|
|
|
Indian Pediatr 2015;52: 421-425 |
 |
Intermittent Short Course
Rifapentine-Isoniazid Combination for Preventing Tuberculosis in
Children
|
|
Source Citation: Villarino ME, Scott NA, Weis
SE, Weiner M, Conde MB, Jones B, et al.; for the International Maternal
Pediatric and Adolescents AIDS Clinical Trials Group (IMPAACT) and the
Tuberculosis Trials Consortium (TBTC). Treatment for preventing
tuberculosis in children and adolescents: A randomized clinical trial of
a 3-month, 12-dose regimen of a combination of rifapentine and isoniazid.
JAMA Pediatr. 2015;169:247-55.
Section Editor: Abhijeet Saha
|
|
Summary
In this randomized, open-label clinical trial
conducted at 29 sites across 5 countries, 1058 children (aged 2-17
years), who were eligible for treatment of latent tuberculosis
infection, were randomized to receive either 12 supervised once-weekly
doses of the combination drugs (rifapentine and isoniazid) for 3 months,
or 270 daily doses of isoniazid, without supervision by a health care
professional, for 9 months. Of the 471 in the combination-therapy group,
415 (88.1%) completed treatment vs 351 of 434 (80.9%) in the
isoniazid-only group (P =0.003). The 95% CI for the difference in
rates of discontinuation attributed to an adverse event was within the
equivalence range. Three of 539 participants (0.6%) who took the
combination drugs had grade 3 adverse events (AE) as against 1 of 493
(0.2%) who received isoniazid only. Neither arm had any hepatotoxicity,
grade 4 adverse events, or treatment-attributed death. None of the 471
in the combination-therapy group developed tuberculosis as against 3 of
434 (cumulative rate, 0.74%) in the isoniazid-only group.
Commentaries
Evidence-based Medicine Viewpoint
Relevance: There is ample literature documenting
the individual and public health benefits of chemo-prophylaxis for
asymptomatic children believed to be at high(er) risk of developing
tuberculosis (TB). This includes children living in contact with
confirmed tuberculosis cases and/or those with latent TB. The Revised
National Tuberculosis Control Program [1,2] and Indian Academy of
Pediatrics [3] recommend using isoniazid (10 mg/kg daily) for 6 months,
after ruling out active disease in these children. In contrast, the
Centers for Disease Control, USA (CDC) previously recommended [4] using
isoniazid for 9 months in contacts with latent TB (i.e., presence of
infection but not disease). Longer duration of prophylaxis is generally
associated with poorer adherence. In addition, isoniazid has the
potential to cause unpleasant adverse events including hepatotoxicity.
Therefore, alternate regimens with shorter drugs and/or durations are
sought for chemo-prophylaxis.
In 2011, the CDC concluded that directly observed
weekly administration of isoniazid with rifapentine (INH-RPT) for 12
weeks, has equivalent efficacy and safety compared to the traditional 9
months daily INH regimen. This was based on the results of a
well-designed, unblinded, multi-center, non-inferiority RCT in people
older than 12 years [5] which reported equivalence of weekly directly
observed INH-RPT combination for 12 weeks and daily unsupervised INH for
9 months (standard protocol). The two regimens had similar efficacy for
prevention of TB over nearly 3 years follow-up (cumulative rate 0.19%
for the combination vs 0.43% for monotherapy). However, adherence
to the regimen was significantly better with the combination (82% vs
69%). Although the group receiving combination regimen had a higher
discontinuation rate due to adverse effects (4.9% vs 3.7%),
hepatotoxicity was much lower (0.4% vs 2.7%). Therefore the CDC
recommended that the shorter INH-RPT regimen could be used to boost
adherence [6].
In contrast, the World Health Organization (WHO)
position appears to be more flexible and the 2015 guidelines permit any
of five different options viz daily INH for 6 or 9 mo, or weekly
INH-RPT for 12 weeks, or daily isoniazid-rifampicin combination
(INH-RMP) for 3-4 mo, or daily rifampicin for 3-4 months [7]. These
variations suggest that the issue needs greater exploration to identify
the optimal regimen.
Rifampicin and Rifapentine belong to the rifamycin
group of drugs that act against Mycobacteria by inhibiting bacterial
DNA-dependent RNA polymerase [8]. However, rifapentine has a
significantly longer elimination half-life than rifampicin (>12 h vs
2-3 h). Following oral ingestion, it achieves a plasma concentration
much higher than the desired minimum inhibitory concentration (MIC) and
serum levels remain higher than the MIC for over 72 hours [9].
Interestingly, consumption with food (especially lipid-rich meal)
increases the peak serum concentration, in contrast to rifampicin that
needs to be taken in a fasting state. Like other rifamycins, rifapentine
also has the potential to cause adverse events, including hepatotoxicity.
The establishment of rifapentine pharmacokinetics in children [10]
expanded the scope of using the drug in children as well.
Against this backdrop, the recent publication of
pediatric data [11] from the INH-RPT versus INH trial described above
[5] is a significant new addition to the existing knowledge on the
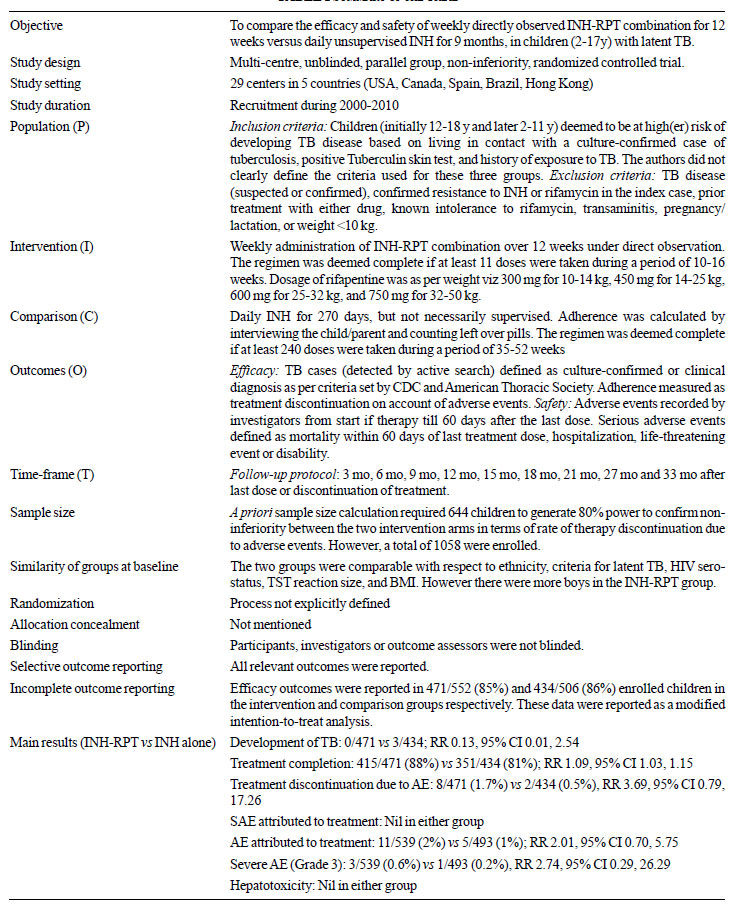
subject of chemoprophylaxis in children. A summary of the trial [11]
details is shown in Table I.
|
TABLE I Summary of the Trial
|
 |
Critical appraisal: Overall, the trial had
high risk of bias, based on unclear randomization process, inadequate
allocation concealment, absence of blinding, and failure to report data
as intention-to-treat. The investigators reported sample size
calculation based on efficacy outcome in the adult trial [5]. However
for this trial [11], they simply extrapolated these calculations. This
may account for recruitment of nearly twice the number of children
specified in the sample size calculation.
The trial was conducted over 13 years (10 years of
recruitment and nearly 3 years of follow-up). The investigators did not
report whether there were significant changes in TB prevalence rate,
control strategies and definition during this period.
It is interesting that despite supervised (directly
observed) weekly regimen, only 88% children completed INH-RPT therapy,
while 81% children completed 9 mo unsupervised therapy with INH. This
has two implications. First, almost 1 in 8 children failed to complete
treatment despite the best possible supervision/monitoring in a research
setting. This suggests that the treatment completion rate is likely to
be lower in the real world setting. Second, the difference from the
unsupervised group was only 7%. This is a very high completion rate in
the unsupervised group, given that only 69% in the adult trial [5]
completed this arm of therapy. This has programmatic implications also
since supervised/observed treatment is expected to result in better
treatment completion rates.
A 2013 Cochrane review [12], incorporating data from
the previous trial [5], reported equivalent success rate with either
regimen (RR 1.04, 95% CI 0.18, 1.07). However, INH-RPT combination
resulted in better adherence (RR 1.19, 95% CI 1.16, 1.22), less serious
adverse events (RR 0.55, 95% CI 0.40, 0.74) and lower hepatotoxocity
(RR 0.16, 95% CI 0.1, 0.27). However, the occurrence of adverse events
resulting in discontinuation of treatment was more frequent with the
combination (RR 1.32, 95% CI 1.07. 1.64). A more recent systematic
review incorporating a network meta-analysis [13] designed to identify
the most efficacious strategy for preventing TB reported equivalent
success (compared to the standard INH monotherapy) with 3 mo INH-RMP
combination, 3-4 mo rifampicin alone, and INH-RPT used in this trial
[11]. However it should be noted that many of the comparisons in a
network meta-analysis are indirect estimates rather than direct
(head-to-head) comparisons.
The cost-benefit ratio of higher expense for
monitoring versus lower expense for reduced number of doses of
medication (albeit more expensive per dose) needs to be calculated. The
authors [11] did not discuss the cost implications of increased
monitoring for adverse events that may be required for the INH-RPT
combination or the implications of switching therapy should such a need
arise. The current CDC guideline [6] correctly points out that choosing
between INH monotherapy versus INH-RPT combination ought to be
influenced of programmatic considerations related to direct observation,
availability of drugs, and resources to manage adverse events.
Extendibility: There are many similarities
between the children in the trial [11] and Indian children in the
general population. Over 90% were recruited because of close contact
with a confirmed case of TB, rather than other high-risk categories.
Although the cut-off for a positive tuberculin skin test was 5 mm,
majority of children had induration greater than 10 mm (which is the
cut-off used in India). The overall HIV prevalence was 2.3%; although
this is significantly higher than the population average in India, it is
reasonable in terms of TB prevalence. About 3.2% enrolled children were
in contact with cases resistant to isoniazid or rifampicin, which is
similar to the global average. However, the trial [11] did not include
infants below 2 y, and those with weight <10 kg; these two groups form
an important subgroup of children who receive chemoprophylaxis in India.
There are no therapy or prophylaxis trials with
rifapentine in India. An older systematic review [14] comparing
rifapentine (RPT) containing therapy (administered twice weekly) vs
rifampicin (RMP) containing combinations (administered daily)
identified 9 RCTs, and reported comparable treatment success (cure)
rate, relapse rate, adverse event rate, and hepatotoxic effects.
However, when rifapentine combinations were used once per week, it
resulted in higher relapse rate compared to twice of thrice weekly
rifampicin based regimens.
Nevertheless, it seems that the combination used in
this trial [11] could be explored for chemoprophylaxis in Indian
children also. However, it appears that rifapentine is yet not available
in India.
Conclusions: This RCT suggests that rifapentine-based
combinations hold promise for chemoprophylaxis in children at risk of
developing tuberculosis disease. However, the high risk of bias,
limitations with extendibility, and absence of cost-effectiveness
analysis spell the need for more research before recommendations for
routine practice can be confidently made.
References
1. Central TB Division, Directorate General of Health
Services, Ministry of Health and Family Welfare. TB INDIA 2014. Revised
National TB Control Programme. Annual Status Report. Available from:
http://www.tbcindia.nic.in/pdfs/TB%20INDIA%20 2014.pdf. Accessed
April 14, 2015.
2. No authors listed. National Guidelines on
Diagnosis and Treatment of Pediatric Tuberculosis. Available from:
http://tbcindia.nic.in/Paediatric%20guidelines_New.pdf. Accessed
April 14, 2015.
3. Kumar A, Gupta D, Nagaraja SB, Singh V, Sethi GR,
Prasad J. Indian Academy of Pediatrics. Updated national guidelines for
pediatric tuberculosis in India, 2012. Indian Pediatr. 2013;50:301-6.
4. Centers for Disease Control and Prevention.
Targeted tuberculin testing and treatment of latent tuberculosis
infection. MMWR. 2000;49:RR-6. Available from:
http://www.cdc.gov/mmwr/PDF/rr/rr4906.pdf. Accessed April 14, 2015.
5. Sterling TR, Villarino ME, Borisov AS, Shang N,
Gordin F, Bliven-Sizemore E, et al. Three months of rifapentine
and isoniazid for latent tuberculosis infection. N Engl J Med
2011;365:2155-66.
6. Centers for Disease Control and Prevention (CDC).
Recommendations for use of an isoniazid-rifapentine regimen with direct
observation to treat latent Mycobacterium tuberculosis infection. MMWR.
2011;60:1650-3.
7. World Health Organization. Guidelines on the
Management of Latent Tuberculosis Infection. World Health Organization
2015. Available from:
http://www.who.int/tb/publications/ltbi_document_page/en/ Accessed
April 14, 2015.
8. Munsiff SS, Kambili C, Ahuja SD. Rifapentine for
the treatment of pulmonary tuberculosis. Clin Infect Dis.
2006;43:1468-75.
9. Pascale Bemer-Melchiora P, Bryskierb, A, Drugeona
HB. Comparison of the in vitro activities of rifapentine and rifampicin
against Mycobacterium tuberculosis complex. Antimicrob Chemother.
2000;46:571-6.
10. Blake MJ, Abdel-Rahman SM, Jacobs RF, Lowery NK,
Sterling TR, Kearns GL. Pharmacokinetics of rifapentine in children.
Pediatr Infect Dis J. 2006;25:405-6.
11. Villarino ME, Scott NA, Weis SE, Weiner M, Conde
MB, Jones B, et al. Treatment for preventing tuberculosis in
children and adolescents: A randomized clinical trial of a 3-month,
12-dose regimen of a combination of rifapentine and isoniazid. JAMA
Pediatr. 2015;169:247-55.
12. Sharma SK, Sharma A, Kadhiravan T, Tharyan P.
Rifamycins (rifampicin, rifabutin and rifapentine) compared to isoniazid
for preventing tuberculosis in HIV-negative people at risk of active TB.
Cochrane Database Syst Rev. 2013;7:CD007545.
13. Stagg HR, Zenner D, Harris RJ, Muñoz L, Lipman
MC, Abubakar I. Treatment of latent tuberculosis infection: a network
meta-analysis. Ann Intern Med. 2014;161: 419-28.
14. Gao XF, Li J, Yang ZW, Li YP. Rifapentine vs.
rifampicin for the treatment of pulmonary tuberculosis: a systematic
review. Int J Tuberc Lung Dis. 2009;13:810-9.
Joseph L Mathew
Department of Pediatrics,
PGIMER, Chandigarh, India.
Email:
[email protected]
Infectious Disease Specialist’s Viewpoint
India is a high tuberculosis (TB) burden country only
because we tolerate TB. Modern medicine does not tolerate infectious
diseases – by healing and by preventing. Pediatrics promotes prevention
– through immunizations, good nutrition and stimulating cognitive
development. When it comes to TB, many are confused about prevention.
Mycobacterium tuberculosis (MTb) infection occurs
as micro-outbreaks in households of adults with pulmonary TB, and
sporadically for all others. BCG does not prevent infection, but
protects against meningitis and military TB in young infected children
[1]. But what about other outcomes of infection? For a few years MTb
would be in slow multiplication mode before becoming non-multiplying
‘latent TB infection’ (LTBI). The former is a window of opportunity when
MTb can be killed off with ‘preventive treatment.’
We identify infected children by Mantoux test with
Purified protein derivative (PPD). By age 5, the cross-reactivity from
BCG would have markedly declined – so, that is a good age for routine
testing. If positive, infection was recent – the child has lived only 5
years. Isoniazid (INH) alone for 9 months, even 6 months, is the
standard preventive treatment. With rifampicin plus INH, the duration
can be reduced to 3-4 months [2]. Motivating parents to give drugs daily
to complete the course is not easy.
In USA in adolescents and adults rifapentine and INH
given once weekly for 12 week is as effective as the longer regimens.
This recent publication [3] shows this 12-dose regimen effective even in
children below the age of 12 years. As soon as rifapentine gets
registered in India, preventive treatment will become quite easy.
There is no excuse for not promoting preventive
treatment in high burden countries [4]. If we neglect pediatric MTb
infection, we will never be able to control adult TB [4].
References
1. Swaminathan S, Rekha B. Pediatric tuberculosis:
Global overview and challenges. Clin Infect Dis. 2010;50:S184-94.
2. Spyridis NP, Spyridis PG, Gelesme A, Sypsa V,
Valianatou M, Metsou F, et al. The effectiveness of a 9-month
regimen of isoniazid alone versus 3- and 4- month regimens of isoniazid
plus rifampin for treatment of latent tuberculosis infection in
children: results of an 11-year randomized study. Clin Infec Dis.
2007;45:715-22.
3. Villarino ME, Scott NA, Weis SE, Weiner M, Conde
MB, Jones B, et al. Treatment for preventing tuberculosis in
children and adloscents. A randomized clinical trial of a 3-month
12-dose regimen of a combination of rifapentine and isoniazid. JAMA
Pediatr. 2015;169:247-55.
4. John TJ. Tuberculosis control in India: Why are we
failing? Indian Pediatr. 2014;51:523-7.
T Jacob John
Child Health Foundation,
Gandhidham, Gujarat.
Email:
[email protected]
Pediatric Pulmonologist’s Viewpoint
The authors describe a non-inferiority randomized
controlled trial comparing two regimens for treatment of latent
tuberculosis infection (LTBI) in children. The results show that weekly
twelve dose observed regimen of isoniazid/rifapentine is non-inferior to
the standard regimen of unobserved nine months of isoniazid.
The isoniazid and rifapentine combination regimen has
benefits of early completion in 3 months and weekly observed doses which
led to better completion rates with equal efficacy (measured by the rate
of incidence of tuberculosis in follow up) compared to isoniazid alone.
The shorter combination regimen appears to have a similar safety profile
as the single drug INH regimen as the risk of hepatotoxicity was not
increased in the two drug regimen.
While the treatment of LTBI is an important strategy
for control of TB in the affluent low burden countries, the role of LTBI
is far more limited in high burden countries as the preventive therapy
does not have a lasting benefit and does not cover for any subsequent
infection. This limits the use of any preventive therapy only to the
young children (under 6 years) who are at a high risk of disseminated
disease after infection. At present, there are several issues with usage
of Rifapentine in children as there is non-availability of safety and
cost-effectiveness data in children less than 2 years and less than 10
kg. Since there are no pediatric formulations, therefore crushed tablets
mixed with food are given to children. This adds complexity as the
available reports have shown inconsistent bioavailability with such
usage. In general, the experts have reservation about using rifamycin-based
preventive therapy in our country because of the possible risk of
emergence of drug-resistance to this very potent but vulnerable drug.
Ankit Parakh
Department of Pediatrics,
BL Kapur Hospital, New Delhi
Email:
[email protected]
|
|
|
 |
|

