|
|
|
Indian Pediatr 2018;55:478-481 |
 |
Lupus Nephritis in
Indian Children: Flares and Refractory Illness
|
|
Jaiben George 1,
Kesavan P Sankaramangalam1,
Aditi Sinha1,
Pankaj Hari1,
Amit K Dinda2 and
Arvind Bagga1
From 1Division of Nephrology, Department
of Pediatrics and 2Department of Pathology; All India
Institute of Medical Sciences,
New Delhi, India.
Correspondence to: Dr Jaiben George, Department of
Pediatrics, All India Institute of Medical Sciences,
New Delhi 110 029, India.
Email: [email protected]
Received: March 25, 2017;
Initial review: June 19, 2017;
Accepted: March 18, 2018.
|
Objective: To evaluate the incidence of flares and treatment
resistance in children with lupus nephritis and their association with
renal outcomes. Methods: We retrospectively reviewed the case
records of 34 children treated for lupus nephritis (Class II-IV) at a
single center. Patients were followed for a minimum of five years to
evaluate treatment response, onset of flares, and renal survival.
Regression analyses were performed to identify the factors associated
with treatment refractoriness, incidence of flares and renal survival.
Results: The incidence of flares was 0.16 episodes/person/year.
Eight patients (23.5%) were refractory to treatment. The five-year renal
survival was 79%. Multiple episodes of flares (P=0.028) and
therapy refractoriness (P=0.003) were associated with poor renal
survival. Conclusions: Prevention and aggressive management of
renal flares is expected to prevent progression to end stage renal
disease in lupus nephritis.
Keywords: Glomerulonephritis, Prognosis, Systemic lupus
erythematosus, Treatment.
|
|
A
lthough lupus nephritis can occur at any age,
10-20% patients have onset in childhood with higher rates of renal
involvement reported in Asian population [1]. While better
immunosuppressive medications have resulted in improved renal survival
and quality of life, patients may experience relapses of disease and may
become refractory to treatment [2]. A previous report on lupus nephritis
from this center described the clinical features, treatment and outcomes
of 54 children with lupus nephritis with an average follow-up of 3 years
[3]. As information on disease relapses and management of refractory
illness is limited in children with lupus nephritis, this study aimed to
evaluate the incidence of flares and treatment resistance in these
patients, and their association with renal outcomes [4].
Methods
Medical records of 55 patients (age <18 years) of
Indian ethnicity treated in our nephrology clinic with a histological
diagnosis of lupus nephritis from Jan-2000 to Dec-2007 were reviewed
[5]. Patients were excluded if they had Class-I renal histology (n=1)
and did not have minimum 5-year follow-up (n=20), leaving behind
34 patients available for analysis.
Therapy for lupus nephritis was based on renal
histology, as described previously [3,5]. Response to treatment was
assessed at the end of 6-months’ induction therapy and classified as
complete response in patients who showed return of serum creatinine to
within ±25% of initial values, proteinuria <0.5 g/24 h, normal urine
sediment and serum albumin >3 g/dL while partial response was
persistence of proteinuria but ³50%
reduction in urine protein/creatinine ratio, and serum creatinine within
±25% of initial values [6]. Patients showing complete or partial
response were screened for renal flares. A nephritic flare was increase
in creatinine (>30%) associated with nephritic urinary sediment while
proteinuric flare was defined by increase in proteinuria (>1 g/m2/d)
without change in plasma creatinine [7]. Patients who did not show
partial or complete response during induction or following a flare were
considered refractory to treatment. These patients were treated with
cyclosporine/tacrolimus/rituximab. Adverse renal outcome was defined as
occurrence of one of the following: (i) estimated
glomerular filtration rate (eGFR) <30 mL/min/1.73 m2
for >3 months, (ii) requiring dialysis/renal transplantation, or
(iii) death due to renal failure [8,9].
The incidence rate of flares was calculated as the
number of flares per person-year. Univariate logistic regression was
used to evaluate risk factors for being refractory to treatment. Kaplan
Meier estimates and proportional hazards models were used to assess the
effect of flares and refractory illness on renal outcome.
Results
The median (IQR) follow-up period was 7 (5.8, 8.0)
years. Induction therapy resulted in complete response in 24 (70.6%) and
partial response in 8 (23.5%) patients. Of 32 responders, 14 (42.4%) had
at least one episode of renal flare; >1 flares were present in 10
(31.2%) (Table I). The median duration to onset of first
flare was 29 months. There were a total of 36 renal flares (36%
nephritic), with an incidence rate of 0.16 flares/person/year. Male
gender (P=0.002), presence of tubulointerstitial fibrosis (P=0.014)
and nephrotic syndrome at presentation (P<0.001) were associated
with higher incidence of flares, while hydroxychloroquine therapy (P=0.039)
was associated with reduced incidence of flares (Table II).
TABLE I Characteristics at Presentation with Lupus Nephritis in Patients with or without Renal Flares
|
Presenting Features |
No flare |
At least one flare |
|
(n=18)* |
(n=14) |
|
#Age at onset (yr) |
10.3 (8.2-12.7) |
10.2 (9-12) |
|
#Boys |
4 (26.7) |
5 (35.7) |
|
Body mass index, kg/m2 |
15.6 (14.8-18.3) |
15.1 (14.3-16.0) |
|
Skin rash |
13 (72.2) |
8 (57.1) |
|
Joint involvement |
12 (66.7) |
9 (64.3) |
|
Hematuria |
9 (50.0) |
8 (57.1) |
|
Edema |
8 (44.4) |
6 (42.9) |
|
Pulmonary involvement |
1 (5.6) |
1 (7.1) |
|
CNS involvement |
2 (11.1) |
1 (7.1) |
|
Hepatic involvement |
0 |
1 (7.1) |
|
Nephrotic syndrome |
4 (22.2) |
9 (64.3) |
|
#eGFR, mL/min/1.73 m2 |
82.1 (63-106.4) |
77.3 (48.3-91) |
|
#Complement C3, mg/dL |
56 (32-76) |
48.5 (25-70) |
|
#Anti-dsDNA antibodies, IU/mL |
130 (62-430) |
81.5 (50-250) |
|
Biopsy |
|
|
|
Class II |
2 (11.1) |
2 (14.3) |
|
Class III |
4 (22.2) |
3 (21.4) |
|
Class IV |
10 (55.6) |
8 (57.1) |
|
Class Vb |
1 (5.6) |
2 (14.3) |
|
Data reported as #median (IQR) or n (%); All
patients had complete data for all the variables except C3 (n=4)
and dsDNA (n=4);*Two children with initial non response are not
included; P>0.05 for all comparisons. |
TABLE II Incidence Rate of Flares in Relation to Patient Characteristics at Presentation
|
Features |
Incidence rate |
Incidence |
P value |
|
(per person/ |
rate ratio |
|
|
year) |
(95% CI) |
|
|
Sex |
|
|
|
|
Male (n=9) |
0.31 |
2.90 (1.42-5.91) |
0.002 |
|
Female (n=23) |
0.11 |
|
|
|
Age at onset |
|
|
|
|
³10 yr (n=19) |
0.14 |
0.76 (0.37-1.55) |
0.400 |
|
<10 yr (n=13) |
0.19 |
|
|
|
Hypertension at presentation |
|
|
|
|
Yes (n=12) |
0.19 |
1.51 (0.74-3.08) |
0.250 |
|
No (n=20) |
0.13 |
|
|
|
Nephrotic range proteinuria at onset |
|
|
|
|
Yes (n=13) |
0.26 |
3.87 (1.72-9.83) |
<0.001 |
|
No (n=19) |
0.07 |
|
|
|
First biopsy |
|
|
|
|
Class IV (n=18) |
0.20 |
1.89 (0.93-4.41) |
0.079 |
|
Other class (n=14) |
0.10 |
|
|
|
Tubulointerstitial fibrosis |
|
|
|
|
Present (n=15) |
0.22 |
2.48 (1.18-5.61) |
0.014 |
|
Absent (n=17) |
0.09 |
|
|
|
Therapy with hydroxychloroquine |
|
|
|
|
Yes (n=16) |
0.09 |
0.46 (0.19-1.02) |
0.039 |
|
No (n=16) |
0.20 |
|
|
|
Maintenance therapy* |
|
|
|
|
Mycophenolate- |
0.25 |
1.79 (0.79-3.84) |
0.123 |
|
mofetil (n=8) |
|
|
|
|
Azathioprine (n=20) |
0.14 |
|
|
|
Response |
|
|
|
|
Complete response (n=24) |
0.14 |
0.54 (0.25-1.21) |
0.098 |
|
Partial response (n=8) |
0.25 |
|
|
|
*Patients on steroids alone during maintenance therapy not
included. |
Eight (23.5%) patients (two at end of induction
phase, six after a flare) had refractory illness. The median time to
diagnosis of refractory illness was 3.9 years. The presence of
tubulointerstitial fibrosis was associated with increased risk of
refractory illness (OR=13.22 [1.39-124.91]; P=0.02). The presence
of Class IV nephritis, type of maintenance therapy- MMF/AZA and
proteinuria at onset failed to show significant association. Eight
patients (23.5%) developed an adverse renal outcome. Five-year patient
and renal survival were 93% and 79%, respectively. Refractory illness
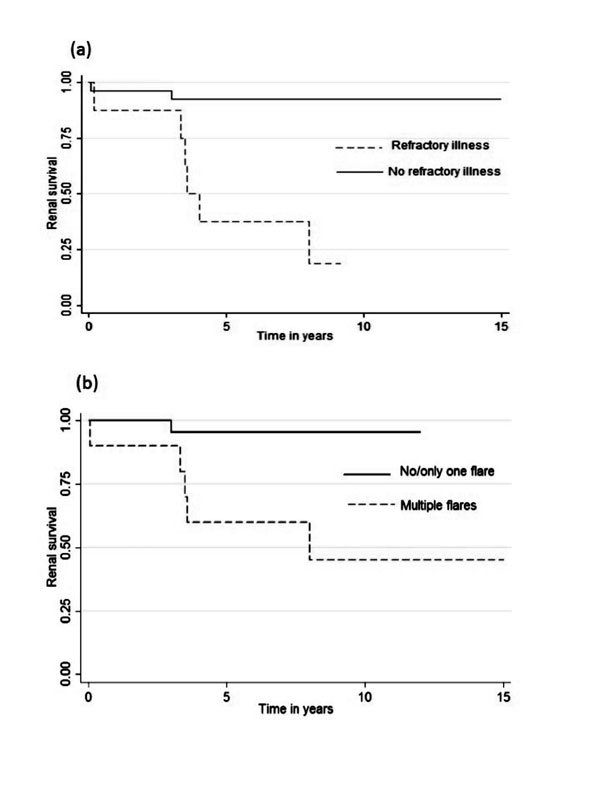
(hazard ratio, HR=11.52 [2.30-57.56], P=0.003) and occurrence of
multiple flares (HR=11.18 [1.29-96.97]; P=0.03) were associated
with adverse renal outcome (Fig. 1), while occurrence of
single renal flare was not.
 |
|
Fig. 1 Renal survival of patients
with lupus nephritis in relation to presence of (a) refractory
illness and (b) multiple flares.
|
Discussion
About two-fifths of the patients of lupus nephritis
in our series experienced at least one episode of renal flare and about
quarter of the patients were considered refractory to conventional
management. Patients with multiple flares and refractory illness were at
increased risk of adverse renal outcome.
This was a retrospective study and has all the
limitations of such design. Although we evaluated the associations
between various clinical characteristics and different outcomes, the
study could not account for potential confounding factors using
multivariate models due to the small sample size. As the study included
patients over a long period of time, variations in therapeutic practices
(hydroxychloroquine treatment becoming a standard practice) and
diagnostic criteria over time might have affected the results of the
study.
The incidence of renal flares reported in this study
is similar to studies in Caucasian children [9,10]. However, this is
lower than the 63% reported in a study by Srivastava, et al. [11]
in Indian children. But the incidence rate of 0.09 flares/patient/year
in their study was lower than that reported in the present study
suggesting that the incidence of multiple flares might have been less in
their cohort. Flares were associated with male gender, presence of
tubulointerstitial fibrosis and nephrotic range proteinuria which have
been linked to severe disease and/or adverse outcomes [12,13]. Other
pediatric studies report non-response rates of 10-29% that are
comparable to the 23% reported in the current study [4,13]. Our finding
that tubulointerstitial fibrosis relates to therapy refractoriness
suggests irreversible kidney injury might play an important role in
prognosis as reported in other studies [14]. Similar to our study,
Gibson, et al. [4] showed that non-response to standard treatment
predicted end-stage renal disease. Our findings that multiple renal
flares are associated with adverse outcome concur with those of Parikh,
et al. [15], who showed that poor renal outcomes are associated
with the number of flares per year and the time spent in flare.
The present study adds to the information on the
disease course and medium term outcomes in pediatric lupus nephritis,
and their determinants. Our findings underscore the role of multiple
disease relapses and subsequent non-response to therapy in predisposing
to advanced kidney disease, and emphasize the importance of vigilance
for disease relapses and the role of effective immunosuppressive
strategies in maintaining disease remission.
Contributors: All authors have contributed to
study concept and design, drafting of manuscript, and its critical
revision; JG, KPS, AS, AB: acquisition, analysis, or
interpretation of data; JG, KPS, AS: statistical analysis; AS, PH, AKD,
AB: Administrative, technical, or material support; AS, AB: study
supervision.
Funding: None; Competing Interest: None
stated.
|
What This Study Adds?
• The incidence of flares is about 0.16
episodes/person/year in children with lupus nephritis.
• About a quarter of these patients become
unresponsive to treatment at medium term follow-up.
|
References
1. Jakes RW, Bae S-C, Louthrenoo W, Mok C-C, Navarra
S V, Kwon N. Systematic review of the epidemiology of systemic lupus
erythematosus in the Asia-Pacific region: Prevalence, incidence,
clinical features, and mortality. Arthritis Care Res. 2012;64:159-68.
2. Vachvanichsanong P, McNeil E. Pediatric lupus
nephritis: More options, more chances? Lupus. 2013;22:545-53.
3. Hari P, Bagga A, Mahajan P, Dinda A. Outcome of
lupus nephritis in Indian children. Lupus. 2009;18:348-54.
4. Gibson KL, Gipson DS, Massengill SA, Dooley MA,
Primack WA, Ferris MA, et al. Predictors of relapse and end stage
kidney disease in proliferative lupus nephritis: focus on children,
adolescents, and young adults. Clin J Am Soc Nephrol. 2009;4:1962-7.
5. Churg J, Bernstein J, Glassock R. Renal Disease:
Classification and atlas of glomerular diseases. 2nd ed. New York,
Tokyo,: Igaky-Shoin; 1995.
6. Bertsias GK, Tektonidou M, Amoura Z, Aringer M,
Bajema I, Berden JHM, et al. Joint European League Against
Rheumatism and European Renal Association-European Dialysis and
Transplant Association (EULAR/ERA-EDTA) recommendations for the
management of adult and paediatric lupus nephritis. Ann Rheum Dis.
2012;71:1771-82.
7. Mok CC, Ying KY, Tang S, Leung CY, Lee KW, Ng WL,
et al. Predictors and outcome of renal flares after successful
cyclophosphamide treatment for diffuse proliferative lupus
glomerulonephritis. Arthritis Rheum. 2004;50: 2559-68.
8. Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel
F, Warady BA, et al. New Equations to Estimate GFR in Children
with CKD. J Am Soc Nephrol. 2009;20:629-37.
9. Gibson KL, Gipson DS, Massengill SA, Dooley MA,
Primack WA, Ferris MA, et al. Predictors of relapse and end stage
kidney disease in proliferative lupus nephritis: focus on children,
adolescents, and young adults. Clin J Am Soc Nephrol. 2009;4:1962-7.
10. Brunner HI, Gladman DD, Ibañez D, Urowitz MD,
Silverman ED. Difference in disease features between childhood-onset and
adult-onset systemic lupus erythematosus. Arthritis Rheum.
2008;58:556-62.
11. Srivastava P, Abujam B, Misra R, Lawrence A,
Agarwal V, Aggarwal A. Outcome of lupus nephritis in childhood onset SLE
in North and Central India: Single-centre experience over 25 years.
Lupus. 2016;25:547-57.
12. Baqi N, Moazami S, Singh A, Ahmad H, Balachandra
S, Tejani A. Lupus nephritis in children: A longitudinal study of
prognostic factors and therapy. J Am Soc Nephrol. 1996;7:924-9.
13. Lee BS, Cho HY, Kim EJ, Kang HG, Ha IS, Cheong H
Il, et al. Clinical outcomes of childhood lupus nephritis: A
single center’s experience. Pediatr Nephrol. 2007;22:222-31.
14. Ioannidis JP, Boki KA, Katsorida ME, Drosos AA,
Skopouli FN, Boletis JN, et al. Remission, relapse, and
re-remission of proliferative lupus nephritis treated with
cyclophosphamide. Kidney Int. 2000;57:258-64.
15. Parikh SV, Nagaraja HN, Hebert L, Rovin BH. Renal
Flare as a Predictor of Incident and Progressive CKD in Patients with
Lupus Nephritis. Clin J Am Soc Nephrol. 2014;9: 279-84.
|
|
|
 |
|

