|
|
|
Indian Pediatr 2017;54: 477-480 |
 |
Screening for
Hypoglycemia in Exclusively Breastfed High-risk Neonates
|
|
Princy Singh, Amit Upadhyay, *Vishnubhatla Sreenivas,
Vijay Jaiswal and Pranjali Saxena
From Department of Pediatrics, LLRM Medical College,
Meerut, UP; and *Department of Biostatistics, AIIMS, New Delhi; India.
Correspondence to: Dr Amit Upadhyay, Department of
Pediatrics, LLRM Medical College, Meerut, India.
Email: [email protected]
Received: April 06, 2015;
Initial review: July 08, 2015;
Accepted: March 31, 2017.
|
Objective: To determine
incidence of hypoglycemia in exclusively breastfed, high-risk but
healthy newborns, and risk factors for its development. Methods:
This observational study enrolled 407 exclusively breastfed high-risk
(low birth weight newborns (1800-2499 g), late preterms,
small-for-gestation, large-for-gestation and infant of diabetic mother),
who did not require admission to neonatal intensive care unit and were
kept in postnatal wards with mother. Hypoglycemia was defined as blood
glucose £46
mg/dL (2.6 mmol/L). Blood glucose was monitored till 48 hours of life.
Results: 27% of the screened newborns developed hypoglycemia in
first 48 hours. 31 (7.6%) developed recurrent (>2) episodes, 28 (6.8%)
had moderate (<37mg/dL) while 8 (1.9%) developed symptomatic
hypoglycemia. With increase in birthweight, risk of hypoglycemia reduced
significantly (P=0.003). Hypoglycemia was observed more
frequently in first 2 hours as compared to next 48 hours (P=0.0001).
Low birth- weight, preterm gestation and male gender was significantly
associated with increased risk of hypoglycemia. Conclusion:
Healthy, high-risk exclusively breastfed newborns in postnatal wards
need close monitoring for hypoglycemia in first 24 hrs of life.
Keywords: Blood glucose, Feeding, Low
birthweight, Management.
|
|
C
aregivers are often apprehensive whether newborns
at risk for hypoglycemia, like small for gestational age (SGA), infants
of diabetic mothers (IDM), large for gestation (LGA) and late-preterm
infants, could be sustained on exclusive breastfeeding [1]. Hence they
often offer supplemental feeding, especially in first 48-72 hrs, leading
to low exclusive breastfeeding rates in the community [2-4]. These
high-risk newborns are recommended to be screened for hypoglycemia, as
it has been shown to be associated with poor neurological outcome [5].
Though incidence of hypoglycemia in high-risk neonates is well
documented, its occurrence in exclusively breastfed high-risk newborns
remains under-evaluated. Most studies on screening of hypoglycemia have
been done on non-exclusive breastfed high-risk newborns or only LGA or
SGA newborns, including those admitted in neonatal intensive care unit
(NICU) [6-9]. We planned this study to document incidence of symptomatic
and asymptomatic hypoglycemia in exclusively breastfed high-risk
newborns. We also intended to evaluate risk factors for development of
hypoglycemia in this population.
Methods
This prospective cohort study was conducted at LLRM
Medical College, Meerut, India between September 2011 to September 2012.
We included all high-risk healthy newborns in postnatal ward whose
mothers were willing for exclusive breastfeeding. High-risk group was
defined as low birth weight (LBW) infants (1800-2500 g), late preterm
(34-36 6/7weeks), SGA (birth
weight <10th percentile for
gestational age), infants of diabetic mother (IDM) or LGA (birthweight
>90th percentile for
gestational age). The birthweight percentiles were adopted from the
National Neonatal and Perinatal Database (NNPD) growth charts [10].
Infants requiring NICU admission within first 48 hrs of life or those
having major congenital malformations were excluded. The study was
approved by institutional ethical committee of LLRM Medical College,
Meerut, India. Informed written consent was obtained from parents. All
the details of the newborn and mother were noted in a proforma at the
time of enrolment.
Counseling as well as assistance for exclusive
breastfeeding was done in all cases by nurses and doctors of Gynecology
and Pediatrics department, as well as by distribution of pamphlets and
display of posters. Breastfeeding was ensured within 30 minutes of birth
in vaginal delivery and no later than 4 hrs of caesarean section, and
thereafter every 2 to 3 hrs, including at least two nighttime feeds
[11]. Blood glucose levels were monitored pre-prandial (preferred) at 1,
2, 6, 12, 24, and 48 hrs of life using glucometer strips (ACCU-CHEK
Active, Serial no. GN 22012409, Germany) [12]. Duration, frequency of
feeding, time since last feed, and if any feed apart from breast milk
was given, was documented. Confirmation of blood glucose by sending the
sample to the laboratory was done only if the level was less than 25 mg/dL
(1.1 mmol/L), if baby was symptomatic or if three consecutive readings
of BGL remained £46
mg/dL. Hypoglycemia was defined as BGL
£46 mg/dL (<2.6 mmol/L)
[13]. For this study, moderate hypoglycemia was defined as BGL of 25 to
<37 mg/dL (<2.1 mmol/L), while severe hypoglycemia as BGL <25 mg/dL
(<1.38 mmol/L). Recurrent hypoglycemia was defined as 2 or more episodes
of hypoglycemia in first 48 hrs of life.
Newborns developing asymptomatic hypoglycemia (25-46
mg/dL) were breastfed, and repeat blood glucose level was determined
after 1 hr; if still in range of 25-46 mg/dL, baby was breastfed again
and advised increased frequency of feeding, or increased volume if baby
was given expressed breast milk (EBM) [13]. Supplementation with infant
formula was done only if the level did not rise to >46 mg/dL despite
breastfeeding/EBM >2 times. Monitoring was discontinued if the blood
glucose level was >46 mg/dL on two consecutive measurements, and
newborns were at least 48 hrs of age. Baby was admitted to the NICU and
treated with intravenous dextrose as per standard protocols, if the
level was <25 mg/dL or symptomatic hypoglycemia occurred at any time
[14].
Data analyses were conducted using Stata 12.1 and
P-value <0.05 was considered significant. A generalized estimating
equations (GEE) model was used for comparison of blood sugar profile
over 48 hours. Using logistic regression, Odd’s ratio of incidence of
hypoglycemia associated with each variable was calculated. Using the
significantly associated variables with hypoglycemia, a multivariate
logistic regression was built to identify the independent factors.
Results
We enrolled 407 newborns, out of which 110 (27%)
developed at least one episode of hypoglycemia in the first 48 hrs of
life [95% CI 23-31%]. Table I and Fig. 1
show incidence of hypoglycemia in different high risk groups and
subgroups. Out of 110 neonates, 74 (67.2%) developed one episode of
hypoglycemia, 36 (32.7%) newborns had recurrent episodes while 30
(27.2%), 5 (4.5%) and 1 (0.009%) newborn had two, three and four
episodes of hypoglycemia, respectively (Fig. 1). Applying
a cut-off of blood glucose level of 40 mg/dL and 45 mg/dL, the incidence
of hypoglycemia was 10.5% and 22.6%, respectively. Majority of newborns
(92.7%) had asymptomatic hypoglycemia. Moderate hypoglycemia was
observed in 28 (25.4%) newborns, of which 24 (21.8%) had hypoglycemia in
first 6 hrs of life, but none of them had severe hypoglycemia. Among
eight symptomatic newborns, 3 (37.5%) neonates developed jitteriness, 2
(25%) developed feeding intolerance, 2 (25%) developed lethargy and 1
(12.5%) had irritability. These eight newborns required intravenous
fluids and were admitted to the NICU.
TABLE I Clinical Characteristics of High-risk Neonates in the Study (N=407)
|
Characteristic |
Number (%) |
Incidence (%)(95% CI) |
OR(95% CI) |
|
Male gender |
221 (54.3%) |
32.1 (26.0, 38.7) |
1.44 (1.12, 1.64) |
|
Low birthweight |
349 (85.7%) |
29.5 (24.8, 34.6) |
3.05 (1.34, 6.95) |
|
Preterm delivery |
130 (31.9%) |
36.9 (28.6, 45.8) |
2.03 (1.29, 3.20) |
|
Large for gestation age |
41 (10.1%) |
14.6 (5.6, 29.2) |
0.46 (0.19, 1.14) |
|
Small for gestation age |
89 (21.9%) |
32.6 (23.0, 43.3) |
1.30 (0.78 , 2.18) |
|
Cesarian delivery |
134 (32.9%) |
30.6 (22.9, 39.1) |
1.30 (0.82, 2.06) |
|
Primigravide mother |
151 (37.1%) |
28.5 (21.4, 36.4) |
1.12 (0.72, 1.76) |
|
Illiterate mother |
130 (32.1) |
30.8 (23.0, 39.5) |
1.33 (0.84, 2.11) |
|
Diabetes mellitus |
35 (9.6%) |
28.6 (14.6, 46.3) |
1.09 (0.50, 2.35) |
|
Premature rupture of membranes |
16 (4.0) |
18.8 (4.0, 45.6) |
0.61 (0.17, 2.19) |
|
Hypertension during pregnancy |
21 (5.2%) |
33.3 (14.6, 57.0) |
1.37 (0.54, 3.50) |
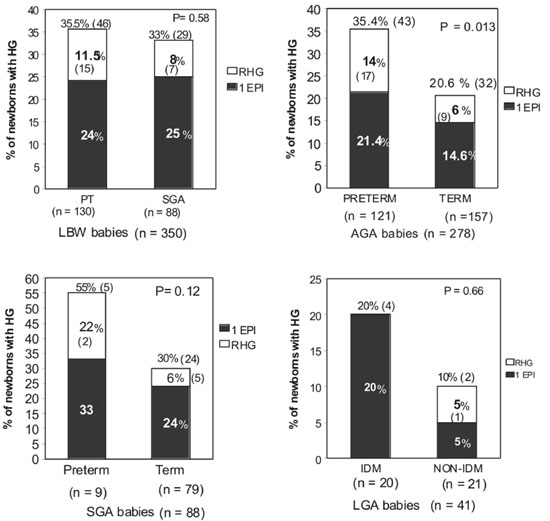
HG= Hypoglycemia, LBW= Low birthweight,
PT=Preterm, SGA=Small for gestation, LGA=Large for gestation,
IDM=Infant of diabetic mother, AGA=Appropriate for gestation,
RHG= Recurrent hypoglycemia, 1 EPI= Only 1 episode of
hypoglycemia.
|
|
Fig. 1 Incidence of hypoglycemia in different high
risk group categories.
|
Incidence of hypoglycemia gradually decreased with
time, from 44/407 (10.8%) at 1 hr to 1/298 (0.3%) at 48 hrs. Incidence
of hypoglycemia was significantly more in first 2 hrs as compared to
next 6 to 48 hrs (P=0.001). Mean (SD) blood glucose levels in
both term and preterm neonates showed a significant gradual increase
from 59.2 (15.9) mg/dL at 1 hr to 76.5 (14.5 mg/dL) at 48 hrs (P<0.01).
Out of 399 neonates, 17 (4.2%) received formula feeds
as 5 (29.4%) neonates had persistent hypoglycemia and 4 (23.5%) mothers
could not express enough breast milk. Despite euglycemia, 8 (40%)
newborns were given formula milk by their family as their mothers could
not successfully breastfeed despite counseling.
In first 6 hrs of life, preterm newborns had
significantly lower blood glucose than term newborns but this difference
was not significant beyond 6 hrs of life. Repeated measures regression
analysis showed that at any point till 48 hrs, preterm newborns had
about 4 mg/dL lower BGL than term newborns (95% CI; 1.48, 6.5 mg/dL;
P=0.002). Hypoglycemic episodes were significantly more in preterm
(36.9%) than term (22.4%) newborns (P=0.002). Odds of development
of hypoglycemia in preterm infants was 2.02 times (95% CI 1.3, 3.2) that
of term infants.
Hypoglycemic newborns were 170 g (95% CI 59, 280 g)
lighter than those newborns who did not develop hypoglycemia within
first 48 hrs of life (P=0.003). SGA and LGA newborns did not have
higher incidence of hypoglycemia as compared to high-risk AGA newborns.
Low birth weight (1.8 kg-2.5 kg), preterm gestation and male gender were
independently significantly associated with the risk of hypoglycemia in
exclusively breast fed newborns (by multivariate analysis) (Table
I). Pregnancy induced hypertension (PIH), premature rupture of
membranes (PROM), diabetes mellitus with gestational diabetes (DM/GDM),
mode of delivery, parity and educational status of mother were not found
to have any significant association with blood glucose levels and risk
of hypoglycemia (Table I).
Discussion
In this study, though incidence of hypoglycemia among
high-risk exclusively breastfed newborns was 27%, there was no severe
hypoglycemia, and very low incidence of symptomatic, moderate and
recurrent hypoglycemia. Preterm gestation, low birth weight and male
gender were significantly associated with hypoglycemia in this
population.
We did not confirm hypoglycemia in each asymptomatic
newborn by laboratory checks, as parents of asymptomatic, healthy,
breastfeeding newborns often object to blood-letting and may resort to
giving alternative milk for fear of more blood sampling. Also, we did
not have a control group of non-high risk breastfed neonates, for it
would have been unethical to screen them and give multiple pricks for
blood sampling.
There is wide variation in the incidence of
hypoglycemia reported in different groups of high-risk neonates [8,9,15]
as well as in method of glucose estimation, cut-off of blood glucose
level for defining hypoglycemia and population enrolled. Sasidharan,
et al. [7] found similar incidence of hypoglycemia in SGA and
preterm newborns in first 48 h of life [7], while others have reported
lower incidence, albeit in different conditions [7,8,16]. Holtrop, et
al. [8] had excluded newborns of diabetic mothers and their newborns
were not exclusively breastfed [8]. Mejri, et al. [16] had
included only term SGA infants, while Bhat, et al. [6] included
all SGA newborns, whether breastfed, formula-fed, or on intravenous
fluids. These factors could have lowered the incidence of hypoglycemia
in their studies. As compared to our study, Harris, et al. [9]
reported higher incidence of hypoglycemia in their population. Their
incidence of moderate and recurrent hypoglycemia was also higher than
that in our study [9].
Almost all our newborns with hypoglycemia were
asymptomatic as reported in some other studies as well [9,10]. Bhat,
et al. [6] have reported higher incidence of symptomatic
hypoglycemia in SGA newborns. The only study on exclusively breastfed
LBW neonates reported only 5% incidence of hypoglycemia using a
similar/different BGL cut-off [17]. However, as their study had smaller
sample size, included only LBW neonates and did not describe the
population characteristics in detail, results may not be comparable.
Current guidelines [18,19] of some forums recommend
formula milk or dextrose infusion in asymptomatic hypoglycemia only
after single unsuccessful trial of feeding over 1 hr. On the contrary,
our study point out that most of such high-risk babies can be managed by
supervised repeated exclusive breastfeeding or EBM rather than top
feeding. We conclude that healthy high-risk newborns in postnatal wards
can be exclusively breastfed, but there is need to closely monitor their
blood glucose levels at least in first 24 hrs, and asymptomatic
hypoglycemia in newborns can be managed with frequent breastfeeds. More
studies with long-term follow up are required to evaluate impact of this
asymptomatic hypoglycemia on this population.
Contributors: AU: conceptualized and designed the
study, monitored data collection and finalization of manuscript of the
paper. PS: enrolled the subjects, collected and managed the data, and
drafted the article; VS: analyzed and interpreted the data, reviewed the
paper and provided important intellectual content; VJ: monitored the
data collection and reviewed the draft paper. PS: reviewed the
literature, and contributed in enrollment of subjects and data
collection.
Funding: None; Competing interest: None
stated.
|
What This Study Adds?
•
Neonates at high risk for
hypoglycemia can be exclusively breastfed with close monitoring
for at least 24 hours and management of asymptomatic
hypoglycemia in these high-risk neonates is possible with
repeated and frequent breastfeeding.
|
References
1. Adamkin DH. Committee on Fetus and Newborn.
Postnatal glucose homeostasis in late-preterm and term infants.
Pediatrics. 2011;127:575-9.
2. Singhal P, Garg SK, Chopra H, Jain S, Bajpai SK,
Kumar A. Status of infant and young child feeding practices with special
emphasis on breast feeding in an urban area of Meerut. IOSR Journal of
Dental and Medical Sciences.2013;7:7-11.
3. Shaili V, Sharma P, Kandpal SD, Jayanti S,
Srivastava A, Nautiyal V. A community based study on breastfeeding
practices in a rural area of Uttarakhand. Natl J Community Med.
2012;3:283-7.
4. Oommen A, Vatsa M, Paul VK, Aggarwal R.
Breastfeeding practices of urban and rural mothers. Indian Pediatr.
2009;46:891-4.
5. Termote B, Verswijvel G, Gelin G, Palmers Y.
Neonatal hypoglycemic brain injury. JBR-BTR. 2008;91:116-7.
6. Bhat MA, Kumar P, Bhansali A, Majumdar S, Narang
A. Hypoglycaemia in small for gestational age neonates. Indian J Pediatr.
2000;67:423-7.
7. Sasidharan CK, Gokul E, Sabitha S. Incidence and
risk factors for neonatal hypoglycaemia in Kerala, India. Ceylon Med J.
2004;49:110-3.
8. Holtrop PC. The frequency of hypoglycaemia in
full-term large and small for gestational age newborns. Am J Perinatol.
1993;10:150-4.
9. Harris DL, Weston PJ, Harding JE. Incidence of
neonatal hypoglycaemia in babies neonates identified as at risk. J
Pediatr. 2012;161:787-91.
10. Report 2002-2003: National Neonatal Perinatal
Database Human Reproduction Research Centre Network. New Delhi: National
Neonatology Forum of India; 2006. (National Neonatal Perinatal Database
Human Reproduction Research Centre Network).
11. Government of India. National Guidelines on
Infant and Young Child Feeding. Ministry of Human Resource Development,
Department of Women and Child Development (Food and Nutrition Board)
2004;11. Available from: http://wcd.nic.in/fnb/fnb/guidelines/nationalguidelines.pdf.
Accessed April 1, 2017.
12. Chloherty JP, Lee-Parritz A. Diabetes mellitus.
In: Chloherty JP, Eichenwald EC, Hansen AR, Stark AR, editors.
Manual of Neonatal Care. 7th ed. Wolters Kluver, Lippincott Williams and
Wilkins; 2011.p-17.
13. UNICEF. Guidance on the Development of Policies
and Guidelines for the Prevention and Management of Hypoglycaemia of the
Newborn, 2011. Available from:https://353ld710iigr2n4po7k4kgvv-wpengine.
netdna-ssl.com/babyfriendly/wp-content/uploads/sites/2/2010/10/hypo_policy.pdf.
Accessed April 1,2017.
14. World Health Organization. Managing newborn
problems: a guide for doctors, nurses, and midwives (Integrated
management of pregnancy and childbirth) 2003. Available from
http://apps.who.int/iris/bitstream/10665/42753/1/9241546220.pdf.
Accessed April 1, 2017.
15. Lubchenco LO, Bard H. Incidence of hypoglycaemia
in newborn infants classified by birth weight and gestational age.
Pediatrics. 1971;47:831-8.
16. Mejri A, Dorval VG, Nuyt AM, Carceller A.
Hypoglycaemia in term newborns with a birth weight below the 10th
percentile. Paediatr Child Health. 2010;15:271-5.
17. Murty VY, Ram KD. Study of pattern of blood sugar
levels in low birth weight neonates who are exclusively on breast milk.
Journal of Dr. NTR University of Health Scinces. 2012;1:90-93.
18. Narayan S, Aggarwal R, Deorari AK, Paul VK.
Hypoglycaemia in the newborn. Indian J Pediatr. 2001;68:963-5.
19. Narayan S, Wazir S, Mishra S. Management of
Neonatal Hypoglycaemia. NNF Clinical Practice Guidelines 2011; 66-67.
Available from:
http://www.nnfi.org/images/pdf/nnf_cpg_consolidated_file-january102011.pdf.
Accessed April 1,2017.
|
|
|
 |
|

