Anti-myelin oligodendrocyte glycoprotein (MOG) antibody disease has been
recently implicated as a major etiology for pediatric non-infectious
encephalitis [1]. We report a case of acute fulminant encephalitis in a
5 year old child mimicking viral encephalitis, which was eventually
diagnosed as anti-MOG antibody encephalitis leading to successful
treatment with immunotherapy, thus highlighting this condition as an
important differential diagnosis for acute viral encephalitis.
A 5-years-old previously normal Indian girl presented
with intermittent fever for 4 days, headache for 2 days followed by
encephalopathy. On admission, she was afebrile with normal vital signs
and a Glasgow coma scale of 12. Subsequently her GCS deteriorated to 8
within 12 hours necessitating mechanical ventilation, and she developed
signs of raised moderate intracranial hypertension and relative
bradycardia. Neuro-logical examination showed sluggish brainstem
reflexes including pupillary and occulocephalic reflex, brisk deep
tendon reflexes and bilateral extensor plantar response. There was no
history of seizures, abnormal movements, visual disturbances, bowel or
bladder dysfunction, or preceding altered sleep or behavior. There was
no history of contact with tuberculosis or recent travel. There was no
history of drug ingestion or any toxic exposure. The initial working
diagnosis was acute febrile encephalopathy with differential diagnosis
of viral encephalitis, acute demyelinating encephalomyelitis (ADEM) or
neuro-metabolic disease with acute decompen-sation. Emergent
neuroprotection measures and a combination of broad spectrum
antimicrobials including Acyclovir were instituted.
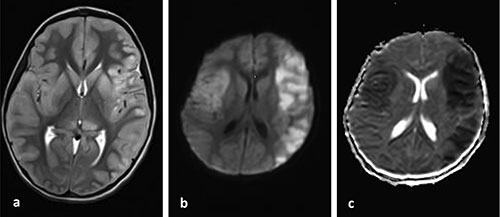
MRI brain showed extensive asymmetrical high signal
changes involving bilateral cortical regions along with ventromedial
thalamus with extensive diffusion restriction suggestive of cytotoxic
edema (Fig. 1). Post contrast study showed no evidence of
parenchymal or leptomeningeal enhancement. MRI of spine and MR angiogram
were normal. On day 2 of admission, patient developed focal seizures
with EEG showing bilateral periodic lateralizing epileptiform discharges
(PLEDs) highly suggestive of a neurotropic viral encephalitis. Due to
the patientís clinical condition, cere-brospinal fluid (CSF) was
deferred until the second week and was unremarkable including negative
routine studies, culture and PCR for neurotropic viruses. The patient
remained deeply encephalopathic and ventilator dependent for the next
two weeks with no response to treatment including acyclovir. In the
second week of admission she developed stereotypical flinging repetitive
asymmetrical lower limb movements, prompting a trial of methyl
prednisolone and immunoglobulins alongside autoimmune and lupus workup
including CSF and serum anti-NMDAR (N-methyl-d-aspartate receptor)
antibodies and oligoclonal bands which were negative. However, there was
no significant clinical improvement. This led to the counselling of the
family regarding an acute fulminant encephalitis with poor neurological
outcome and need for tracheostomy. After review of the recently
published case series by Armangue, et al. [1], serum anti-MOG antibodies
(IgG) immunofluorescence test was sent and showed a positive titer of
1:40. Plasma Exchange was then instituted with a total of 5 cycles on
alternate days. After the second cycle of plasma exchange itself, the
patient showed rapid clinical improvement in the form of improved GCS
and was successfully weaned off from ventilation. At the time of
discharge two weeks later, the patient could walk unsupported and talk
in simple sentences. On follow-up at 4 months after the illness, the
patient remained clinically well, and had regained pre-illness
developmental status. Her repeat anti-MOG titers were negative and
repeat neuroimaging showed no active lesions.
 |
|
Fig. 1 a) MRI T2-weighted image showing
bilateral asymmetrical (left more than right) cortical high
intensity signal with cortical swelling along with high signal
in the ventromedial thalami, b) MRI diffusion weighted image
(DWI) and c) apparent diffusion coefficient (ADC) images showing
bilateral cortical cytotoxic edema in the form of diffusion
restriction and corresponding drop in the ADC values.
|
During the last decade, anti-MOG antibodies have been
implicated in a wide range of pediatric acquired demyelinating syndromes
including optic neuritis, myelitis and ADEM [2]. However a recent
multicenter observational study by Armangue, et al highlighted the
widening spectrum of anti-MOG antibodies disease [1], demonstrating it
as the commonest etiology of non-infectious, non-ADEM encephalitis in
the pediatric age group, in addition to the well-established
presentations mentioned above. Of the 116 anti-MOG antibody positive
patients recruited in the study, 22 (19%) were diagnosed as encephalitis
other than ADEM, thus making it an important differential diagnosis in
pediatric encephalitis. The clinical presentation included
encephalopathy, seizures, status epilepticus, fever, abnormal behavior,
motor deficits, abnormal movements and brainstem-cerebellar dysfunction.
MRI showed non-ADEM like findings including extensive bilateral cortical
involvement (55%) with or without basal ganglia involvement and
meningeal enhancement. Another recent publication by Budhram, et al.
coined the term FLAMES based on a distinct radiological pattern of
unilateral cortical FLAIR-hyperintense lesions in adult anti-MOG
encephalitis with seizures [3]. Our case had clinical features of
encephalopathy, brainstem dysfunction and abnormal movements while MRI
brain showed extensive bilateral cortical and basal ganglia involvement
with diffusion restriction but without meningeal enhancement. These
observations were in keeping with the findings described in the study by
Armangue, et al. [1]
We conclude that anti-MOG encephalitis should be
considered in a child with fulminant encephalitis with bilateral
cortical involvement with diffusion restriction on MRI, with or without
meningeal contrast enhancement. Steroids should be the first line
treatment for anti-MOG encephalitis, and usually shows a good response.
However, early plasma exchange should be considered in cases with
inadequate response to pulse steroids.
1. Armangue T, Olive-Cirera G, Martinez-Hernandez E,
et al. Associations of paediatric demyelinating and encephalitic
syndromes with myelin oligodendrocyte glycoprotein antibodies: A
multicentre observational study. Lancet Neurol. 2020;19:234-46.
2. Fernandez-Carbonell C, Vargas-Lowy D, Musallam A,
et al. Clinical and MRI phenotype of children with MOG antibodies. Mult
Scler. 2016;22:174-84.
3. Budhram A, Mirian A, Le C, et al. Unilateral
cortical FLAIR-hyperintense lesions in Anti-MOG-associated Encephalitis
with Seizures (FLAMES): Characterization of a distinct clinico-radiographic
syndrome. J Neurol. 2019; 266:2481-87.

