|
|
|
Indian Pediatr 2013;50: 327-330 |
 |
Neurodevelopmental Evaluation of Very Low
Birth Weight Infants with Sepsis at 18 to 24 Months’ Corrected
Age
|
|
Dílek Díllí, Zeynep Eras, *UGur Dílmen and Evrim
Durgut Sakrucu
From the Department of Neurology and Developmental
Pediatrics, Zekai Tahir Burak Maternity Teaching Hospital, Ankara,
Turkey
Corresponding author:
Dilek Dilli, Zekai Tahir Burak Kadín Sagligi Egitimve
Arastirma Hastanesi, Neonatoloji Klinigi, Talatpasa bulvari, Hamamönü/Ankara/Turkey.
[email protected]
Received: April 03, 2012;
Initial review: April 23, 2012;
Accepted: June 28, 2012.
Published online: July 05, 2012.
PII: S097475991200303-2
|
In this cohort study, neurodevelopmental outcome of 20 of 24
surviving very low birth weight infants with sepsis followed-up
between 2008 and 2009 was compared with 20 control (uninfected
infants). We found that plasma interleukin-6 and C-reactive protein
values were negatively correlated with mental developmental index
scores (r= -0.33, P= 0.03 and r= -0.40, P= 0.01,
respectively) at 18 to 24 months’ corrected age. The results of this
study indicate that sepsis experienced in the neonatal period seems
to be related to low mental developmental index scores at 18 to 24
months’ corrected age.
Key words: Neurodevelopmental outcome, Preterm, Sepsis.
|
|
Despite recent advances in neonatal intensive care
improving survival of very low birth (VLBW) infants, survival without
major neonatal morbidity has not increased [1]. The risk factors for
poor neurologic outcome include prematurity, male gender,
bronchopulmonary dysplasia (BPD), intracranial hemorrhage (ICH) or
periventricular leukomalacia (PVL), and retinopathy of prematurity (ROP)
[2]. To the best of our
knowledge, to date three studies have demonstrated that neonatal
infections were associated with an increased risk of poor
neurodevelopmental outcomes [3-5].
Methods
In our previous study [6], performed between April
2008 and May 2009, 35 infants with sepsis [proven sepsis (culture
positive): 23, clinical sepsis: 12] were evaluated.
At the end of the first study, 7 of 35 (20.0%)
infants with clinical or proven sepsis died. Surviving and weighed
d"1500 g (n=20, 57.1%) infants were planned to be included for
the current study at 18 to 24 months’ corrected age. For each of the 20
VLBW sepsis survivors, 1 VLBW infant with the same gestational age, and
the same year of admission were recruited as matched controls.
The subjects were evaluated for the relation between
sepsis developed in the first weeks of life and neurodevelopmental
disabilities when the infants were 18 to 24 months’ corrected age Bayley
Scales of Infant Development-Second Edition (BSID-II) was administered
for neurodevelopmental evaluation [7]. Cerebral palsy (CP) was defined
as a nonprogressive central nervous system disorder. Neurodevelopmental
impairment (NDI) was defined as any of the following: moderate-to-severe
cerebral palsy; a mental develop-mental index (MDI) or psychomotor
developmental index (PDI) of less than 70; bilateral deafness; or
bilateral blindness. Profound impairment was defined as an MDI of less
than 50 or a Gross Motor Function Classi-fication System level of 4 or
5. Minimal impairment (MI) was defined as a MDI or PDI scores between
70-84 and not having moderate-to-severe cerebral palsy, bilateral severe
hearing loss or blindness [7].
Results
Perinatal data of the patients according to two
groups are seen on Table I.
TABLE I Perinatal Data and Neurodevelopmental Evaluation at 18-24 months
Corrected Age of study subjects according to Groups.
|
Group 1
(Sepsis)(n= 20) |
Group 2 (Without
sepsis)(n = 20) |
P value* |
|
Gestational age, median (IQR), wk
|
28.5
(28-32) |
29
(28-32) |
0.60 |
| Age
at study, median (IQR), d |
11.5
(9.2-16.7) |
13.5
(11-18) |
0.23 |
|
Birth weight, median (IQR), g
|
1150
(932-1295) |
1390
(1172-1470) |
0.007 |
| Male
gender, n (%) |
10
(50) |
10
(50.0) |
1.0 |
|
Premature rupture of membranes, n(%) |
6
(30) |
4
(20.0) |
0.71 |
|
Antenatal steroid, n (%)
|
10
(50) |
11
(55.1) |
1.0 |
|
Cesarean delivery, n (%)
|
16
(80) |
17
(85.0) |
1.0 |
|
5-min Apgar score, median (IQR)
|
7
(7-8) |
8
(7-9) |
0.10 |
| RDS,
n (%) |
12
(60) |
8
(40.0) |
0.34 |
| PDA,
n (%)
|
5
(25) |
2
(10.0) |
0.40 |
|
Mechanical ventilation, n (%)
|
16
(80) |
14
(70.0) |
0.71 |
|
IL-6, median (IQR), pg/mL |
185
(77-727) |
12
(2-62.7) |
0.001 |
| CRP,
median (IQR), mg/L
|
22
(10-34) |
2
(1-6.8) |
0.001 |
|
CD64MFI, median (IQR) |
98
(59-238) |
34
(32-76) |
0.001 |
| NEC,
n (%) |
1
(5.0) |
0 |
1.0 |
| BPD,
n (%)
|
4
(20) |
2
(10.0) |
0.66 |
| ICH,
n (%)
|
9
(45) |
0 |
0.001 |
| PVL,
n (%) |
2
(25) |
0 |
0.13 |
| ROP,
n (%) |
2
(10) |
1
(14.3) |
0.48 |
|
Length of hospital stay, median (IQR) |
44.5
(33.5-67) |
22
(17-38) |
0.001 |
|
Corrected age, median (IQR), mo |
19
(18-21) |
20
(18-21) |
0.62 |
| Body
weight, median (IQR), g |
10
(10-11.2) |
11(10-11.4) |
0.22 |
| Body
length, median (IQR), cm |
81(75.5-85) |
81
(81-84) |
0.54 |
| Head
circumference, median (IQR), d |
45
(41-49) |
46
(45-48) |
0.52 |
| MDI,
point, median (IQR),
|
70
(62-76) |
93
(71-100) |
0.001 |
| PDI,
point, median (IQR) |
86.5
(70.5-94) |
96
(85-110) |
0.001 |
|
Minimal impairment, n % |
8
(40.0) |
3
(15.0) |
0.15 |
|
Neurodevelopmental
Impairment, n % |
9 (45.0) |
4 (20.0) |
0.17 |
|
*P values of Mann Whitney-U or Fisher’s exact
test comparing infants with proven or clinical sepsis versus
without sepsis.
|
Correlation analyses showed that interleukin-6 (IL-6)
and C reactive protein (CRP) values at the first weeks of life and MDI
scores at 18 to 24 months’ corrected age were negatively
correlated (r=-0.33, P=0.03 and r=-0.40, P=0.01,
respectively). IL6 and CRP values did not correlate with PDI scores.
There was no correlation between neutrophil CD64 expression and MDI or
PDI scores.
Table I shows growth and neurodevelopmental
evaluation at 18 to 24 months’ corrected age and its relation to sepsis
at the first weeks of life. CP was defined in 2 (15.4%) infants with
proven sepsis. NDI occurred 8 (61.5%) infants with proven sepsis and 1
(14.3%) infant with clinical sepsis compared to 4 (20.0%) infants
without sepsis (P=0.02). MI occurred in 5 (71.4%) infants with
proven sepsis and 3 (23.1%) infants with clinical sepsis compared to 3
(15.0%) infants without sepsis (P=0.01). NEC (grade 3) was
defined in one patient with proven sepsis and PVL was detected in two
patients from each sepsis group. NDI was observed in these patients at
neurodevelopmental evaluation. Profound impairment was not defined in
any of the infants.
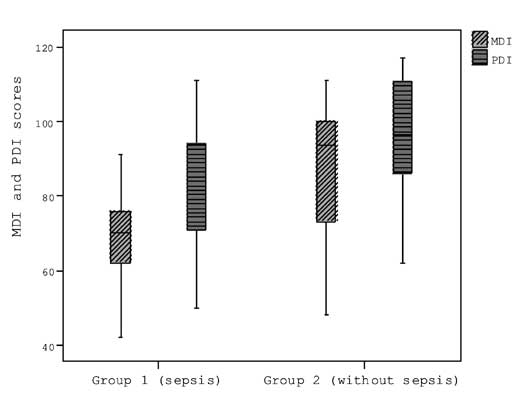
MDI and the PDI scores according to the groups are
shown in Fig. 1.
 |
|
Fig. 1 MDI and PDI scores according to
groups are shown; Group 1: proven or clinical sepsis, Group 2:
without sepsis.
|
Clinical characteristics of the subjects with and
without NDI are shown in Table II. It was noticed that
birthweight was significantly lower among the subjects with NDI. There
were no significant differences in other clinical variables including
sepsis between the two groups.
TABLE II Clinical Characteristics of the Subjects with and without Neurodevelopmental Impairment
|
Subjects with neuro- |
Subjects without neuro- |
P value* |
|
developmental impairment |
developmental impairment
|
|
|
(n=
13) |
(n=
27) |
|
|
Gestational age, median (IQR), wk
|
28
(26-32) |
29
(28-32) |
0.33 |
|
Birth weight, median (IQR), g
|
1160
(925-1290) |
1350
(1100-1470) |
0.02 |
| Male
gender, n (%) |
6
(46.2) |
14
(51.9) |
1.0 |
|
5-min Apgar score, median (IQR)
|
7
(7-8) |
8
(7-9) |
0.22 |
|
Respiratory distress score, n (%) |
8
(61.5) |
12
(44.4) |
0.50 |
|
Patent ductus arterious, n (%)
|
4
(30.8) |
3
(11.1) |
0.18 |
|
Mechanical ventilation, n (%)
|
1
(7.7) |
9
(33.3) |
0.12 |
|
IL-6, median (IQR), pg/mL |
165
(10-675) |
25.8
(12-110) |
0.17 |
| CRP,
median (IQR), mg/L
|
12
(2.3-31.5) |
6
(2-24) |
0.20 |
|
CD64MFI, median (IQR) |
88
(34-168) |
69.7-207) |
0.75 |
|
Sepsis (proven or clinical), n(%) |
9
(69.2) |
11
(40.7) |
0.17 |
|
Necrotising enterocolitis, n(%) |
1
(7.7) |
0 |
0.32 |
|
Bronchopulmonary dysplasia, n (%)
|
2
(15.4) |
4
(14.8) |
1.0 |
|
Intracranial bleed, n (%)
|
4
(30.8) |
5
(18.5) |
0.43 |
|
Periventricular leucomalacia, n(%) |
1
(16.7) |
1
(6.7) |
0.50 |
|
Retinopathy of prematurity, n (%) |
1
(7.7) |
1
(3.7) |
1.0 |
|
Length of hospital stay, median (IQR) |
47
(24-73) |
32
(22-42) |
0.24 |
| MDI,
point, median (IQR),
|
62
(45-63) |
87
(76-99) |
<0.001 |
| PDI,
point, median (IQR) |
65
(53-77) |
96
(87-110) |
<0.001 |
|
**P values of Mann Whitney-U or
Fisher’s exact test comparing infants with and without
neurovelopmental impairment.
|
Median MDI and PDI scores were significantly lower
among infants with NDI than those of infants without NDI.
Discussion
In this cohort study on VLBW infants, MDI and PDI
scores were lower in infants with sepsis compared to ones without sepsis
at 18 to 24 months’ corrected age. In a multicenter Swiss cohort study,
Schlapbach, et al. [5] performed neurodevelopmental evaluation on
541 extremely low birth weight infants. Their results indicated that
sepsis was among the four main risk factors influencing long-term
outcomes in their population, together with BPD, brain injury, and ROP,
all of which had a greater impact on outcome than gestational age, birth
weight, and gender. Benjamin, et al. [3] and Stoll, et al.’s
[4] studies have also supported the relationship between sepsis and poor
neurodevelopmental outcomes.
Several mechanisms may play role in
neurodevelopmental impairment associated with sepsis. First, bacterial
products and the cytokine storm in the course of the systemic
inflammatory response syndrome may directly damage the highly vulnerable
premature brain and other organs, such as the lung and retina [8,9].
Martin, et al. [10] also reported a higher risk of
neurodevelopmental dysfunction and microcephaly in NEC infants with late
bacteremia.
Recently, Silveira RC and Procianoy RS [11] studied
on 62 very preterm infants to evaluate association between severity of
early inflammatory response and neurodevelopment outcome. They did not
find any association of high cytokines plasma levels with poor
neurodevelopment outcome at 22 to 24 months’ corrected age. In the
current study, we found that inflammatory markers obtained at the first
weeks of life were negatively correlated with MDI but not PDI scores at
18 to 24 months’ corrected age.
The sample size is too small to make any meaningful
conclusions for a study of this nature. As this was a cohort study we
could include in the study only available patients 18 to 24 months’
corrected age. On the other hand, assessing neurodevelopment at two
years of age may underestimate the full spectrum of cognitive and
neuromotor outcomes, such as specific learning difficulties or milder
motor dysfunctions [12]. Additionally, a higher risk of poor
neurodevelopment has been reported in infants with NEC and with
meningitis [13]. Because there was only one case of grade 3 NEC among
infants with proven sepsis, we did not analyze its effect separately.
The results of this study indicate that sepsis
experienced in the neonatal period seems to be related to low MDI scores
at 18 to 24 months’ corrected age.
Conflict of interest: There is no conflict of
interest; Funding: None.
References
1. Fanaroff AA, Stoll BJ, Wright LL, Carlo WA,
Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and
mortality for very low birthweight infants. Am J Obstet Gynecol.
2007;196:147e141-148e141.
2. Schmidt B, Asztalos EV, Roberts RS, Robertson CM,
Sauve RS, Whitûeld MF. Impact of bronchopulmonary dysplasia, brain
injury, and severe retinopathy on the outcome of extremely
low-birth-weight infants at 18 months: results from the trial of
indomethacin prophylaxis in preterms. JAMA. 2003;289:1124-9.
3. Benjamin DK Jr, Stoll BJ, Fanaroff AA, McDonald
SA, Oh W, Higgins RD, et al. Neonatal candidiasis among extremely
low birth weight infants: risk factors, mortality rates, and
neurodevelopmental outcomes at 18 to 22 months. Pediatrics.
2006;117:84-92.
4. Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA,
Hintz SR, Vohr B, et al. Neurodevelopmental and growth
impairment among extremely low-birth-weight infants with neonatal
infection. JAMA. 2004; 292:2357–65.
5. Schlapbach LJ, Aebischer M, Adams M, Natalucci G, Bonhoeffer
J, Latzin P, et al. Impact of sepsis on neurodevelopmental
outcome in a Swiss National Cohort of extremely premature infants.
Pediatrics. 2011;128:e 348-57.
6. Dilli D, Oðuz ÞS, Dilmen U, Köker MY, Kýzýlgün M.
Predictive values of neutrophil CD64 expression compared with
interleukin-6 and C-reactive protein in early diagnosis of neonatal
sepsis. J Clin Lab Anal. 2010;24:363-70.
7. Bayley N. Bayley Scales of Infant Development II.
San Antonio, TX: Psychological Corp;1993.
8. Wu YW, Colford JM Jr. Chorioamnionitis as a risk
factor for cerebral palsy: a metaanalysis. JAMA. 2000;284: 1417-24.
9. Glass HC, Bonifacio SL, Chau V, Glidden D, Poskitt
K, Barkovich AJ, et al. Recurrent postnatal infections are
associated with progressive white matter injury in premature infants.
Pediatrics. 2008;122: 299-305.
10. Martin CR, Dammann O, Allred EN, Patel S, O’Shea
TM, Kuban KC, et al. Neurodevelopment of extremely preterm
infants who had necrotizing enterocolitis with or without late
bacteremia. J Pediatr. 2010;157:751-756.e1
11. Silveira RC, Procianoy RS. High plasma cytokine
levels, white matter injury and neurodevelopment of high risk preterm
infants: assessment at two years. Early Hum Dev. 2011;87:433-7.
12. Marlow N, Wolke D, Bracewell MA, Samara M.
Neurologic and developmental disability at six years of age after
extremely preterm birth. N Engl J Med. 2005;352: 9-19.
13. Hintz SR, Kendrick DE, Stoll BJ, Vohr BR,
Fanaroff AA, Donovan EF, et al. Neurodevelopmental and growth
outcomes of extremely low birth weight infants after necrotizing
enterocolitis. Pediatrics. 2005;115:696-703.
|
|
|
 |
|

