From the Department of Pediatrics, KEM Hospital,
Sardar Mudliar Road, Rastapeth, Pune 411 001, India.
Correspondence to: Dr. S.M. Shinde, Department of
Pediatrics, KEM Hospital, Sardar Mudliar Road, Rastapeth, Pune 411
001, India. E-mail:
shinde_sandeep@hotmail.com
Manuscript received: December 10, 2003; Initial
review completed: January 29, 2004; Revision accepted: June 1, 2004.
Abstract:
We report a 7½-year-boy with disseminated systemic
cryptococcosis. Although other species have been incriminated, this
appears to be the first report of Cryptococcus humicolus. The child
was HIV negative. He was treated with amphotericin B and fluconazole
with intensive supportive care. The child responded after 6 weeks and
is now on maintenance fluconazole therapy.
Keywords: Amphotericin B, Fluconazole, Crypto-coccus
humicolus, Systemic crypto-coccosis.
Systemic cryptococcosis is a rare infection in
pediatric patients(1). Most of the reports described are in adults
with immuno-deficiency disorders, or malignant condition on
chemotherapeutic agents(2). However, pediatric cases are equally
distributed(3). Of the various strains incriminated, Cryptococcus
neoformans serotype A appears to affect immunodeficient hosts such
as children with HIV or on steroid therapy, whereas Cryptococcus
neoformans var gattii affects normal immunocompetent children(2), We
report for the first time, a systemic infection with cryptococcus
humicolus species affecting a young child.
Case Report
A 7½-year-boy was referred with history of low
grade fever, cough and weight loss for a duration of 2 months. He
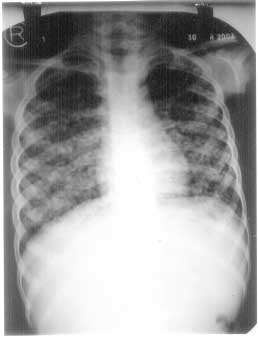
was dyspneic for one week. Chest X-ray prior to the admission was
suggestive of bilateral miliary shadows (Fig.1). Erythrocytic
sedimentation rate was normal and tuberculin test was negative. The
pediatrician had started 4 drug antitubercular therapy (SHRZ) with
oral betamethasone. However, the condition had deteriorated even
after 2 months of antitubercular therapy. The patient had five
attacks of oral thrush during two years prior to admission. The
thrush responded each time to clotrimoxazole mouth paint and oral
fluconazole therapy. There was no history of contact with
tuberculosis. On admission the child was dyspneic with respiratory
rate of 70/min. The patient had tachycardia, generalized significant
lymph-adenopathy and bilateral pedal edema. There were rales and
rhonchi on auscultation of chest. Liver was enlarged 6.5 cm, firm,
and spleen was 3.5 cm below costal margin.
 |
|
Fig. 1. X-ray chest on admission
suggestive of bilateral miliary shadows. |
Blood culture grew Cryptococcus humicolus (by
using mini API and ID 32 strip biochemical reactions). Bone marrow
(Fig.2), liver biopsy and lymph node FNAC all showed Crytococcus on
histology. Urine culture also grew cryptococci. Serum
immunoglobulins were on lower side of normal limit (Table I). CD4
count was 22%, HIV by ELISA was negative. Tuberculin test (10 TU)
was negative. CT Brain was suggestive of atrophic changes with mild
hydrocephalus. We stopped antitubercular therapy and steroids and
started the patient on amphotericin B, fluconazole, cefotaxime and
amikacin (broad spectrum cover) and supportive therapy (oxygen 5
L/min and enteral nutrition with nasogastric tube feeding). Clinical
improvement in the form of reduced dyspnea, improved appetite and
regression of hepatosplenometaly was seen only after 3 weeks of
therapy. Fever subsided initially but relapsed with one episode of
neutropenia (absolute neutrophil count was 150/cmm, total leucocyte
count was 1500/cmm). It was treated with granulocyte monocyte colony
stimulating factor (GM-CSF) for 5 days. At the end of 6th week blood
culture and urine culture were sterile for Cryptococci. Child was
then taken off oxygen therapy. He received amphotericin B for a
total of 5 weeks. (total cumulative dose 700 mg). We were able to
discharge him after 7 weeks of hospitalization on fluconazole
prophylaxis. On 2 weeks follow up in out patient clinic, the patient
reported significant improvement and showed weight gain and
regression of hepatosplenomegaly.
Test
|
Result
|
Normal Range
|
S. IgM level
|
815 mg/dL
|
855 - 1255 mg/dL
|
S. IgM level
|
74 mg/dL
|
74-142 mg/dL
|
S. IgA level
|
92 mg/dL
|
96-206 mg/dL
|
S. IgE level
|
3.60 IU/mL
|
Upto 101 IU/mL
|
Absolute CD4
|
461 µL
|
289 - 2600 µL
|
Per cent CD4
|
22%
|
29 -59%
|
Absolute CD 8
|
508/µL
|
190 - 2120 / µL
|
Per cent CD8
|
24.2%
|
19 - 48%
|
 |
|
Fig. 2. Bone marrow biopsy stained with
leishman stain and seen under 100x oil immersion showing
cryptococci. |
Discussion
Cryptococcus grows in soil and in bird excreta
especially of pigeons(4,5). Infection is acquired in most cases by
inhalation of fungal spires(3). Cryptococcus neoformans has
worldwide distribution and preferentially infects immunosuppressed
hosts or patients with HIV infection(1). Prevalence data for India
are not available, but in sub Saharan Africa 15-80% of all patients
with AIDS develop cryptococcal infection(1). Most of the patients
reported are adults, over the age of 40 years(6). As mentioned
earlier it is rarely reported in children(5). However, none of the
above reports pertain to the species Cryptococcus humicolus.
In view of the miliary shadows on X-ray, dyspnea
and hepatosplenomegaly our patient was first thought to have
disseminated tuberculosis. Fungal culture was attempted because of
no response to antitubercular therapy. To our surprise both blood
and urine culture grew cryptococci. Liver biopsy, bone marrow biopsy
and lymph node biopsy also showed significant number of cryptococci.
The boy however, was negative for HIV on ELISA test.
The treatment generally recommended for systemic
cryptococcosis is amphotericin B with flucytosine(4,5,7,8). The
lipid based amphotericin B is mostly preferred as it is said to be
less nephrotoxic(7,8). However in view of financial constraints we
used the cheaper non lipid based amphotericin B with fluconazole (flucytosine
is not freely available in India)(9). We were worried initially, as
response to therapy was poor and child continued to need intensive
care support with oxygen and tube feeding for nearly 6 weeks. We
were able to discharge him home (after 7 weeks of hospitalization)
on fluconazole prophylaxis.
Prior to the use of amphotericin B cryptococcal
meningitis and disseminated disease were invariably fatal. However,
with the availability of amphotericin B, flucytosine, fluconazole
and other azoles, the mortality rate of cryptococcal disease has
decreased upto 28% with various regimen(3). However, the cost and
non availability of some of the drugs is a particular problem in our
country.
Acknowledgement
Authors would like to thank Dr. Avinash Pradhan
for interpreting the histology and Dr. Rama Manchanda for the
hematological work up of the case. Grateful acknowledge-ment is also
made to Dr. Sheila Bhave for her valuable help in drafting and
editing the report.
Contributors: SS drafted the report, carried out
literature search and was the resident incharge of the patient. KV
looked after the patient on day to day basis. AP decided the patient
management and will act as guarantor.
Funding: None.
Competing interests: None stated.
