|
|
|
Indian Pediatr 2020;57:1023-1025 |
 |
The Association Between
Environmental Lead Exposure and Recurrent Respiratory Infections
in Children Aged 3-7 Years in Shenyang, China
|
|
Xue-Ning Li, 1,2 Ying Liu,2
Na Huang,2 Xiao-Jun Cheng
2 and Li-Hong Jia1
From 1Department of Child and Adolescent Health, School of Public
Health, China Medical University; and 2Department of Pediatrics, The
Fourth Affiliated Hospital of China Medical University; Shenyang,
Liaoning, People’s Republic of China.
Correspondence to: Dr Li-Hong Jia, Professor, Department of Child and
Adolescent Health, School of Public Health, China Medical University,
Shenyang 110122, Liaoning, People’s Republic of China.
Email: [email protected]
Received: September 17, 2019;
Initial review: December 30, 2019;
Accepted: July 13, 2020.
|
Objectives:To investigate the lead exposure
levels, and the effect of blood lead level (BLL) on recurrent
respiratory infections in children aged 3-7 years in Shenyang.
Methods: A case-control study including 78 children with recurrent
respiratory infections and 141 controls was performed. Venous blood was
obtained for BLL, and a questionnaire was completed. Results: The
BLL was significantly higher in children with recurrent respiratory
infections than that in the control group [Median (IQR): 2.56
(1.29-6.19) vs 1.99 (0.90-5.92) µg/dL, P=0.029]. Children
with BLL
ł1.95
µg/dL were more likely to be suffering from recurrent respiratory
infections (OR=2.328, 95%CI=1.228-4.413) than those with BLL <1.95 µg/dL.
Conclusions: High lead level can increase the risk of respiratory
infections in preschool children.
Keywords: Humoral immunity, Lead toxicity, Predisposition,
Risk Factors.
|
|
Lead is harmful to children’s health because
of the dysfunction of various organ systems induced by lead,
such as hematological, neurological, gastrointestinal, central
nervous, renal and immune systems [1,2]. Studies showed that
people exposed to occupational lead had impaired congenital and
humoral immune responses and increased susceptibility to chronic
infection [4,5]. However, there is little information about the
effect of non-occupational lead exposure on humoral immunity.
At least 6% of children under 6 years old
suffer from recurrent respiratory infections (RRI). We studied
the blood lead and immunoglobulin levels among children aged 3
to 7 years in present study to study its relation with RRI.
METHODS
The study was done between September, 2017
and October, 2018. A case-control study was carried out in
children aged 3 to 7 years. Among children diagnosed with RRI,
78 were chosen randomly from the inpatient department of our
hospital, and the control group was 141 healthy children of
matched age and gender who were chosen randomly from the
physical examination center of the same hospital. Exclusion
criteria for both case and control group were taking zinc,
calcium, iron, vitamin A, vitamin D, or multivitamin
supplementation in past 3 months; history of congenital
malformation, such as heart disease and thoracic deformity; and
history of disease associated with kidney, liver or immune
system.
Ethics approval was granted by the institute
ethics committee and informed written consent was obtained from
the parents/caretakers of the participants. Parents/ caretakers
of 219 participants completed a questionnaire, including child’s
age, sex, BMI (kg/m 2),
passive smoking and social economic status (low, middle, high
income). If anyone in the family was smoking currently, it was
defined as passive smoking. Children’s medical histories were
reviewed in particular with regard to the frequency of upper
respiratory infections (cold, pharyngitis, laryn-gitis,
tonsillitis, otitis media) and lower respiratory infec-tions (tracheitis,
bronchitis, bronchiolitis, pneumonia). RRI was defined as either
upper respiratory infections at least six times within one year;
or lower respiratory infections at least two times within one
year [7].
The sample size was calculated according to
the assumptions that alpha of 0.05, power of 0.8, odds ratio
2.5, and prevalence of exposure (lead poisoning) in the control
group 20% [8]. The result was 77 children in the case group and
139 children in the control group.
Blood samples were collected in lithium
heparin coated trace-metal free tubes and were transported on
ice to Shenyang Harmony Health Medical Laboratory for analysis.
Blood lead level (BLL) was determined by atomic absorption
spectrometry through graphite furnace ionization techniques.
Since BLLs were non-normally distributed,
statistical analysis was performed after logarithmic
transformation. Student t-test and analysis of variance test
(ANOVA) were used to evaluate the differences of indicators
between different groups. Categorical variables were compared by
chi-square test and Fisher’s exact test. BLLs was categorized
into two groups (<1.95 µg/dL and
ł1.95 µg/dL)
for multiple logistic regression analysis. Data were analyzed by
Statistical Package for the Social Sciences (SPSS 20.0). The
results were considered statistically significant at 5%.
RESULTS
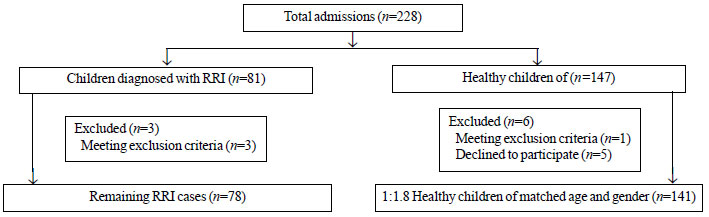
A total of 228 children were approached, of
which, 5 refused to complete a questionnaire, while 4 met one of
the exclusion criteria. The case-control study eventually
included 78 children with RRI and 141 healthy controls (Fig.
1). The percentage of passive smoking exposure was
significantly lower in the control group than that of the case
group (41.1% vs 56.4%; P=0.03) (Table I).
The median (IQR) BLL of case group was significantly higher than
that of the control group [2.56 (1.29-6.19) vs 1.99
(0.90-5.92) µg/dL; P=0.029]. Children with BLL
ł1.95 µg/dL
were more likely to be suffering from RRI, which was
approximately 2.5 times more than those who had BLL <1.95 µg/dL.
Table I Baseline Characteristics of Children With Recurrent Respiratory Infections and Controls
| Characteristics |
Control group
|
Cases |
|
(n=141) |
(n=78) |
| Child age |
|
|
| 36-47 mo |
51 (36.2) |
28 (35.9) |
| 48-59 mo |
31 (22.0) |
26 (33.3) |
| 60-71 mo |
22 (15.6) |
17 (21.8) |
| 72-84 mo |
37 (26.2) |
7 (9.0) |
| Male gender |
67 (47.5) |
39 (50.0) |
| Passive smoking* |
58 (41.1) |
44 (56.4) |
| Socio economic status |
|
|
| Low income |
32 (22.7) |
15 (19.2) |
| Middle income |
103 (73.0) |
57 (73.1) |
| High income |
6 (4.3) |
6 (7.7) |
|
All values in no. (%) except #mean (SD); All P>0.5
except *P=0.03. |
 |
|
Fig.1 Flow of participants in
the study.
|
Multivariate analysis of risk factors for
recurrent respiratory infections showed that both passive
smoking [OR (95% CI)=1.18 (0.98-3.20); P=0.057] and BLL
of 1.95 µg/dL or higher [OR (95% CI) = 2.33 (1.23-4.41); P=0.010]
had a higher risk of having recurrent respiratory infections.
DISCUSSION
Environmental lead exposure has always been
one of the important public health issues in children, even at
chronically low levels [5].
A value of 5 µg/dL US Centers for Disease
Control and Prevention reference concentration) was considered
as the clinical cut off for elevated BLLs [12]. This study show
that the BLLs below 5 µg/dL are associated with an increased
risk of RRI in preschool children. In addition, we observed that
IgG levels of case group were lower than that of the control
group, but the difference between these two groups was not
significant (data not shown), which may be related to relatively
small number of cases. The result also suggests that lead
exposure may increase the risk of RRI by other means, such as by
affecting cellular immunity. However, cellular immune indicators
were not studied in the present study.
Previous studies [4,13,14] have shown that
blood lead can affect the levels of immune cytokine, for
example, reducing the production of IgG and IgM. The effects of
lead on immune cytokine and other adverse health are highly dose
dependent. At present, the immunologic effects from low blood
lead exposure (under 5 µg/dL) were poorly understood. The
present study found that higher BLLs ( ł1.95
µg/dL) increased the risk of RRI in preschool children, as also
observed by other researchers [5]. In addition to lead exposure,
some studies reported the association between other factors and
RRI, such as socioeconomic status, passive smoking, air
pollution, micronutrient intake of children [15,16]. Smokers
often avoid children due to the increasing awareness of smoking
harmfulness. So our results did not show a significant
association between passive smoking and RRI.
Our findings highlight a potentially
preventable cause of infectious disease in preschool-age
children, findings indicate that it is necessary to control the
source of lead pollution, and the harmful effects of apparently
low levels of blood lead need to be further explored.
Ethics approval: The Fourth
Affiliated Hospital of China Medical University; No.
EC-2018-KS-053; dated December 17, 2018.
Contributors: X-NL: collection of data,
study concept, analysis of data, revision of the manuscript; YL:
collection of data, electronic preparation, revision of the
manuscript, NH: collection of data, electronic preparation,
revision of the manuscript; X-JC: collection of data and
electronic preparation; LHJ: study concept, analysis of data,
final revision.
Funding: National Natural Science
Foundation of China (project number 81673190).
Competing interest: None stated.
|
What This Study Adds?
• Blood lead levels >1.95 µg/dL may increase the risk
of recurrent respiratory infections in preschool
children.
|
REFERENCES
1. Cabral M, Toure A, Garçon G, Diop C,
Bouhsina S, Dewaele D, et al. Effects of environmental
cadmium and lead exposure on adults neighboring a discharge:
Evidences of adverse health effects. Environ Pollut. 2015;
206:247-55.
2. Geier DA, Kern JK, Geier MR. A
cross-sectional study of the relationship between blood lead
levels and reported attention deficit disorder: An assessment of
the economic impact on the United States. Metab Brain Dis.
2018;33: 201-8.
3. Li MM, Cao J, Xu J, Cai SZ, Shen XM, Yan
CH. The national trend of blood lead levels among Chinese
children aged 0-18 years old, 1990-2012. Environ Int.
2014;71:109-17.
4. Undeger U, Basaran N, Canpinar H, Kansu E.
Immune alterations in lead-exposed workers. Toxicology. 1996;
109:167-72.
5. Krueger WS, Wade TJ. Elevated blood lead
and cadmium levels associated with chronic infections among
non-smokers in a cross-sectional analysis of NHANES data.
Environ Health. 2016;15:16.
6. Bozzetto S, Pirillo P, Carraro S, Berardi
M, Cesca L, Stocchero M, et al. Metabolomic profile of
children with recurrent respiratory infections. Pharmacol Res.
2017;115: 162-7.
7. Subspecialty Group of Respiratory
Diseases; Society of Pediatrics, Chinese Medical Association.
Clinical Concept and Management of Recurrent Respiratory Tract
Infections in Children (revised). Zhonghua Er Ke Za Zhi.
2008;46: 108-10.
8. Ren HM, Wang JD, Wang GP, Zhang XL, Wang
CM. Influence of soil lead upon children blood lead in Shenyang
City. Huan Jing Ke Xue. 2005;26:153-8.
9. Wang C, Ouyang H, Wang J, Liu J, Zhang X,
Wang Y. Impact of lead pollution in environment on children’s
health in Shenyang City. Huan Jing Ke Xue. 2003;24:17-22.
10. Jacob B, Ritz B, Heinrich J, Hoelscher B,
Wichmann HE. The effect of low-level blood lead on hematologic
parameters in children. Environ Res. 2000;82:150-9.
11. Karmaus W, Brooks KR, Nebe T, Witten J,
Obi-Osius N, Kruse H. Immune function biomarkers in children
exposed to lead and organochlorine compounds: A cross-sectional
study. Environ Health. 2005;4:5.
12. Health NC for E. CDC-Lead-Standard
Surveillance Definitions and Classifications. Available from:
https://www.cdc.gov/nceh/lead/date/definitons.htm. Accessed
December 14, 2018.
13. Sun L, Hu J, Zhao Z, Li L, Cheng H.
Influence of exposure to environmental lead on serum
immunoglobulin in preschool children. Environ Res.
2003;92:124-8.
14. Baţaran N, Undeger U. Effects of lead on
immune parameters in occupationally exposed workers. Am J Ind
Med. 2000;38:349-54.
15. Hai-Feng LI, Yan Z, Pei-Gang J, Hong-Xing
J. Risk factors for recurrent respiratory infections in
preschool children in China. Iran J Pediatr. 2014;24:14-22.
16. Mathew JL, Patwari AK, Gupta P, Shah D,
Gera T,Gogia S, et al. Acute respiratory infection and
pneumonia in India: A systematic review of literature for
advocacy and action: UNICEF-PHFI series on newborn and child
health, India. Indian Pediatr. 2011;48:191-218.
|
|
|
 |
|

