|
|
|
Indian Pediatr 2021;58:1046-1051 |
 |
Effect of Behavior
Change Communication on the Incidence of Pneumonia in Under Five
Children: A Cluster Randomized Controlled Trial
|
|
Jayashree Gothankar, 1
Prasad Pore,1 Girish
Dhumale,2 Prakash Doke,1
Sanjay Lalwani,3
Sanjay Quraishi,2 Sujata
Murarkar K,1 Reshma Patil,1
Vivek Waghachavare,2 Randhir
Dhobale,2 Kirti Rasote,2
Sonali Palkar1
From Departments of 1Community Medicine and 3Pediatrics, Bharati
Vidyapeeth Deemed to be University Medical College, Pune; and
2Department of Community Medicine, Bharati Vidyapeeth Deemed to be
University Medical College and Hospital, Sangli; Maharashtra.
Correspondence to: Dr Jayashree Gothankar, Department of Community
Medicine, Bharati Vidyapeeth Deemed to be University Medical College,
Off Pune Satara Road, Pune 411 043, Maharashtra.
Email: [email protected]
Received: November 25, 2020;
Initial review: February 25, 2021;
Accepted: August 18, 2021.
Trial Registration: CTRI/2017/12/010881
|
Background: Improving health education of the
mother by providing community-based interventions is known to help
control pneumonia.
Objective: To determine the effect of behavior
change communication (BCC) activities for mothers in reducing the
incidence of childhood pneumonia.
Design: Open-label cluster randomized controlled
trial.
Setting: Urban slums and villages in two districs
of Maharashtra.
Participants/Cluster: Under-five children and
their mothers from households in the randomly selected 16 clusters out
of total 45 clusters, stratified into Pune and Sangli districts and
further into rural and urban areas before randomization.
Intervention: Three forms of BCC activities were
imparted, viz., interactive sessions of education using pictorial
mothers’ booklet, screening of a audio-visual film, and virtual hand
wash demonstration and use of flashcard. Routine care under the National
health program was provided by the Accredited Social Health Activists
(ASHA) workers in both the arms.
Outcome: The primary outcome was pneumonia as per
the IMNCI criteria assessed during fortnightly visits of the ASHA/anganwadi
workers to the houses of under-five children, who received at least one
follow-up visit in a period of one year.
Results: The incidence of pneumonia in 1993 and
1987 under-five children in the intervention and control arm was 0.80
and 0.48 episodes per child per year, respectively (P=0.03).
Conclusion: BCC for mothers is not sufficient to
reduce the incidence of childhood pneumonia.
Keywords: Community intervention, Health education, Mothers,
Surveillance.
|
|
P
neumonia is one of the commonest cause of
under-five mortality [1] with estimates showing that 23% of
global pneumonia cases (around 43 million cases) occur in India
annually [2,3]. Lack of exclusive breastfeeding,
under-nutrition, low birth-weight, overcrowding, lack of
immunization and poor healthcare-seeking behavior are a few of
the leading risk factors for pneumonia in India and other low
and middle-income countries (LMICs) [4,5]. Only one in five
caregivers in the developing world know the two key symptoms of
pneumonia -fast and difficult breathing [6,7]. One of the
recommended critical activities in WHO’s and UNICEF’s Global
Action Plan for the Control of Pneumonia and Diarrhea is
improving health education of the mother by providing
community-based interventions (CBI) [8,9]. Our study was
conducted to determine the effect of behavior change
communication (BCC) activities directed at mothers in reducing
the incidence of childhood pneumonia.
METHODS
An open-label cluster randomized control
trial was conducted between December, 2015 and March, 2018 in
Pune and Sangli districts of Maharashtra in the urban and rural
field practice area of two medical colleges. Approval was
obtained from institutional ethics committee, and written
consent from the mothers was obtained prior to the enrolment.
Based on the reported incidence of childhood
pneumonia of 0.2-0.5 per child per year in under-five children
[10], and assuming the coefficient of variation (k) to be 0.4,
the sample size was calculated as 15 clusters.The study enrolled
sixteen clusters to cover for unforeseen eventualities
precluding the BCC activities in any cluster.
A cluster was defined as one of the 45
notified slums or revenue villages in the field practice area of
the two medical colleges. The 45 eligible clusters were first
stratified into two districts, further into urban and rural
clusters, urban clusters were stratified based on the East or
West. The rural clusters were stratified based on the primary
health center (PHC). These clusters were then randomized in to
intervention and control arms, based on a computer-generated
randomization schedule and two clusters per site were randomly
selected, thus 16 clusters were included. Participants were
under-five children and their mothers from the households in the
selected clusters (Web Fig.1).
Families residing for more than six months
with under-five children were included in the study. All the
under-five children and their mothers (including expectant
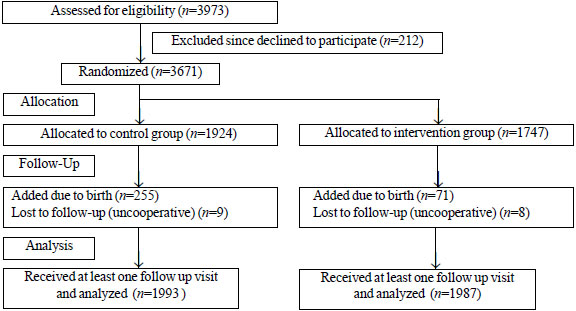
mothers) were enrolled as study participants. Fig. 1
shows the participant flow diagram. The new births were enrolled
throughout the trial period ensuring that they receive at least
nine months of surveillance. We excluded those children who
completed five years of age during the surveillance period from
further visits. All the children who had received at least one
follow-up visit were analyzed. The literacy status of the mother
was reported as per the census definition [11]. Ventilation
status of the house was assessed using the availability of per
capita floor space [12]. Due to the nature of the intervention
provided, allocation concealment and masking were not possible
after randomization.
 |
|
Fig. 1 Study flow chart.
|
The total study period included the following
phases: preparatory (2 months), baseline survey and enrollment
(3 months), intervention (4 months), and surveillance (12
months).
The components of the BCC activities for the
mothers in the intervention arm consisted of imparting knowledge
about child feeding, including the importance of feeding of
colostrum, exclusive breastfeeding till six months of age,
gradual introduction of food from the age of six months, causes
of malnutrition among children, the importance of taking weight
and plotting of growth charts in anganwadi; imparting knowledge
about steps to prevent pneumonia in their children, such as
complete immunization, prevention of indoor air pollution, the
practice of cough etiquettes; hand hygiene including occasions
and steps of hand wash; and, providing information about the
signs and symptoms of pneumonia.
The BCC intervention was administered by
trained field supervisors to an invited group of 8-10 mothers at
a time, in an interactive manner using a validated mothers’
booklet, and a hand wash demonstration. The second BCC activity
was imparted by screening an audio-visual film for a larger
group of 15-20 mothers and virtual hand wash demonstration.
These two BCC activities were separated by a gap of two months.
ASHAs and anganwadi workers were involved in planning and
coordinating the BCC activities, thereby ensuring maximum
cooperation of the mothers. The third BCC or continued
intervention, through the house-to-house visit, was done three
months after the second BCC activity by using flashcards. A
total of eight trained field supervisors were involved in
imparting the BCC activities, under supervision of the site
investigators. Routine care under the national health program
was continued in both the arms of the study.
The primary outcome was the incidence of
pneumonia. Trained doctors confirmed the episode of pneumonia
using WHO Integrated management of neonatal and childhood
illnesses (IMNCI) guidelines [13]. The outcome was assessed by
fortnightly visits conducted for one year by the respective
ASHAs of each cluster, except in Pune (urban), where anganwadi
workers enquired about the current status of the child’s health
from the mother during the house-to-house surveillance visits.
For labeling a new episode of pneumonia in the same child, a
symptom-free period of a minimum of 14 days was considered
essential, otherwise, it was presumed to be continuation of the
preceding episode [14]. Besides, information about other
illnesses and death among under-five children was collected by
the field supervisors.
Quality checks were done randomly by site
investigators and field supervisors. Site investigators
conducted once-a-week field visits or as and when a case of
pneumonia was suspected. For data entry, the critical fields in
the tools were identified as a proxy to completeness and
accuracy – discrepancy up to 0.1% and 1%, respectively were
considered acceptable. Additionally, alternate forms were
physically cross-checked for discrepancies related to data
entry.
Statistical analysis: Intention to treat
analysis was done to analyze the incidence of pneumonia (as
episodes per child per year follow-up) in the intervention and
control arm. The relative risk was calculated to compare the
incidence between two arms. P value <0.05 was considered
statistically significant.
RESULTS
Sixteen clusters were randomly selected out
of the 45 clusters, eight were in the intervention arm, and
eight were in the control arm i.e., four in each urban and rural
area of the two districts. The under-five children enrolled in
the intervention arm were 1747 (20.1% aged <1 year) and in the
control arm 1924 (20.8% aged <1 year) (Fig. 1). A total
of 39 391 fortnightly follow-up visits were conducted in
intervention and 40 288 in the control arm during one year.
Baseline household and other demographic characteristics were
similar between the arms except for higher unclean fuel use in
control arm (20.1% vs 10.3%; P<0.05). Information related
to the child was obtained from the mothers i.e., exclusive
breast feeding for children between 6-12 months, primary
immunization for children between 12-24 months, birthweight for
children up to 6 months of age etc., hence the denominators
varied as per the number of mother-child in that group (Table
I).
Table I Baseline Characteristics of Households and Under-Five Children Enroled in the Study
| Characteristics |
Intervention arm
|
Control arm
|
|
n=1448 |
n=1374 |
| Household characteristics |
|
|
| Joint family |
871/1448 (60.2) |
812/1373 (59.1) |
| Hindu religion |
1278/1448 (88.3) |
1166/1374 (84.9) |
| SC/ST caste |
387/1448 (26.7) |
333/1374 (24.2) |
| Literate mother |
1295/1367(95.7) |
1334/1413(94.4) |
| Overcrowdinga |
906/1444(62.7) |
839/1371 (61.2) |
|
Inadequate ventilationb |
1349/1408 (95.8) |
1289/1315 (98.0) |
| Smoking indoor |
33/1442 (2.3) |
52/1368 (3.8) |
|
Unclean fuelc |
149/1448(10.3) |
277/1374(20.2) |
| Child characteristics |
n=1747 |
n= 1924 |
| Male sex |
925/1747(52.9) |
1014/1924(52.7 ) |
| Age (y)d |
2.38 (1.36) |
2.39 (1.37) |
| Birthweight (kg) |
2.51 (0.61) |
2.72 (0.60) |
|
(n=293) |
(n=371) |
|
Received colostrume |
313/330 (94.8) |
333/370 (90.0) |
| Exclusive breast- |
86/172 (46.0) |
111/249 (44.4) |
| feeding till 6 mo |
309/335 (92.2) |
296/304 (97.4) |
|
Fully immunizedf |
|
|
| Nutritional status of the child g |
|
|
| Wasting |
295/1678 (17.5) |
309/1852 (16.7) |
| Stunting |
720/1685 (42.7) |
916/1878 (48.8) |
| Undernutrition |
565/1693 (33.3) |
694/1864 (37.2) |
|
Date presented as number/total number (%). aNumber of
family members per room criteria was used; bInadequate
ventilation was defined as households with less than 100
sq. ft. of floor area per person with, or without a fan;
cUnclean fuel included biomass, coal stove, stove with
kerosene for cooking purposes for most of the days of
the week by the household; dThis information was
collected from mothers of infants upto one year of age
only to remove the possibility of recall bias, and the
intention was to assess the most essential i.e., primary
immunization; eInformation was analyzed for
infants between >6 mo to one year of age only;
fImmunization information was analyzed for children with
cards and aged between 12-23 months. gWHO classification
was used; results presented for <-2SD. Child
characteristics are based on children enrolled during
baseline phase only. |
There were a total of 5505 episodes of
illnesses in the intervention arm and 6436 episodes in the
control arm. Of these, there were 44 and 31 episodes of
pneumonia in the intervention and control arm, respectively,
constituting an incidence of 0.80 and 0.48 episodes of pneumonia
per child per year, respectively in the two arms [RR (95% CI)
1.66 (1.05-2.62); P=0.03]. Three children in the
intervention and two in the control arm had two episodes each.
There was no case of severe pneumonia and very severe disease.
Twenty-six (59.1%) episodes in inter-vention arm and 21 (67.7%)
episodes in control arm were reported in boys [RR (95% CI)
0.87(0.62-1.23); P=0.77]. For 93.2% of pneumonia episodes
in the intervention arm, children were taken to the health care
provider as the first action, in contrast to 54.9% from the
control arm [(RR (95% CI) 5.06 (2.58 to 9.92); P<0.001)]
(Table II). None of the children required hospitalization
for pneumonia in both the arms. There were two deaths reported
in each study arm, unrelated to pneumonia. The number of
pneumonia episodes was highest in the winter season (51%).
Table II Episodes of Common Illnesses in the Intervention and Control Groups
|
Illnesses/action taken |
Intervention arm,
n=1747
|
Control arm, n=1924 |
RR(95% CI) |
P value |
|
Number of |
Incidence |
Number of |
Incidence |
|
|
|
episodes |
(per child per y) |
episodes |
(per child per y) |
|
|
| Total illness
episodes documented /total visits |
5505/39391 |
13.98 |
6436/40288 |
15.97 |
— |
— |
| Pneumonia |
44 |
0.80 |
31 |
0.48 |
1.66 (1.05 to 2.62) |
0.030 |
| Cold/cough
|
2738 |
49.74 |
2770 |
43.0 |
1.15 (1.11 to 1.20) |
<0.001 |
| Diarrhea |
128 |
2.32 |
242 |
3.76 |
0.62 (0.50 to 0.76) |
<0.001 |
| Vomiting |
52 |
0.94 |
88 |
1.37 |
0.69 (0.49 to 0.97) |
0.03 |
|
Contacting a HCPa |
41/44 |
- |
7/31 |
- |
5.06 (2.57 to 9.92) |
<0.001 |
|
Symptoms were assessed from mothers of the
children,only pneumonia was diagnosed using IMNCI
criteria. aContacting a health care provider as a first
action taken in case of pneumonia episodes. |
Out of all the episodes of illness, diarrhea
contributed to 2.32 and 3.76 episodes per child per year in the
intervention and control arm, respectively (P <0.001).
DISCUSSION
Our study shows that the incidence of all
illnesses taken together, was significantly less with BCC
intervention. The low incidence of pneumonia in both the arms of
the study was comparable to that reported in South East Asian
countries [10,13]. This low incidence may reflect the fact that
Maharashtra has better health indicators, compared to other
states of India [14]. A three-year follow-up study completed in
2008 in a Southern state of India reported an incidence rate of
0.4 (95% CI=0.3-0.7) in its first year [15]. However, the
incidence of pneumonia in the current study was higher in
children less than one year of age compared to those in 1-5 year
age group, similar to the findings reported by other studies
[16,17].
Like other studies, the fortnightly follow-up
visits in the current study, for one calendar year, took into
account the seasonal variation in the incidence of pneumonia
[18,15]. Possibly, a more extended follow-up period or
revisiting the clusters after a gap of two years might be
required to observe benefits from these activities on health
outcomes [19]. Though the WHO IMNCI tool for confirming
pneumonia lacks specificity, it is the best measure of reporting
pneumonia in children under five years of age [20]. The
possibility of overdiagnosis of pneumonia by non-physician
healthworkers was addressed by confirmation of these episodes by
an expert. The seasonal trend of pneumonia in the current study
was similar to those reported by other studies [15,21,22].
The care-seeking pattern for illness was
similar in both groups with the commonest healthcare provider
contacted being private practitioners. These findings are
similar to other studies in India [23-26]. The current study
reported fewer hospital admissions for pneumonia compared to
other studies in India [15]. It may be due to early case
detection and ambulatory management of pneumonia. Another study
from India had concluded that trust in the public health system
is essential for making the community-based pneumonia management
program successful [27].
The overall morbidity and diarrheal episodes
during follow-up were less than other studies in India [20]. The
incidence of pneumonia was slightly higher in the intervention
than the control arm, probably reflecting higher reporting by
mothers about illness episode in their children in the
intervention arm than in the control arm. There were
significantly fewer diarrhea episodes in the intervention arm
than in the control arm.
The current study has the potential for
generalizability as the community health workers i.e., ASHA and
anganwadi workers, were involved in surveillance visits.
Routinely, ASHA and Anganwadi workers deliver incentive-based
maternal and child health - related work, but in this trial,
they received surveillance-related training, enabling them to
timely identify sickness in a child as recommended by WHO [28].
It also helped to gain cooperation from mothers and other family
members. However, external validity is limited to states with
similar health parameters. BCC may be valuable in states with
high under-five mortality, but further studies need to be
conducted in these states. The limitation of the present study
was a relatively short follow-up duration, which may be
inadequate to observe the impact of BCC activities.
BCC alone is unlikely to be effective for the
reduction of the incidence of pneumonia. The reduction in the
incidence of pneumonia is influenced by factors such as economic
status, birthweight, overcrowding, joint family, type of fuel,
etc. So, intervention in the form of BCC activity may need
support of additional strategies to reduce the incidence of
pneumonia.
Acknowledgments: Dr Nandini Malshe for
her technical inputs. Mrs. Aruna Deshpande, Mr Sane, Statistical
consultant; Mrs. Mahima Dwivedi and Dr. Supriya Phadnis, Project
coordinators for their inputs in project implementation and
report compilation; Dr. V N Karandikar, Ex-Director Health
Sciences of Bharati Vidyapeeth University Pune; Dr. Manoj Das,
INCLEN Trust International for technical guidance.
Ethics clearance: Bharati Vidyapeeth
Deemed University Institutional Ethics Committee; No.
ECR/313/Inst/MH/2013/RR-16 dated February 16, 2015. Bharati
Vidyapeeth Deemed University Medical College and Hospital IEC,
Sangli; No. ECR/276/Inst/MH/2013/RR-16 dated March 01, 2015.
Contributors: JG, PD, PP, GD, SL:
conceptualization; JG, PP, GD: data curation; JG, PP, GD, PD:
formal analysis; JG, SK, PD: funding acquisition; JG, PD, PP,
GD: methodology; JG, GD, PP, SP: project administration; SL, JG,
PD: resources; PP, VW: software; SQ, SM, RP, VW, RD, KR, SP:
supervision; JG, PD, SL: validation; JG, PP: writing – original
draft preparation; JG, PD: Writing – review and editing. All
authors approved the final version of manuscript, and are
accountable for all aspects related to the study.
Funding: This work was supported by Bill
and Melinda Gates Foundation through The INCLEN Trust
International (Grant number: OPP1084307). The funding source had
no contribution in study design, implementation, collection and
interpretation of data and report writing. Competing
interest: None stated.
Note: Additional material related
to this study is available with the online version at
www.indianpediatrics.net
| |
|
WHAT IS ALREADY KNOWN?
• Behavior change communication (BCC)
interventions, alongwith efforts towards improving the
immunization status of children and breastfeeding
promotion, are documented to be efficient,
cost-effective, and sustainable interventions in
reducing the burden of childhood pneumonia.
WHAT THIS STUDY ADDS?
• BCC intervention alone, aimed towards mothers, was
not found to be sufficient to reduce the incidence of
pneumonia in under-five children.
|
REFERENCES
1. Million Death Study Collaborators.
Causes of neonatal and child mortality in India: a
nationally representative mortality survey. Lancet.
2010;376:1853-60.
2. Rudan I, O’Brien KL, Nair H, et al.
Epidemiology and etiology of childhood pneumonia in 2010:
Estimates of incidence, severe morbidity, mortality,
underlying risk factors and causative pathogens for 192
countries. J Glob Health. 2013;3:010401.
3. Watt JP, Wolfson LJ, O’Brien KL, et
al. Burden of disease caused by Haemophilus influenzae type
b in children younger than 5 years: Global estimates.
Lancet. 2009; 374:903-11.
4. Farooqui H, Jit M, Heymann DL, Zodpey
S. Burden of severe pneumonia, pneumococcal pneumonia and
pneumonia deaths in Indian states: Modelling based
estimates. PLoS One. 2015;10:1-11.
5. Walker CLF, Rudan I, Liu L, et al.
Global burden of child- hood pneumonia and diarrhoea.
Lancet. 2013; 381:1405-16.
6. Cohen AL, Hyde TB, Verani J, Watkins
M. Integrating pneumonia prevention and treatment
interventions with immunization services in resource-poor
countries. Bull World Health Organ. 2012;90:289-94.
7. Mull DS, Mull JD, Kundi MM, Anjum M.
Mothers’ perceptions of severe pneumonia in their own
children: a controlled study in Pakistan. Soc Sci Med.
1994;38:973-87.
8. Qazi S, Aboubaker S, MacLean R, et al.
Ending preventable child deaths from pneumonia and diarrhoea
by 2025. Development of the integrated global action plan
for the prevention and control of pneumonia and diarrhoea.
Arch Dis Child. 2015;100:S23-8.
9. Van Ginneken JK, Lob Levyt J, Gove S.
Potential interventions for preventing pneumonia among young
children in developing countries: promoting maternal
education. Trop Med Int Health. 1996;1:283-94.
10. Ghimire M, Bhattacharya SK, Narain
JP. Pneumonia in South-East Asia region: Public health
perspective. Indian J Med Res. 2012;135:459-68.
11. Government of India. Census of India
2011 [Internet]. Accessed October 5, 2020. Available from:
https://censusindia.gov.in/2011-common/censusdata2011.html
12. Park K. Park’s Textbook of Preventive
and Social Medicine. 24th ed. Banarasidas Bhanot publishers;
2017. p.775-76.
13. Rudan I, Tomaskovic L, Boschi-Pinto
C, Campbell H. Global estimate of the incidence of clinical
pneumonia among children under five years of age. Bull World
Health Organ. 2004;82:895-903.
14. Ram F, Paswan B, Singh SK, et al.
Improvements in maternal health in India: Evidence from
NFHS-4 ( 2015-16). Demography India. 2016; 43.
15. Gladstone BP, Das AR, Rehman AM.
Burden of illness in the first 3 years of life in an Indian
slum. J Trop Pediatr. 2010;56:221-6.
16. Bari A, Sadruddin S, Khan A. Cluster
randomized trial of community case management of severe
pneumonia with oral amoxicillin in children 2-59, Pakistan.
Lancet. 2011; 378:1796.
17. Luby SP, Agboatwalla M, Feikin DR,
Painter J, Billhimer W, Altaf A, et al. effect of
handwashing on child health: A randomized controlled trial.
Lancet. 2005;366:225-33.
18. Lanata CF, Rudan I, Boschi-Pinto C,
et al. Methodological and quality issues in epidemiological
studies of acute lower respiratory infections in children in
developing countries. Int J Epidemiol. 2004;33:1362-72.
19. Boone P, Elbourne D, Fazzio I, et al.
Effects of community health interventions on under-5
mortality in rural Guinea-Bissau (EPICS): A
cluster-randomized controlled trial. Lancet Glob Health.
2016;4:e328-35.
20. Mortimer K, Ndamala CB, Naunje AW, et
al. A cleaner burning biomass-fuelled cookstove intervention
to prevent pneumonia in children under 5 years old in rural
Malawi (the Cooking and Pneumonia Study): A cluster
randomized controlled trial. Lancet. 2017;389:167-75.
21. Montella S, Corcione A, Santamaria F.
Recurrent pneumonia in children: A reasoned diagnostic
approach and a single centre experience. Int J Mol Sci.
2017;18:296.
22. Smith KR, Samet JM, Romieu I, Bruce
N. Indoor air pollution in developing countries and acute
lower respiratory infections in children. Thorax.
2000;55:518-32.
23. Minz A, Agarwal M, Singh JV, Singh
VK. Care seeking for childhood pneumonia by rural and poor
urban communities in Lucknow: A community-based
cross-sectional study. J Family Med Primary Care. 2017;6:
211-7
24. Soni A, Fahey N, Phatak AG, et al.
Differential in healthcare-seeking behavior of mothers for
themselves versus their children in rural India: Results of
a cross sectional survey. International Public Health
Journal. 2014;6:57.
25. Bhandari N, Mazumder S, Taneja S,
Sommerfelt H, Strand TA. Effect of implementation of
Integrated Management of Neonatal and Childhood Illness
(IMNCI) programme on neonatal and infant mortality: cluster
randomized controlled trial. BMJ. 2012;344:e1634
26. Das JK, Lassi ZS, Salam RA, Bhutta
ZA. Effect of community based interventions on childhood
diarrhea and pneumonia: uptake of treatment modalities and
impact on mortality. BMC Public Health. 2013;13:1-0.
27. Awasthi S, Nichter M, Verma T, et al.
Revisiting community case management of childhood pneumonia:
Perceptions of caregivers and grass root health providers in
Uttar Pradesh and Bihar, Northern India. PLoS One.
2015;10:1-18.
28. Revised WHO Classification and Treatment of Pneumonia in
Children at Health Facilities: Evidence Summaries. World Health
Organization; 2014. Accessed on Oct 5, 2020. Avail-able from:
https://www.ncbi.nlm.nih.gov/books/NBK264162/
|
|
|
 |
|

