|
|
|
Indian Pediatr 2018;55: 251-253 |
 |
Isolated Mediastinal
Pseudocyst of the Pancreas
|
|
Pankaj Halder 1,
Kartik Chandra Mandal1,
Bidyut Debnath1
and Sumedha Mukherjee2
From Departments of 1Pediatric Surgery and
2Anesthesiology, Dr BC Roy, Post Graduate Institute of
Pediatric Sciences (PGIPS), Kolkata, West Bengal, India.
Correspondence to: Dr Pankaj Halder, Assistant
Professor, Dr BC Roy, Post Graduate Institute of Pediatric Sciences
(PGIPS), Kolkata, West Bengal, India.
Email: [email protected]
Received: January 02, 2017;
Initial review: May 17, 2017;
Accepted: November 22, 2017.
|
Background: Mediastinal pancreatic pseudocyst is a rare complication
of pancreatitis. Case characteristics: An 8-year-old boy with
chest pain and shortness of breath. Computed tomography of chest showed
a cystic mass in the mediastinum. The cyst aspirate revealed high
amylase and lipase levels, suggestive of pancreatic pseudocyst.
Outcome: The patient gradually recovered after Roux-en-Y
cystojejunostomy. Message: Cysto-jejunostomy is a viable
treatment option for mediastinal pancreatic pseudocyst, especially with
failure of medical therapy.
Keywords: Cystojejunostomy, Management, Transdiaphragmatic
approach.
|
|
Isolated mediastinal pancreatic pseudocyst (IMPP) is infrequently
reported in literature. It occurs when inflammatory exudative fluid
enters the mediastinum through the native diaphragmatic rents and
produces mediastinal pseudocyst of the pancreas (MPP) [1]. An atypical
clinical presentation makes the clinical diagnosis challenging.
Although, presumptive diagnosis and minimally invasive therapeutic
inter-ventions for MPP have now become possible with upgraded imaging
techniques, yet the specific surgical management remains a dilemma.
Case Report
An 8-year-old boy was admitted with unrelenting chest
pain and shortness of breath of 4 months’ duration. He was receiving
anti-tubercular therapy for the same from another center. After
admission, the child became severely dyspneic and developed circulatory
failure. Echocardio-graphy revealed pericardial effusion which needed
ultrasonography (USG) guided aspiration on two occasions. A detailed
history revealed absence of fever, vomiting, pain abdomen, hemoptysis,
hematemesis or abdominal trauma. Laboratory findings revealed anemia but
serum adenosine deaminase, amylase and lipase were not raised. Chest
X-ray showed mediastinal widening. USG revealed a thoraco-abdominal
cystic lesion with pancreatic calcification. USG-guided aspiration of
the cyst yielded pale sanguineous fluid which showed high amylase
(279,000 U/L) and lipase (206,500 U/L) but was negative for acid fast
bacillus. A possibility of pancreatic pseudocyst extending into the
mediastinum was entertained. Contrast enhanced computed tomography
revealed a tri-foliate shaped, large encysted lesion in the posterior
mediastinum while that of abdomen did not reveal any abnormality in
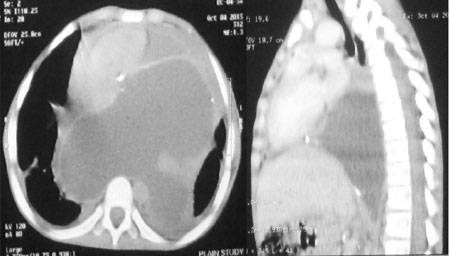
pancreas (Fig. 1).
 |
|
Fig. 1 Contrast-enhanced computed
tomograph of thorax shows large encysted mediastinum lesion with
tri-foliate shape, thick enhancing walls and lobulated outlines
in the posterior mediastinum. The heart is pushed anteriorly
with mild pericardial effusion.
|
After a few days, the child presented with chest pain
and dyspnea that could not be managed by medical therapy alone. Hence,
surgical drainage of the cyst was planned. Initially, abdomen was
explored with a transverse epigastric incision but, there was no
evidence of inflammation or collection around the pancreas. The same
incision was extended along left 7 th
intercostal space across the diaphragm. There was a thick walled large
isolated cyst in the posterior mediastinum which was aspirated. The cyst
was opened in between stay sutures and 1.5 litre of pale sanguineous
fluid was drained. A jejunal Roux loop was brought up to the mediastinum
through an opening in the diaphragm and anastomosed to the interior wall
of the cyst in the form of Roux-en-Y cystojejunostomy (RCYJ).
Oral feeding was initiated on 6th post-operative day.
The intra-operative cyst aspirate again showed extraordinary high
amylase and lipase levels. Biopsy of the excised cyst wall suggested a
benign cyst without any true lining epithelium. A repeat USG after three
weeks showed significant reduction in the size of the pseudocyst. At the
time of discharge, the child was asymptomatic.
Discussion
The most accepted hypothesis of MPP is extension of
abdominal pseudocyst into the mediastinum through any of the hiatal
openings or through the diaphragmatic crura. An ectopic pancreatic
tissue in the mediastinum may also produce it following abnormal
differentiation of pluripotent epithelial cells of the ventral primary
foregut or migration of the cells from pancreatic bud [2]. Isolated
variety possesses some peculiar features unlike the abdominal pseudocyst.
First, symptoms are non-specific (chest pain, shortness of breath,
fever, night sweats, heart murmur, fatigue, chronic pulmonary infiltrate
and tamponade) and mainly due to large mediastinal cystic mass. Thus, it
is often confused with thymoma, mediastinal teratoma, lymphoma and
cystic lung lesion like congenital cystic adenomatous malformation. In
our case, as the USG revealed thoraco-abdominal cystic lesion with
pancreatic calcification, a possibility of MPP was kept and USG guided
aspiration was performed to estimate the amylase/lipase. Second, the
serum amylase and lipase levels may not be raised in isolated variety.
Third, it does rarely resolve spontaneously. Fourth, complications like
interstitial lymphedema, pericardial effusion and cardiac tamponade are
common in long standing cases [3]. The role of definitive surgical
management of IMPP is still unclear.
Several management strategies like medical,
endoscopic procedure, surgical drainage and image guided external
drainage have been described in literature. Each of the options
needs to be selected carefully considering the location, number, size,
communication and status of the pancreatic duct. Complete resolution of
the cyst is reported with use of octreotide (somatostatin analogues) in
addition to bowel rest and parenteral nutrition [4]. Both transpapillary
nasopancreatic drainage and endoscopic USG guided internal drainage (via
transgastric or transesophageal) have been reported but, they are
associated with innumerable complications [5]. Endoscopic transpapillary
stent is only applicable when pseudocyst communicates with the
pancreatic duct [6]. External drainage procedure is not acceptable due
to increased chances of bleeding, infection, clogging of catheters,
recurrent cyst and risks for formation of a permanent fistula. Choice of
treatment is internal drainage procedure in the form cysto-esophagostomy
(CE) or cysto-gastrostomy (CG) or RCYJ. Both CE and CG are associated
with reflux and mediastinitis. Moreover, the length may not be adequate
to access the cyst cavity and excessive pulling may cause twisting of
the cardio-esophageal junction and tension at anastomotic site [7]. A
trans-diaphragmatic RYCJ has been evolved to ease a tensionless
anastomosis, especially for IMPP where a de-functioning jejunal loop is
anastomosed with the cyst at its dependant part. Thus, chances of
mediastinitis and reflux are minimal [8].
The management of IMPP is challenging as several
controversies exist regarding its specific treatment. Early diagnosis
can be made if this condition is kept in mind while treating any
longstanding case of mediastinal cystic mass. Trans-diaphragmatic RYCJ
seems to be a viable option for the treatment of IMPP.
Acknowledgement: Prof Biswanath Mukhopadhyay, Ex
Professor, Department of Pediatric Surgery, Nil Ratan Sircar Medical
College and Hospital, Kolkata.
Funding: None; Competing interests: None
stated.
References
1. Topa L, Laszlo F, Sahin P, Pozsar J. Endoscopic
transgastric drainage of a pancreatic pseudocyst with mediastinal and
cervical extensions. Gastrointest Endosc. 2006;64:460-3.
2. Rokach A, Izbicki G, Deeb M, Bogot N, Arish N,
Hadas-Halperen I, et al. Ectopic pancreatic pseudocyst and cyst
presenting as a cervical and mediastinal mass - case report and review
of the literature. Diagn Pathol. 2013;8:176-80.
3. Tan MH, Kirk G, Archibold P, Kennedy P, Regan MC.
Cardiac compromise due to a pancreatic mediastinal pseudocyst. Eur J
Gastroenterol Hepatol. 2002;14:1279-82.
4. Suga H, Tsuruta O, Okabe Y, Saitoh F, Noda T,
Yoshida H, et al. A case of mediastinal pancreatic pseudocyst
successfully treated with somatostatin analogue. Kurume Med J.
2005;52:161-4.
5. Sadat U, Jah A, Huguet E. Mediastinal extension of
a complicated pancreatic pseudocyst; a case report and literature
review. J Med Case Rep. 2007;1:12-5.
6. D bkowski K, Biaek A, Kukla M, Wójcik J,
Smereczyński A, Koaczyk K, et al. Mediastinal pancreatic
pseudocysts. Clin Endosc. 2017;50:76-80.
7. Kotsis L, Agocs L, Kostic S, Vadasz P.
Transdiaphragmatic cyst-jejunostomy with Roux-en-Y loop for an
exclusively mediastinal pancreatic pseudocyst. Scand J Thorac Cardiovasc
Surg. 1996;30:181-3.
8. Kamble RS, Gupta R, Gupta AR, Kothari PR, Dikshit
KV, Kekre GA, et al. Thoracoabdominal pseudocyst of pancreas: An
rare location, managed by retrocolic retrogastric Roux-en-Y
cystojejunostomy. World J Gastrointest Surg. 2015;7:82-5.
|
|
|
 |
|

