of tongue by a 3
cm stalk with no other oropharyngeal attachments. There was pressure
necrosis of the tip of the anterior part of tongue. The tumor was
vascular and composed of hair and cartilage. It was excised and a
hemiglossectomy was performed. A cleft palate was noted.
 |
|
Fig. 2 The neonate undergoing
tracheostomy during the EXIT procedure.
|
The resected tumor was lobulated pale-tan to
hemorrhagic and weighed 100 g. Histologically, the tumor was composed of
derivatives from all three germ cell layers including prominent immature
neuroectoderm, focal melanin pigmentation, choroidal epithelium,
cartilage, smooth and skeletal muscles, mucinous epithelium with focal
ciliation, squamous islands and liver tissue. The histological grade was
3 out of 3. No malignant germ cells were identified. Serial AFP levels
showed a declining trend postoperatively.
The patient was discharged at 2 months corrected age
with tracheostomy mask and tube feeds. At 5 months, there was a
recurrence at the base of the tongue, which was excised. Histopathology
report showed a mixed teratoma. Screening for metastasis was negative.
Gastrostomy was performed at 4 months of age to facilitate feeding.
Repair of the cleft palate was also done. Persistent sialorrhea was
controlled with scopolamine patches and botulinum toxin injections. At
15 months, he has mild gross motor delay with normal fine motor and
social skills. He has speech delay which is anatomical because of
glossectomy. Vision and hearing tests are normal. Discussions are
underway to assess the feasibility of tongue reconstruction.
Discussion
EXIT procedure was originally designed to remove
tracheal occlusion devices in fetuses with congenital diaphragmatic
hernia [4]. It can however be used to secure the fetal airway prior to
complete delivery whenever airway compromise is anticipated at birth
[5]. During EXIT, a cesarean section is done under general anesthesia.
This procedure differs from the usual caesarean section in that the
mother receives deep anesthesia and enough time is given for the
anesthetics to pass via the placental circulation to the fetus. The
goals are to maintain uterine relaxation and volume to maintain the
uteroplacental circulation, delay fetal-neonatal transition, achieve a
surgical level of fetal anesthesia without cardiac depression and
maintain normal maternal blood pressure during the period of deep
anesthesia [4]. Only the
fetal head and shoulders are delivered and the airway is secured by
intubation or tracheostomy while the placental circulation is intact.
Once the airway is secured, the fetus is delivered and the cord is cut.
In a large case series reported by Hedrick, securing
the airway was the most common indication for EXIT in fetuses with large
neck masses or congenital high airway obstruction syndrome [6]. Other
indications of the procedure are [4,7,8] for insertion of ECHO cannular
when severe hypoxia is anticipated in the delivery room due to pulmonary
or cardiac abnormalities; and for rapid control of the airway when twin
separation in conjoined twins is indicated for survival.
Our patient had a large oropharyngeal mass with
suspected airway compromise. She presented at 26 weeks which is beyond
the legal limit for medical termination of pregnancy. The team discussed
offering comfort care versus delivery by EXIT to the parents,
highlighting that this procedure had never been done in our country, and
the parents opted for an EXIT procedure.
Early radical excision is the treatment for large
head and neck teratomas without intracranial extension [9]. These are
mostly benign, and recurrence is rare [10]. Higher mortality in giant
oral teratomas is invariably due to the inability to secure airway
leading to death at or shortly after birth. The concept and expertise of
EXIT procedure is limited to only a few tertiary centers in the world,
and needs to be expanded.
Acknowledgements: Adjunct A/Prof Teo Eu-leong
Harvey James, Department of Diagnostic Imaging, and Dr Anicete Rosslyn
Capuno, Department of Otolaryngology for their help in providing the
images for this report. Ms. Siti Nurfadilah, Department of Neonatology
for her assistance in formatting the text and images.
Contributors: PAJ: Review of literature and
manuscript preparation, involved with antenatal planning, delivery and
managing the case; SC: Manuscript preparation and literature review; BS:
Manuscript preparation and involved with antenatal planning, delivery
and managing the case; KTEC: Provided the histopathology slides with
descriptions and interpretation.
Funding: None; Competing interests:
None stated.
References
1. Zhang GZ, Din GC, Zhao YF. Giant epignathus
teratoma: Report of a case. J Oral Maxillofac Surg. 2007;65:337-40.
2. Clement K, Chamberlain P, Boyd P, Molyneux A.
Prenatal diagnosis of an epignathus: A case report and review of the
literature. Ultrasound Obstet Gynecol. 2001;18:178-81.
3. Kountakis SE, Minotti AM, Maillard A, Stiernberg
CM. Teratomas of the head and neck. Am J Otolaryngol. 1994;15:292-6.
4. Harrison MR, Adzick NS, Flake AW, VanderWall KJ,
Bealer JF, Howell LJ, et al. Correction of congenital
diaphragmatic hernia in utero VIII: Response of the hypoplastic lung to
tracheal occlusion. J Pediatr Surg. 1996;31:1339-48.
5. Dighe MK, Peterson SE, Dubinsky TJ, Perkins J,
Cheng E. EXIT procedure: Technique and indications with prenatal imaging
parameters for assessment of airway patency. Radiographics.
2011;31:511-26.
6. Hedrick HL. Ex utero intrapartum therapy. Semin
Pediatr Surg. 2003;12:190-5.
7. Marwan A, Crombleholme TM. The EXIT procedure:
Principles, pitfalls, and progress. Semin Pediatr Surg. 2006;15:107-15.
8. Bouchard S Jouhnson MP, Flake AW, Howell LJ, Myers
LB, Adzick NS, et al. The EXIT Procedure: Experience and outcome
in 31 cases. J Pediatr Surg. 2002;37:418-26.
9. Vandenhaute B, Leteurtre E, Lecomte-Houcke M,
Pellerin P, Nuyts JP, Cuisset JM, et al. Epignathus teratoma:
Report of three cases with a review of the literature. Cleft Palate
Craniofac J. 2000;37:83-91.
10. Levine AB, Alvarez M, Wedgwood J, Berkowitz RL,
Holzman I. Contemporary management of a potentially lethal fetal
anomaly: successful perinatal approach to epignathus. Obstet Gynecol.
1990;76:962-6.
|
|
|
 |
|

