There is high prevalence of vitamin D deficiency in adolescents,
especially females [1]. 25 hydroxyvitamin-D [25(OH)D] is the main
circulating metabolite of vitamin D, and its concentration in serum
reflects vitamin D stores. Serum concentrations of 1, 25(OH)
2D
increase by 50%–100% over pre-pregnancy levels during the second
trimester, and by 100% during third trimester, which is required for
fetal skeletal growth. In a population with a high prevalence of vitamin
D deficiency and poor dietary calcium intake, the problem is likely to
worsen during pregnancy and may cause significant consequences in the
newborn, including rickets and tetany [2,3]. This study was undertaken
to determine the prevalence of hypovitaminosis D in women in labor, and
in cord blood of their offspring.
This study was conducted from September 2013 to March
2014 in two branches of CloudNine Hospital in the city of Bengaluru,
Southern India. Pregnant women in labor were sequentially enrolled. They
were on regular maintenance dose of calcium (500 mg/day) and vitamin D
(400 IU/day). Women on any drugs that affect vitamin D levels or on
higher supplemental dose were excluded from the study. Those with a
known history of rheumatoid arthritis, disorders of thyroid, parathyroid
or adrenals, hepatic or renal failure, metabolic bone disease, type 1
diabetes mellitus, or malabsorption were excluded. Women with preterm
labor or antenatal suspicion of low birth weight babies were not
included in the study.
Maternal blood samples were collected during labor,
and cord blood samples were collected soon after delivery. The blood
samples were analyzed at Acquity Labs using Liquid Chromatography Mass
Spectrometry (LCMS/MS). The reference range of 25(OH)D for both maternal
and cord blood was taken as 20-80 ng/mL. A level of less than 20 ng/mL
was considered as hypovitaminosis-D.
 |
|
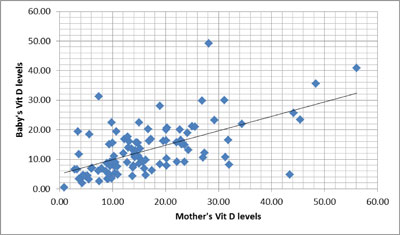
Fig. 1 Correlation of mothers
25-hydroxy vitamin D levels with cord blood vitamin D levels.
|
A total of 106 mothers and cord blood samples were
studied. The mean (SD) maternal vitamin D level was 16.3 (10.3) ng/mL.
Seventy-five mothers (70.7%) had hypovitaminosis-D. The mean (SD) cord
blood vitamin D level was 12.8 (8.5) ng/mL Eighty-eight newborns (83%)
had hypovitaminosis D. Among 75 mothers with hypovitaminosis D, 70
(93.3%) and blood samples had low vitamin D levels whereas 61.3% (n=18)
cord blood samples from 31 mothers having normal vitamin-D levels had
hyporitaminosis D. There was a significant (r=0.6; P<0.001)
correlation between maternal and cord blood vitamin D levels.
The limitation of our study was that we did not
quantify the sunlight exposure and did not record dietary calcium intake
or maternal nutritional status and skin color. Cord blood calcium and
PTH levels were also not done. Several reports confirm the high
prevalence of hypovitaminosis-D among pregnant women in South Asia
[4,5]. A strong correlation between maternal and cord blood levels has
also been reported earlier [6-8].
At present, vitamin D supplementation is not a part
of antenatal care programs in India. The US National Academy of Sciences
mentions 400 IU/day as the reference dietary intake during pregnancy but
several investigators worldwide are arguing for revised guidelines for
higher vitamin D allowance during pregnancy and lactation [9,10]. Our
study showed high prevalence of hypovitaminosis D in women in labor and
their newborns. This may call for vitamin D supplementation to mothers
or their newborns.
Contributors: PK: collection of data, analysis
and the initial manuscript was prepared; AS, KK, SVG, SS: reviewed
critically, helped in finalizing the manuscript and approved the final
manuscript.
Funding: None; Competing Interests: None
stated.
References
1. Rajeswari J,
Balasubramanian K, Bhatia V, Sharma VP, Agarwal AK. Aetiology and
clinical profile of osteomalacia in adolescent girls in northern
India. Natl Med J India. 2003;16:139-42.
2. Delvin EE, Salle BL, Glorieux FH, Adeleine P,
David LS. Vitamin D supplementation during pregnancy: Effect on
neonatal calcium homeostasis. J Pediatr. 1986;109:328-34.
3. Purvis RJ, Barrie WJ, MacKay GS, Wilkinson EM,
Cockburn F, Belton NR. Enamel hypoplasia of the teeth associated
with neonatal tetany: A manifestation of maternal vitamin D
deficiency. Lancet. 1973;2:811-4.
4. Goswami R, Gupta N, Goswami D, Marwaha RK,
Tandon N, Kochupillai N. Prevalence and significance of low
25hydroxyvitamin D concentrations in healthy subjects in Delhi. Am J
Clin Nutr. 2000;72:472-5.
5. Datta S, Alfaham M, Davies DP, Dunstan F,
Woodhead S, Evans J, et al. Vitamin D deficiency in pregnant
women from a non-European ethnic minority population: An
interventional study. Br J Obstet Gynaecol. 2002;109:905-8.
6. Nicolaidou P, Hatzistamatiou Z, Papadopoulou
A, Kaleyias J, Floropoulou E, Lagona E, et al. Low vitamin D
status in mother-newborn pairs in Greece. Calcif Tissue Int.
2006;78:337342.
7. Sachan A, Gupta R, Das V, Agarwal A, Awasthi
PK, Bhatia V. High prevalence of vitamin D deficiency among pregnant
women and their newborns in Northern India. Am J Clin Nutr.
2005;81:1060-64
8. Kazemi A, Sharifi F, Jafari N, Mousavinasab N.
High prevalence of vitamin D deficiency among pregnant women and
their newborns in an Iranian population. J Women’s Health.
2009;18:835-9.
9. Hollis BW, Wagner CL. Assessment of dietary
vitamin D requirements during pregnancy and lactation. Am J Clin
Nutr. 2004;79:717-26.
10. Dratva J, Merten S, Ackermann-Liebrich U. Vitamin D
supplementation in Swiss infants. Swiss Med Weekly. 2006;136:473-81.

