|
|
|
Indian Pediatr 2013;50: 334-335 |
 |
Nasal Hemophilic Pseudotumor: Favorable
Response to Radiotherapy
|
|
Radheshyam Purkait, Aritra Mukherjee, Suptotthitaa Naskar, and *Ramchandra
Bhadra,
From the Department of Paediatric Medicine and *Radiology , NRS
Medical College and Hospital, 138, AJC Bose Road, Kolkata, West Bengal,
India.
Correspondence to: Dr Radheshyam Purkait,
Department of Paediatric Medicine, NRS Medical College & Hospital,
Kolkata 700 014, West Bengal, India.
Email:
[email protected]
Received: July 07, 2012;
Initial review: August 01, 2012;
Accepted: September 21, 2012
|
|
Hemophilic pseudotumors are rare but
dangerous complications of Hemophilia. We hereby report a 3-year-old boy
with Hemophilia B, presenting with nasal pseudotumor, showing
favorable response to radiotherapy after unsuccessful treatment
with factor IX replacement therapy. The diagnosis and treatment of this
rare condition is also reviewed.
Key words: Hemophilia, Nasal, Pseudotumor,
Radiotherapy.
|
Hemophilia A and B are the only two
heritable bleeding disorders inherited as X-linked recessive
pattern affecting exclusively the male while females are
carriers. Hemophilia A (Factor VIII deficiency) is more
common than hemophilia B (Factor IX deficiency). The degree
of severity of clinical manifestations depends on factor
level. The joints are the most frequent site of bleeding
followed by the soft tissues and bones [1]. Occasionally, it
presents as a pseudotumor that most commonly develops in the
femur, tibia and pelvic bones, while orbit, small bones of
the hand, mandible, clavicle, spinal canal are less common
sites [2]. However occurrence of nasal hemophilic
pseudotumor is an extremely rare and there have been only
few such reports in world literature but none associated
with hemophilia B [3,4].
We report here a nasal pseudotumor in a
boy with Hemophilia B that presented as epistaxis with
progressively increasing respiratory distress to highlight
the relatively unusual location and radiotherapy as an
effective modality of treatment.
Case Report
A 3-year-old boy with hemophilia B was
admitted with a history of progressively increasing nasal
mass and intermittent epistaxis for last 1 month. Careful
history revealed that about 2 months back the child had a
minor trauma to the nose, followed by epistaxis, which was
initially controlled over 5 days with pressure bandage and
factor IX replacement. Physical examination revealed a large
swelling (5X6 cm) over anterior and upper part of the nose,
completely altering the normal architecture of the nose. The
swelling was tense, glistening, of heterogeneous consistency
and was only mildly tender to touch (Fig. 1).
Anterior rhinoscopy did not provide much information other
than documenting the presence of the mass.
 |
|
Fig.1 A large (5×6 cms),
tense, glistening swelling of heterogeneous
consistency over upper part of the nose with gross
narrowing of both the nostrils (left) and
post-treatment (right).
|
Laboratory investigations were as
follows: Hemoglobin: 10 gm%, prothrombin time (PT): 12.1s
(control-11.8s, INR-1.03), activated partial thrombo-plastin
time (aPTT): 100.9s (control- 28.1s), factor VIIIc assay:
76% (ref. range: 50-150%) and factor IX assay: less than 1 %
(ref. range: 50-150%).
Factor replenishment was started as an
initial treatment but the condition failed to improve much
and epistaxis continued, even after repeated transfusions.
Moreover the size progressively increased over the next few
days causing respiratory discomfort. A differential
diagnosis of nasopharyngeal angiofibroma was made.
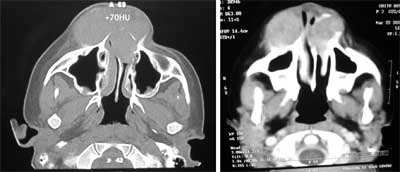
Non-contrast computed tomography (CT) scan of nose and
paranasal air sinuses demonstrated an externally protruding
large (3.5×5 cm) soft tissue mass with high density (+70HU)
involving the anterior third of both the nasal fossae with
erosion of the nasal septum and smooth scalloping of the
adjoining bones due to chronic pressure changes, which
showed mild enhancement on contrast study, suggestive of a
pseudotumor or blood cyst (Fig. 2). Surgical
intervention was planned but his parents refused that due to
operative risks.
 |
|
Fig.2 Showing an externally
protruding large (3.5×5 cms) soft tissue mass with
high density (+ 70 HU) on plain CT with erosion of
anterior nasal septum and smooth scalloping of the
adjoining bones. The lesion showed mild enhancement
on contrast study.
|
The child was therefore referred to the
department of Radiation Oncology and external beam radiation
therapy was then instituted. A total dose of 900 cGy over 6
fractions in 6 days was given by 6 MV linear accelerator.
The size of pseudotumor gradually decreased, and epistaxis
completely stopped by two weeks after completion of
radiotherapy. The patient has been under follow-up for last
six months since treatment. During this time no evidence of
tumor recurrence was observed.
Discussion
Pseudotumors or blood cysts are rare but
dangerous complications of hemophilia, occurring in 1%-2% of
patients with severe forms of the disease [1]. It is
essentially a chronic, slowly expanding hematoma resulting
from repetitive bleeding and is surrounded by thick fibrous
capsule. Many patients recall sustaining an injury prior to
development of the pseudotumor [5]. As the swelling
progresses, increasing pressure leads to the slow
destruction of adjacent structures by progressive necrosis
[6]. Invasive techniques such as, percutaneous aspiration
and needle biopsies are strongly discouraged to diagnose
hemophilic pseudotumor due to increased risk of
complications like hemorrhage, infection and fistulization
[2,6]. High quality CT scan and/or magnetic resonance
imaging (MRI) is an excellent tool for preoperative
visualization of the extent of the lesion, its mass effect
on vital surrounding structures and possible invasion of
joints. CT is particularly helpful in the evaluation of
bone, whereas MRI is superior to CT for delineating soft
tissue and intramedullary spaces [7].
Even though treatment of hemophilia has
undergone rapid development in the past decade, at present
hemophilic pseudotumor lacks standard management guidelines.
Till now, the initial treatment is conservative with
clotting factor replacement to keep an activity of 100%. For
patient with inhibitors, recombinant factor VIIa or
prothrombin complex concentrates can be used. In general,
operative removal of the entire mass is a reliable treatment
because the pseudotumor likely will reform if it is not
completely removed [1]. Radiotherapy with or without
replacement therapy has shown promising results as an
alternative to a more mutilating surgery or where surgery is
contraindicated, or resistant to conservative treatment. The
exact mechanism of hemophilic pseudotumor to respond to
radiotherapy is not known. But different opinion suggests
that radiation results in: (a) endarteritis in an
acute bleeding hematoma; (b) direct injury of small
vessels causing fibrosis and healing; and (c)
stimulation of fibroblasts resulting in fibrosis [8]. There
has been considerable variation in the literature in
radiotherapy dose. Also, the doses, as low as 600 cGy to as
high as 2350 cGy, with or without factor replacement, have
shown good response with complete resolution of lesions [9].
Even though, no standard radiation dose and fractionation
schedule exists in the management of hemophilic pseudotumors,
radiation therapy should be tried in cases where surgery is
not feasible.
Contributors: RP, AM and RB made the
diagnosis. AM and SN were involved in the management of the
child. All authors contributed to the literature search,
drafting and preparation of the manuscript. TS and RP were
involved in the management of the patients. RP will act as
guarantor.
Funding: None; Competing interest:
None stated.
References
1. Harold RR, Nigel SK, Miguel E.
Hemophilia A and Hemophilia B. In: Kenneth K,
Marshall AL, Ernest B, Thomas JK, Uri S, Josef TP,
editors. William Hematology. 8th ed. USA: McGraw Hills;
2010. p. 2009-21.
2. Kilic YA, Dundar SV, Onat D, Akhan O.
Iliopsoas hemophilic pseudotumor with bowel fistulization.
Bratisl Lek Listy. 2009;110:729-31.
3. Gupta S, Mohapatra BB, Ghai S, Seith
A, Kashyap R, Sharma R, et al. Haemophilic
pseudotumour of the paranasal sinuses: management with
radiotherapy and factor replacement therapy. Haemophilia.
2001;7:595-9.
4. Raj P, Wilde JT, Oliff J, Drake-Lee
AB. Nasal haemophilic pseudotumour. J Laryngol Otol.
1999;113:924-7.
5. Stafford JM, James TT, Allen AM, Dixon
LR. Hemophilic pseudotumor: radiologic-pathologic
correlation. Radio-graphics. 2003;23:852-6.
6. Karunanithi G, Sethi P, Reddy SK,
Vivekanandam. Hemophilia of orbit. Oman J Ophthal.
2009;2:86-8.
7. Geyskens W, Vanhoenacker FM, Van der
Zijden T, Peerlinck K. MR imaging of intra-osseous
hemophilic pseudotumor: case report and review of the
literature. JBR-BTR. 2004;87:289-93.
8. Kang JO, Cho YJ, Yoo MC, Hong SE.
Hemophilia pseudotumor of the ulna treated with low dose
radiation therapy: A case report. J Korean Med Sci.
2000;15:601-3.
9. Kapoor R, Shastri J, Malhotra P, Kumar V, Singh P.
Hemophilic pseudotumor- is there a role of radiotherapy?
Turk J Hematol. 2006;23:53-8.
|
|
|
 |
|

