|
|
|
Indian Pediatr 2020;57:1029-1032 |
 |
Factors Associated With
Mortality in Toxic Encephalopathy Due to Shigellosis in Children
|
|
Machinary Puthenpurayil Jayakrishnan, 1
Madathil Govindaraj Geeta,1
Padinharath Krishnakumar,2
VK Gireeshan,1 Biju George,3
P Prathiksha,4 Govindakarnavar
Arunkumar4 and PM Anitha5
From Departments of 1Pediatrics, 3Community
Medicine and 5Microbiology, Government Medical College,
Kozhikode, Kerala; 2Institute of Mental Health and
Neurosciences (IMHANS), Kozhikode, Kerala; and 4Manipal
Institute of Virology, Manipal Academy of Higher Education (Deemed to be
University), Manipal, Karnataka; India.
Correspondence to: Dr Machinary Puthenpurayil Jayakrishnan,
Additional Professor of Pediatrics, Government Medical College,
Kozhikode, Kerala, India.
Email:
[email protected]
Received: February 21, 2020;
Initial review: February 25, 2020;
Accepted: July 27, 2020.
|
Objective: To study the clinical characteristics
and factors associated with mortality among children with Shigella encephalopathy.
Methods: The data collection was done prospectively from January,
2018 to May, 2019 with retrospective data from June, 2016 to December,
2017. The study cohort consisted of 58 children <12 years of age with Shigella encephalopathy
admitted to the pediatric intensive care unit. Shigella
encephalopathy was confirmed if culture or real time polymerase chain
reaction (PCR) of a stool sample or rectal swab was positive, with
temporal association of diarrhea with seizures, altered sensorium or
both. Association of mortality with risk factors was tested using chi
square test, and the strength of association was estimated in terms of
relative risk (RR) and 95% CI. Results: Seizures and altered
sensorium were the predominant neurological symptoms. Shock occurred in
32 (55%) children, while blood in stools was a feature in only 6 (10%)
children. S. sonnei was the commonest species identified
on stool culture (19;33%). On univariate analysis, prolonged seizures,
shock, prolonged altered sensorium, multi-organ dysfunction,
lymphocytopenia at admission and need for mechanical ventilation were
significantly associated with mortality. On multivariate regression,
delayed presentation (presentation to the hospital 48 hours after the
onset of symptoms) and prolonged altered sensorium (>12 hours) were
found to be independently associated with mortality. Conclusions:
Recognition of factors associated with mortality in Shigella
encephalopathy may assist in better monitoring of sicker children and
improved outcomes.
Keywords: Diarrhea, Ekiri syndrome, Morbidity, Outcome, S.
sonnei.
|
|
S
higellosis continues to be an important cause of
diarrhea-related mortality in developing countries [1,2] with
Shigella flexneri being the predominant species
endemic in India [3]. The most common extra-intestinal
complication in shigellosis is encephalopathy, presenting with
seizures, headache, lethargy, confusion or hallucinations [4].
Over the last few decades, there has been a substantial
reduction in deaths related to shigellosis [5]. Children with
Shigella encephalopathy usually recover without any neuro-logical
deficits [4].
A recent study from Bangladesh has reported
high case fatality in children with Shigella
encephalopathy [6] We have also noticed an increase in mortality
due to Shigella encephalopathy in our center which
prompted us to analyze the hospital records which showed that
there was only one death between 2013 and 2015 (unpublished
data). Lethal toxic encephalopathy or Ekiri syndrome (a severe
form of encephalopathy resulting in rapid prog-ression to coma
and death) is reported in children with shigellosis from abroad
but not from India [7]. The present study aimed to describe the
clinical charac-teristics of Shigella encephalopathy in
children and to identify factors associated with mortality.
METHODS
The study was conducted in the Pediatric
Intensive Care Unit (PICU) of the Government Medical College,
Kozhi-kode, a tertiary referral centre. Children between 1 month
and 12 years of age admitted from 1 June, 2016 to 31 May, 2019
with a diagnosis of Shigella encephalopathy were included
in the study. The data collection was done prospectively from
January, 2018 to May, 2019 with retrospective data from June,
2016 to December, 2017. The study was approved by the
institutional ethics committee.
Shigella encephalopathy was suspected
based on the temporal association of diarrhea with altered
sensorium, seizures or both in children. Stool microscopy and
culture were done in all cases, apart from other investigations
including complete blood count, blood culture, cerebrospinal
fluid analysis and culture, blood sugar, serum electrolytes,
renal and liver function tests. The diagnosis was confirmed if
Shigella spp. was isolated from a stool sample or rectal
swab, or if polymerase chain reaction (PCR) from a stool sample
was positive. Children with a negative stool culture or PCR,
history of seizures poorly controlled with anti-epileptics, and
those whose sensorium improved after correction of shock were
excluded from the study.
The clinical characteristics were recorded
and the factors associated with mortality were studied. The
following definitions were chosen: Delayed presentation:
Presentation to the hospital 48 hours after the onset of
symptoms; Undernutrition: weight for age or weight for height
below –2 z-scores on the WHO child growth standards; Fluid
refractory shock: persistent shock despite administration of 60
mL/kg of fluid in first hour or development of fluid overload
features like hepato-megaly or lung crepitations; Multi organ
dysfunction: dysfunction of 2 or more organ systems other than
the CNS; Prolonged seizure: seizures lasting for more than 30
minutes without the child regaining consciousness in between;
Prolonged altered sensorium: altered sensorium lasting more than
12 hours; Hyponatremia: serum sodium concentration less than 135
mmol/L; Hypocalcemia: serum ionized calcium less than 1.1 mmol/L;
Lymphocyto-penia: Lymphocyte count below the normative value for
the corresponding age.
All children were treated with ceftriaxone
and other supportive measures, which included management of
seizures and raised intracranial tension. Indications for
mechanical ventilation included worsening respiratory failure,
refractory shock and a score on the Glasgow coma scale of <8.
Seizures were managed in accordance with the unit protocol which
included a benzodiazepine, followed by fosphenytoin and
levetiracetam or sodium valproate, depending on the response.
Hypertonic saline (3%) was used as therapy for raised
intracranial tension. Shock was managed as per standard
protocol, including fluid boluses and inotropic support in fluid
refractory shock. Appropriate intravenous fluids were used for
rehydration and replacement of ongoing losses.
Statistical analysis: Qualitative
variables were summarised as frequency and percentages and
associa-tion of mortality with risk factors were tested using
chi square test. A P value of <0.05 was considered to be
statistically significant. Strength of association of risk
factors with mortality was estimated in terms of relative risk
(RR) and its 95% confidence interval (95% CI). A multivariate
logistic regression was done to find out adjusted odds ratio of
the variables. Those variables which were found to be
significant on univariate analysis were selected for modeling
using binary logistic regre-ssion to obtain an adjusted OR and
its 95% CI. Statistical analysis was performed using SPSS V.16
(SPSS, Chicago, Illinois, USA).
RESULTS
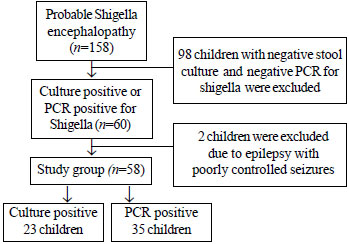
Out of 158 probable cases, Shigella
encephalopathy was confirmed in 60 children (Fig. 1).
Among them, 2 children had epilepsy with poorly controlled
seizures and were not included for the analysis. The final
sample consisted of 58 children with confirmed
shigella encephalopathy. The prospective and retrospective data
included 40 and 18 children, respectively (27 girls, age range
38 days-12 years). Stool culture was positive for shigella in 23
(40%) children while the rest had stool PCR positive for
Shigella spp.
 |
|
Fig.1 Study flow chart.
|
Nearly half (48%) of the diarrheal episodes
occurred during the months of May and June. All except 5
children (53; 91%) were admitted to the PICU within 48 hours,
and 45 (78%) of them on the first day of illness itself. The
initial symptom was fever in 54 (93%) children and seizures,
loose stools, vomiting and abdominal pain in one child each.
Seizures and altered sensorium were the predominant neurological
symptoms. Altered sensorium or seizures preceded loose stools in
16 (28%) children, while the majority (42, 72%) developed
features of encephalopathy after the onset of loose stools (Table
I). S. sonnei was the commonest organism
identified in stool culture (33%) followed by S.boydii
(3%) and S. flexneri (2%). Blood culture was sterile
in all cases.
Table I Clinical and Laboratory Characteristics of Children With Shigella Encephalopathy (N=58)
| Characteristic |
No (%) |
| Fever as initial symptom |
54 (93) |
| Seizures |
51 (88) |
| Prolonged seizure (lasting >30 min) |
10 (17) |
|
Altered sensorium
|
27 (47) |
|
Prolonged altered sensorium (lasting >12 h)
|
21 (36) |
| Headache |
3 (5) |
| Blood in stools |
6 (10) |
| Shock |
32 (55) |
| Fluid-refractory shock |
25 (43) |
| Lymphocytopenia |
37 (64) |
| Hypocalcemia |
12 (21) |
| Hyponatremia |
28 (48) |
| Need for mechanical ventilation |
13 (22) |
| Multi-organ dysfunction |
11 (19) |
The mortality in the present sample was 26%.
More than half (9;60%) of the children who died were below the
age of 5 years. Death occurred within 24 hours of
hospitalization in (4, 27%) children and within 48 hours in 7
(47%) children. All 5 children who were admitted after 48 hours
of onset died.
Among the children who died, prolonged
altered sensorium occurred in 13 (87%), while 7 (47%) children
had prolonged seizures. All the 13 children who had persistent
low scores of <8 on the Glasgow coma scale died. Severe
metabolic acidosis in the absence of shock or kidney injury was
a feature in 2 (3%) children, and global developmental delay
were present in 4 (7%) children. Computed tomography scans of
the brain in two children and autopsy in one child showed severe
cerebral edema. Stool culture for S. Sonnei was positive
in 3 children who died.
On univariate analysis, prolonged seizures,
admission to PICU after 48 hours of onset, shock, prolonged
altered sensorium, persistently low score on the Glasgow coma
scale, hyperglycemia at admission, multi - organ dysfunction,
need for mechanical ventilation and lymphocytopenia at admission
were significantly associated with mortality. On multivariate
regression, delayed presentation to the hospital more than 2
days after the onset of any symptoms and altered sensorium for
>12 hours were found to be independently associated with
mortality (Table II).
Table II Risk Factors for Mortality in Shigella Encephalo-pathy in Children (N=15)
| Variables |
Adjusted OR (95% CI) |
P value |
| Prolonged altered sensorium (n=13) |
18.23 (2.27 to 16.13) |
0.006 |
| Hyperglycemia (n=4)* |
1.43 (0.09 to 21.16) |
0.79 |
| Shock (n=13) |
4.64 (0.41 to 52.47) |
0.22 |
| Hyponatremia (n=5)* |
0.46 (0.07 to 3.06) |
0.42 |
| Undernutrition (n=2) |
13.13 (0.01 to 17042.92) |
0.48 |
| Lymphocytopenia (n=5)* |
0.22 (0.03 to 1.61) |
0.14 |
| Delayed
presentation (n=5) |
8.74 (1.02 to
74.96) |
0.05 |
|
*at admission. |
DISCUSSION
We studied the clinical characteristics and
mortality in 58 children with Shigella encephalopathy
during a period of three years. More than a quarter of the
children died, possibly due to the occurrence of lethal toxic
encephalo-pathy. Lethal toxic encephalopathy or Ekiri syndrome,
first reported from Japan is a rapidly progressing fulminant
encephalopathy associated with shigellosis in children [7-8]. In
the present sample, children who died had a similar progress of
encephalopathy with death occurring within 48 hours of the onset
of the disease in 47% of cases.
The cause of death in lethal toxic
encephalopathy is not yet well understood, although severe
cerebral edema has been described and it is suggested that
prevention will help to improve the outcome [7,9]. Entry of
inflammatory cytokines into the brain in susceptible children,
might be the reason for severe encephalopathy [10]. Our findings
are also suggestive of the role of cerebral oedema.
In a large series from Israel, a
disproportionate number of cases had developmental delay and
intellectual disability, suggesting a possible increased
susceptibility [9], though, we could not confirm the
association. Although hypocalcemia and hyponatremia have been
reported in children who died due to encephalopathy, they were
not significantly associated with mortality in our series [7,9].
S sonnei was the commonest serogroup
isolated in our series, although S flexneri has been
reported as the most common serogroup in India [11-13]. Recent
studies have reported increasing incidence of S sonnei
infections in this region [14]. A shift towards S sonnei
has been observed in other countries as socioeconomic conditions
improve [15]. A significant association of S sonnei with
encephalopathy has been reported earlier, suggesting increased
virulence and might partly explain the increased mortality [6].
Delayed presentation and prolonged altered
senso-rium were found to be independently associated with
mortality, suggesting that timely initiation of antibiotics
shortens the duration of illness and results in bacterio-logical
clearance, as reported in literature [16]. One limitation of the
present study is that the exact cause of rapidly progressing
encephalopathy leading to death could not be identified in all
children since we could not carry out brain imaging studies in
all children and autopsy could be done in one child only.
The increased mortality in shigella
encephalopathy in the present sample underscores the need for
further studies on the changing virulence of Shigella
organisms, as well as host-specific risk factors and optimal
treatment.
Ethics Clearance: Institutional
ethics committee of the Government Medical College, Kozhikode;
No. GMCKKD/RP2018/IEC/15, dated 11 January, 2018.
Contributors: MPJ: designed study,
collected the data and wrote the initial draft of the paper;
MGG, PK: helped in writing the manuscript and interpretation of
the data; VKG: patient management and helped in collection of
the data; BG: expert in statistics who did the statistical
analysis; PP, GA, PMA: conducted microbiological analysis.
Funding: None; Competing interest:
None stated.
|
|
What This Study Adds?
•
Delayed presentation more than 48 hours after the
onset, and prolonged altered sensorium beyond 12 hours
were the risk factors identified for mortality in
Shigella encephalopathy in children.
|
REFERENCES
1. Troeger C, Blacker BF, Khalil IA, Rao PC,
Cao S, Zimsen SR, et al. GBD 2016 Diarrhoeal Disease
Collaborators. Estimates of the global, regional, and national
morbidity, mortality, and etiologies of diarrhea in 195
countries: A systematic analysis for the Global Burden of
Disease Study 2016. Lancet Infect Dis. 2018;18:1211-8.
2. Khalil IA, Troeger C, Blacker BF, Rao PC,
Brown A, Atherly DE, et al. Morbidity and mortality due
to shigella and enterotoxigenic Escherichia coli diarrhoea: The
Global Burden of Disease Study. 1990-2016. Lancet Infect Dis.
2018;18:1229-40.
3. Taneja N, Mewara A Shigellosis:
Epidemiology in India. Indian J Med Res. 2016;143: 565-76.
4. Ashkenazi S, Dinari G, Zevulunov A, Nitzan
M. Convulsions in childhood shigellosis: Clinical and laboratory
features in 153 children. Am J Dis Child. 1987; 141:208-10.
5. Bardhan P, Faruque AS, Naheed A, Sack DA.
Decrease in shigellosis-related deaths without Shigella
spp.-specific interventions, Asia. Emerg Infect Dis.
2010;16:1718-23.
6. Afroze F, Ahmed T, Sarmin M, Smsb Shahid
A, Shahunja KM, ShahrinL, et al. Risk factors and outcome
of Shigella encephalopathy in Bangladeshi children. PLoS Negl
Trop Dis.2017;11:e0005561.
7. Pourakbari B, Mamishi S, Kohan L, Sedighi
L, Mahmoudi S, Fattahi F, et al. Lethal toxic
encephalopathy due to childhood shigellosis or Ekiri syndrome. J
Microbiol, Immunology and Infection. 2012;45:147-50.
8. Sakamoto A, Kamo S. Clinical, statistical
observations on ekiri and bacillary dysentery; a study of 785
cases. Ann Paediatr. 1956;186:1-18.
9. Goren A, Freier S, Passwell JH. Lethal
toxic encephalo-pathy due to childhood shigellosis in a
developed country. Pediatrics. 1992;89:1189-93.
10. Yuhas Y, Weizman A, Ashkenazi S.
Bidirectional concentration-dependent effects of tumor necrosis
factor alpha in Shigella dysenteriae-related seizures. Infection
and immunity. 2003;71:2288- 91.
11. Mandal J, Ganesh V, Emelda J, Mahadevan
S, Parija SC. The recent trends of shigellosis: A JIPMER
perspective. J Clin Diagn Res. 2012; 6:1474-7.
12. Ballal M, Devadas SM, Chakraborty R,
Shetty V. Emerging trends in the etiology and antimicrobial
susceptibility pattern of enteric pathogens in rural Coastal
India. Int J Clin Med. 2014;5:425-32.
13. Tejashree A, Vijaykumar GS, Rao R, Mahale
RP, Gopala-krishnan R, Ponna Y. Spectrum of enteric pathogens in
a tertiary hospital. Transworld Med J. 2013;1:69-73.
14. Madhavan A, Balakrishnan S, Vasudeva
panicker J. Anti-biotic susceptibility pattern of Shigella
isolates in a tertiary healthcare center.J Lab Physicians.
2018;10:140-4.
15. Vinh H, Nhu NT, Nga TV, Duy PT, Campbell
JI, Hoang NV, et al. A changing picture of shigellosis in
Southern Vietnam: Shifting species dominance, antimicrobial
susceptibility and clinical presentation. BMC Infect Dis.
2009;9:204
16. Christopher PR, David KV, John SM,
Sankarapandian V. Antibiotic therapy for Shigella dysentery.
Cochrane Database Syst Rev. 2010;8:CD006784.
|
|
|
 |
|

