I
nvasive Aspergillosis (IA) infection is a major
diagnostic concern in immunosuppressed children. For the diagnosis of
IA, simultaneous histopathologic/cytological and culture examination of
tissue and fluid specimens is recommended [1]. In sick children, biopsy
is not always possible and culture of respiratory specimens have a poor
yield. The double sandwich ELISA Galactomannan antigen test has been
developed and validated as useful for diagnosis of IA. The high
mortality associated with IA makes the galactomannan antigen test a
promising test for early initiation of therapy, especially in children
with acute leukemia [2].
TABLE I Diagnostic Efficacy of GMI in Invasive Aspergillosis in Pediatric Febrile Neotropenia
|
Cut-off |
Sensitivity |
Specificity |
PPV |
NPV
|
|
0.5 |
100% (11/11) |
47.7% (30/63) |
25% (11/44) |
100% (30/30) |
|
1 |
81.8% (9/11) |
66.7% (42/63) |
30% (9/30) |
95.5% (42/44) |
|
1.5 |
81.8% (9/11) |
92.1% (58/63) |
64.2% (5/14) |
96.7% (58/60) |
|
PPV and NPV: Positive and Negative Predictive Value; GMI:
Galactomannan Index. |
We studied the diagnostic accuracy of various
cut-offs of Galactomannan antigen test in children with febrile
neutropenia. Out of 74 episodes of febrile neutropenia, 17 children had
invasive aspergillosis by European Organization for Research and
Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the
National Institute of Allergy and Infectious Diseases Mycoses Study
Group (EORTC/MSG) 2008 criteria (3 Proven, 11 Probable and 3 Possible).
Galactomannan antigen test was done with immuno-enzymatic sandwich
microplate assay in serum samples (Platelia® Aspergillus, Bio-Rad
Laboratories, Hercules, CA). All 11 isolates had positive serum
Galactomannan antigen test expressed as "galactomannan index" (GMI
>0.5). All the probable infections that grew Aspergillus also had
evidence of fungal infection on computed tomogram of the chest.
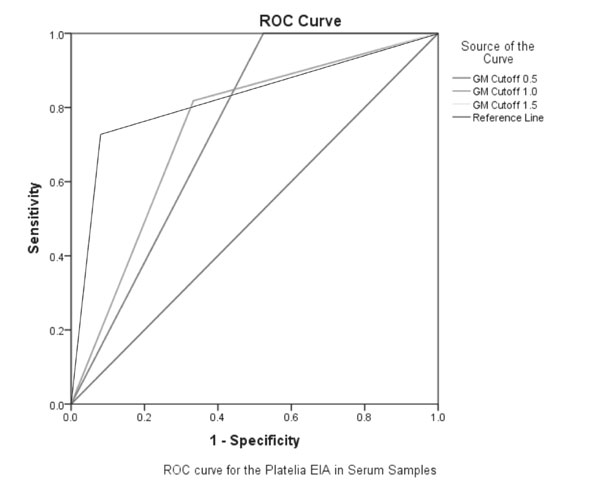
Table I shows various diagnostic accuracy parameters at
different cut-off points of GM antigen test. We plotted ROC curves for
various cut-off’s (Fig. 1) to identify optimal cut-off
value for GMI. GMI cut-off of 1.5 had the best diagnostic accuracy (Area
under curve 0.869).
 |
|
Fig. 1 ROC curve for various ODI
cut-offs of Galactomannan antigen test for diagnosis of Inasive
aspergillosis.
|
Different studies have used different positive
cut-off for GMI ranging from 0.5 to 1.5 [3]. Recent EORTC guidelines do
not recommend any specific cut-off value for positive result [4]. US
Food and Drug Administration approved ELISA in the United States
recommends a cut-off value of 0.5 [5].
There is heterogeneity in sensitivity and specificity
in various systematic reviews and meta-analysis done on galactomannan
assay. Our study showed no false negative at a cut-off of 0.5.
Increasing the cut-off to 1.0 or 1.5 increased the specificity but at
the expense of decrease in sensitivity (Table I). In our
study negative predictive value of GM antigen was 95-100%. Our study
shows that a GMI cut-off of 1.5 has a good specificity with reasonable
sensitivity and seems to be optimal cut-off in diagnosis of invasive
aspergillosis which is also consistent with other studies discussed in
literature [6].
Our study has certain limitations like the effect of
confounders giving false positive GM antigen test results like use of
antibiotics (e.g. piperacillin-tazobactam) and dietary
contamination (formulae milk) which were not excluded. For suspected
invasive pulmonary aspergillosis bronchoscopy with BAL is recommended
but it was not done in any patient due to presence of significant
thrombocytopenia. A small sample size was another major limitation.
Our study highlights the usefulness of serum GM
antigen test in the early diagnosis of IA and suggests a GMI cut-off of
1.5 as it have highest diagnostic accuracy. Early institution of
specific therapy will prevent unnecessary use of antifungal therapy and
development of resistance.
Contributors: JK: conceived idea,
collected data, prepared the manuscript; AS: Involved in data
collection, analysis and preparing the manuscript; RS: Involved in idea,
preparing the manuscript, evidence review and analysis; IX: preparing
manuscript and in galactomannan test reporting; SKK: Involved in idea,
preparing the manuscript, evidence review and analysis. All authors
approved the final version of manuscript.
Funding: None; Competing interest:
None stated.
References
1. Patterson TF, Thompson GR, Denning DW, Fishman JA,
Hadley S, Herbrecht R, et al. Practice Guidelines for the
Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious
Diseases Society of America. Clin Infect Dis. 2016;63:e1-60.
2. Lin SJ, Schranz J, Teutsch SM. Aspergillosis
case-fatality rate: systematic review of the literature. Clin Infect
Dis. 2001;32:358-66.
3. Arvanitis M, Mylonakis E. Diagnosis of invasive
aspergillosis: recent developments and ongoing challenges. Eur J Clin
Invest. 2015;45:646-52.
4. De Pauw B, Walsh TJ, Donnelly JP, Stevens DA,
Edwards JE, Calandra T, et al. Revised definitions of invasive
fungal disease from the European Organization for Research and Treatment
of Cancer/Invasive Fungal Infections Cooperative Group and the National
Institute of Allergy and Infectious Diseases Mycoses Study Group
(EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46: 1813-21.
5. Dixon C. Galactomannan - FDA. Available from:https://www.fda.gov/downloads/Drugs/GuidanceCompliance
RegulatoryInformation/Guidances/UCM420236.pdf. Accessed June 29,
2017.
6. Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive
aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect
Dis. 2006;42:1417-27.

