|
|
|
Indian Pediatr 2018;55:966 -968 |
 |
Evaluating Neonates
With Antenatal Hyderonephrosis Using a Standard Protocol: An
Audit of Hospital Records
|
|
Ramesh Babu 1,
Binu Ninan2 and
Venkata Sai3
From Departments of 1Pediatric Urology,
2Neonatology and 3Radiology, Sri Ramachandra
University,
Porur, Chennai, India.
Correspondence to:Dr Ramesh Babu, Professor of
Pediatric Urology, Sri Ramachandra University, Porur,
Chennai 600 106, India.
Email: [email protected]
Received: July 20, 2017;
Initial review: November 20, 2017;
Accepted: June 02, 2018.
Published online: June 02, 2018.
PII:S097475591600122
|
|
Aims: To audit the extent of evaluation of neonates with antenatal
hydronephrosis. Methods: Records of all neonates with antenatal
hydronephrosis between January 2013 and December 2016 were audited to
look for patient factors and investigation results. Results: 290
records were evaluated, 93 (32%) of which had abnormalities detected on
voiding cystourethrogram. In the presence of hydroureter, 65% had an
abnormality while in the absence only 11% were abnormal. In the presence
of pelvis ³20 mm, 93% had abnormal
diuretic renogram, while with pelvis <20 mm, only 1.5% were abnormal (P=0.001).
Numbers needed to harm calculation revealed 1 in 2 patients would
receive an unnecessary voiding cystourethrogram in the absence of
hydroureter, and unnecessary diuretic renogram when pelvis <20 mm.
Conclusions: While evaluating neonates with antenatal hydronephrosis
invasive tests can be limited, if evaluation is guided by
ultrasonographic criteria.
Keywords: Diagnosis, Radioisotope renography,
Vesico-ureteic reflux.
|
|
W
ith the advent of fetal ultrasound, antenatal
hydronephrosis is being diagnosed frequently. Studies [1-7] have shown
that fetal vesico-ureteric reflux (VUR) is too benign a condition to
warrant an invasive voiding cysto-urethrogram (VCUG). The revised
guidelines published by the Indian Society of Pediatric Nephrology
(ISPN) recommend a VCUG to be performed in all patients with unilateral
or bilateral hydronephrosis with renal pelvic antero-posterior diameter
(APD) >10 mm, hydronephrosis of Society for Fetal Urology (SFU) grade
3-4, or ureteric dilatation [8]. We audited the hospital records over a
four-year period of following ISPN recommendations, and assessed the
utility of invasive tests like VCUG in neonates with antenatal
hydronephrosis.
Methods
Records of all neonates who presented with antenatal
hydronephrosis between January 2013 and December 2016 were evaluated.
These neonates had been managed with a uniform protocol as per ISPN [8].
Records were audited to look for the patient gender, ultrasound factors
(unilateral/bilateral, presence/absence of hydroureter) and radiological
findings on VCUG (abnormal/normal). Treatment data were obtained from
records to identify significant abnormalities that warranted medical or
surgical treatment.
Those who were detected to have posterior urethral
valves (PUV) on early VCUG underwent cystoscopic fulgration after
stabilization. Those diagnosed to have VUR on late VCUG were started on
continuous antibiotic prophylaxis. In the remaining, a Diuretic
renography was performed at 6-8 weeks of life to assess renal function
and drainage; those with persistent obstructive pattern and reduction in
split renal function underwent surgical intervention.
APD from initial USG was correlated with diuretic
renography findings to determine mean APD in those with obstruction. APD
value, two standard deviation below the mean was used to determine how
many could have avoided diuretic renography. Based on the findings,
Numbers Needed to Harm (NNH) was calculated. Statistical analysis was
performed using Fisher’s exact test and P value less than 0.05
was considered significant.
Results
Among 310 neonates evaluated for antenatal
hydronephrosis over the 4 year period, after excluding those with
incomplete record, a total of 290 were evaluated (180 males; bilateral
130) (Fig. 1). The median (range) follow-up was for 2
(1-4) years. All the patients underwent VCUG; 93 (32%) had abnormalities
detected on VCUG. In boys with bilateral hydro-uretero-nephrosis, PUV
was demonstrated in 100%. In the presence of bilateral hydronephrosis
(without hydroureter) only 24% had an abnormal VCUG. In the presence of
unilateral hydronephrosis, only 5% had an abnormal VCUG and none
warranted an intervention. Presence of hydroureter was significantly
associated with an abnormal VCUG (65% vs11%, P=0.001) (Table
I).
 |
|
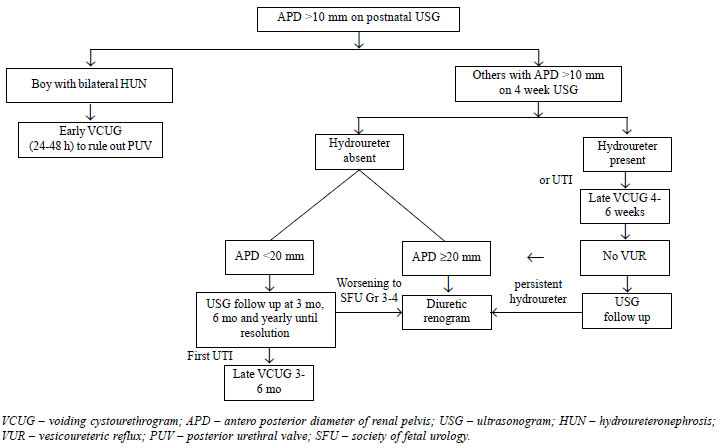
Fig. 1 Algorithm (based on the
present study) to limit invasive tests during post natal
evaluation of neonates with fetal hydronephrosis.
|
All patients with normal VCUG (n=197)
underwent Diuretic renography, and an obstructive pattern was identified
in 60 (20.5%). The mean (SD) APD in those with obstructive pattern was
significantly higher than in those without obstruction [26 (2.9) vs
14 (2.5) mm; P=0.001]. Obstructive pattern was significantly more
common in those with APD ³20
mm [93.5% vs 1.5%, P=0.001] (Table I). The
two patients with APD <20 mm remained stable without any need for
surgery, and 43 (74%) of those with APD
³20 mm had drop in
split renal function and underwent a pyeloplasty.
TABLE I Association of Postnatal Ultrasonographic Findings and Invasive Investigations in
Antenatally-detected Hydronephrosis
|
USG criteria |
Voiding Cystourethrogram (n=290) |
|
Abnormal |
Not Abnormal |
|
Hydroureter |
73 (65%) |
40 (35%) |
|
No hydroureter |
20 (11%) |
157 (89%) |
|
|
Renogram Findings (n=197) |
|
Obstructive pattern |
No obstruction seen |
|
APD ³20 mm |
58 (93.5) |
4 (6.5) |
|
APD <20 mm |
2 (1.5) |
133 (98.5) |
|
All values in No. (%); APD: Antero-posterior diameter of renal
pelvis; USG: Ultrasonography. |
One in two patients would be harmed by the
unnecessary voiding cystourethrogram in the absence of hydroureter and
unnecessary diuretic renogram when APD <20 mm. A total of 11/290 (3.8%)
encountered problems related to VCUG (hematuria 4, dysuria 4, urinary
retention 2, urosepsis 1) and 22/197 (11%) due to diuretic renography
(multiple venous access 12, sedation issues 7, repeat study 3).
Discussion
In this medical record review, we found that in the
absence of hydroureter a chance of finding a significant abnormality
(grade 3-5 VUR) in VCUG is 11%. Similary in those with APD <20 mm, the
chance of finding a significant obstruction in Diuretic renography is
only 0.5 %.
Mears, et al. [3] felt a more conservative
approach to the postnatal investigation of antenatal hydronephrosis did
not result in any missed damaged kidneys. Erickson, et al. [13]
reported that no cases of SFU III hydronephrosis have required surgery,
whereas, only 50% of children followed conservatively required surgery
in another report [14]. Lee, et al. [15] showed that by using
ultrasonography criteria 63% VCUGs could have been avoided. The SFU
guidelines have suggested an individualized approach, based on multiple
sonographic factors like laterality, ureteric dilatation, bladder wall
thickening and urethral dilatation [7].
On the basis of our findings we propose an algorithm
(Fig. 1) to limit the number of invasive investigations
like VCUG or Diuretic renography in those with ANH. We suggest that
those without hydroureter could be spared a VCUG unless they develop a
UTI. Similarly, those with <20 mm APD, Diuretic renography is reserved
for those with worsening hydronephrosis. One essential caveat in this
recommendation is the availability of an experienced pediatric
sonologist who can pick up a hydroureter or measure APD properly. This
protocol is based on a single center data. Further larger studies
covering multiple centers would be able to throw more light on the
extent of evaluation required in neonates with antenatal hydronephrosis.
Contributions: RB conceived the study analyzed
the results and prepared the manuscript: BN and VS helped in correcting
the manuscript
Funding: None; Competing interests: None
stated.
|
What This Study Adds?
•
Ultrasonographic criteria (absence
of hydroureter and APD <20 mm) could help in avoiding invasive
tests like voiding cystourethrogram and diuretic renogram.
|
References
1. Babu R, Sai V. Postnatal outcome of fetal
hydronephrosis: Implications for prenatal counseling. Indian J Urol.
2010; 26:60-2.
2. Ansari MS, Ayyildiz HS, Jayanthi VR. Is voiding
cystourethrogram necessary in all cases of antenatal hydronephrosis?
Indian J Urol. 2009;25:545-6.
3. Mears AL, Raza SA, Sinha AK, Misra D.
Micturatingcystourethrograms are not necessary for all cases of
antenatally diagnosed hydronephrosis. J Pediatr Urol. 2007;3:264-7.
4. Yeung CK, Godley ML, Dhillon HK, Gordon I, Duffy
PG, Ransley PG. The characteristics of primary vesico-ureteric reflux in
male and female infants with pre-natal hydronephrosis. Br J Urol.
1997;80:319-27.
5. Marra G, Barbieri G, Dell’Agnola CA, Caccamo ML,
Castellani MR, Assael BM. Congenital renal damage associated with
primary vesicouereteral reflux detected prenatally in male infants. J
Pediatr. 1994;124:726-30.
6. Pauchard JY, Chehade H, Kies CZ, Girardin E,
Cachat F, Gehri M. Avoidance of voiding cystourethrography in infants
younger than 3 months with Escherichia coli urinary tract infection and
normal renal ultrasound. Arch Dis Child. 2017; 102:804-8.
7. Nguyen HT, Herndon CD, Cooper C, Gatti J, Kirsch
A, Kokorowski P, et al. The Society for Fetal Urology Consensus
Statement on the Evaluation and Management of Antenatal Hydronephrosis.
J Pediatr Urol. 2010:6: 212-31.
8. Sinha A, Bagga A, Krishna A, Bajpai M, Srinivas M,
Uppal R, et al. Revised Guidelines on Management of Antenatal
Hydronephrosis. Indian Pediatr. 2013;50: 215-31.
9. Arora S, Yadav P, Kumar M, Singh SK, Sureka SK,
Mittal V, et al. Predictors for the need of surgery in
antenatally detected hydronephrosis due to UPJ obstruction - A
prospective multivariate analysis. J Pediatr Urol. 2015;11:248.e1-5.
10. Passerotti CC, Kalish LA, Chow J, Passerotti AM,
Recabal P, Cendron M, et al. The predictive value of the first
postnatal ultrasound in children with antenatalhydro-nephrosis. J
Pediatr Urol. 2011;7:128-36.
11. Onen A, Jayanthi VR, Koff SA. Long-term follow-up
of prenatally detected severe bilateral newborn hydronephrosis initially
managed nonoperatively. J Urol. 2002;168:1118-20.
12. Farhat W, McLorie G, Geary D, Capolicchio G,
Bägli D, Merguerian P, et al. The natural history of neonatal
vesicoureteral reflux associated with antenatal hydronephrosis. J Urol.
2000;164:1057-60.
13. Erickson BA, Maizels M, Shore RM, Pazona JF,
Hagerty JA, Yerkes EB, et al. Newborn Society of Fetal Urology
grade 3 hydronephrosis is equivalent to reserved percen-tage
differential function. J Pediatr Urol. 2007;3:382-6.
14. Chertin B, Pollack A, Koulikov D, Rabinowitz R,
Hain D, Hadas-Halpren I, et al. Conservative treatment of
ureteropelvic junction obstruction in children with antenatal diagnosis
of hydronephrosis: lessons learned after 16 years of follow-up. Eur
Urol. 2006;49:734e8.
15. Lee RS, Cendron M, Kinnamon DD, Nguyen HT.
Antenatal hydronephrosis as a predictor of postnatal outcome: A
meta-analysis. Pediatrics. 2006;118:586-93.
|
|
|
 |
|

