|
|
|
Indian Pediatr 2021;58:675-681 |
 |
Framework to
Incorporate Leadership Training in Competency-Based
Undergraduate Curriculum for the Indian Medical Graduate
|
|
Sumita Sethi, 1 Henal
Shah,2 Avinash Supe3
From Department of 1Ophthalmology, BPS GMC for Women, Khanpur,
Sonepat, Haryana; Department of 2Psychiatry,
Topiwala National Medical College and BYL Nair Charitable Hospital,
Mumbai, Maharashtra; and 3Department of Surgical Gastroenterology and
Medical Education, Seth GS Medical College and KEM Hospital, Mumbai,
Maharashtra.
Correspondence to: Dr Sumita Sethi, Coordinator Medical Education
Unit, BPS GMC for Women, Khanpur, Sonepat, Haryana.
Email:
sumitadrss@rediffmail.com
Received: December 16, 2020;
Initial review: December 27, 2020;
Accepted: February 06, 2021.
Published online: April 17, 2021;
PII: S097475591600314
|
The new competency-based curriculum recognized the
importance of leadership skills in physicians and has outlined
competencies that would lead to attaining this goal. To prepare the
Indian medical graduates as effective healthcare leader, there is no
universal approach; it is desirable that the institutes organize the
leadership competencies into an institutional framework and integrate
these vertically and horizontally in their curriculum in a longitudinal
manner. We describe the rationale for incorporating formal leadership
training in the new competency-based undergraduate curriculum and
propose a longitudinal curricular template utilizing a
mixed/multi-modality approach to teach and apply leadership
competencies.
Keywords: Competency-based medical education, Physician leader.
|
|
T he recently revised
Graduate Medical Education regulations (GMER) recognized
‘leader and member of the health care team and system’ as one of
the roles for the Indian medical graduate (IMG) [1]. With a
vision to develop an IMG who is globally relevant, this was a
desirable step. It was aligned to Accreditation Council for
Graduate Medical Education (ACGME), which requires students to
demonstrate the ability to ‘work effectively as a member or
leader of a healthcare team or other professional group’ [2]. While broad outlines are provided in the
curriculum, steps to implement the competencies and achieve
goals is largely the responsibility of each institute. We herein
describe the rationale for the inclusion of a formal, culturally
sensitive leadership training in undergraduate medical
education, and provide overarching principles of designing an
institutional framework for incorporating leadership training in
Indian medical colleges under the new competency-based
curriculum (CBME).
The Framework
Leadership Competencies
The first and foremost step is to identify
the desired leadership competencies and outcomes; these will
then serve as the basis for creating course objectives and
further guide the institutional framework and all subsequent
details like content and delivery of leadership training. Many
leadership competencies are already described in the new
curriculum [3]; however, these are not comprehensive and institutes may need to
reframe and expand them to precisely describe the leadership
competencies for their students. Ideally a complete set of
leadership competencies should include self-management
competencies (explo-ration and management of self to develop
greater self-awareness and emotional intelligence), team
management competencies (under-standing principles of working
colla-boratively and leading teams in multi-professional
environ-ments), ability to work with healthcare systems and
other focused leadership competencies (e.g., leading change,
setting realistic goals) and behavior or transfer of learning
based competencies (e.g., demonstration as successful team
leader in actual conditions, networking) [4-8].
Teaching Learning Methods
Once competencies have been identified and
defined; these will then guide the learning experiences that
will be used to deliver the leadership training. Methodologies
described for leadership training are vast, methods such as
group discussions and collaborative work, interactive lectures,
sharing narratives, presentations, demons-trations, use of media
clips and role play activities have been used previously [9-13].
Based on an extensive literature review of teaching learning
methods in leadership and teamwork training [5,6,9-14]
and from our experience of introduction of
institutional student leadership program [15], we propose the
following methodology for teaching learning of leadership and
teamwork principles:
Activities designed to enable an exploration
of self: ‘Who you are is how you lead’ [5,13]; it is
of foremost importance that a leader knows and understands
himself well so that he can identify areas for improvement [4].
The leadership journey for the student
will require an in-depth understanding of self so that one can
constantly learn from own experiences and deal with the
volatile, unpredictable, complex and ambiguous (VUCA) nature of
heathcare system [16]. We suggest tools such as SWOT analysis (for
self-exploration of one’s strength and weakness), changing
‘self-talk’ (for building self-image and improving
self-confidence, reflective writing (for developing deeper
knowledge of self) etc. in form of small group interactive
discussions to generate awareness of self and for developing
attributes like strong emotional intelligence and resilience.
Activities designed to understand leadership
and teamwork principles: Ability to work with others in a
team has been identified as an essential skill for a leader [7].
We suggest tools such as Myers Briggs type
inventory (MBTI); small group interactive activities aiming at
highly specific team related skills like Color blind, Mission to
Burundi; games based on group dynamics and stages of team
building; role plays based on difficult conversations, conflict
management, communication and negotiation skills to help them
learn about the underlying principles of team management, group
dyna-mics and common barriers to effective team working [17,18]. Use of appreciative leadership principles
of inquiry, illumination, inclusion and inspiration as a method
of positive strength-based leadership to create change would be
a useful model [19].
Experiential learning: Team-based
experiential learning activities have been accepted to be the
most effective for practicing leadership skills [7,14].
Students are asked to identify an issue or
concern in clinical, community or educational setting and
execute its solution through a standard framework that includes
defining the problem, communicating with team members and
stakeholders, preparing a timeline, deciding a solution to the
problem and implementation strategy. However, before designating
any assignment as team task, it is important to understand the
concept of ‘task interdependence’ i.e., the extent to which team
members depend on one another for task completion; if a task is
insufficiently complex and can be completed by an individual
working alone, then it should not be labelled as a team task
[20]. Some examples
of team based experiential learning tasks are student leadership
activities like leading a team for a seminar or a competition,
leading and participating in inter-professional teams in
hospitals or rural or mobile units, participating in audits and
utilizing clinical practice guidelines to plan comprehensive
effective patient care in multi-disciplinary settings.
Reflective practice: Reflecting on
an experience and subsequent analysis facilitate incorporation
of behavioral changes into practice, help in exploring its
relevance to past personal experiences and identifies
opportunities in future to achieve more desirable outcome
[17,18,21]. Equally
important is the concept of team reflexivity; there is evidence
that regular team reflexivity helps in improving organizational
outcomes in healthcare [22].
Clinical and community postings: Not
every opportunity for teaching of leadership skills needs to be
formal and explicit; there are certain very informal and readily
available opportunities in our medical curriculum which can be
well utilized. Clinical care rounds are the most commonly
identified curricular approach in literature towards teaching
leadership and teamwork by specifically demonstrating the roles,
responsibilities and interactions among members of
multidisciplinary teams in fulfilling needs of patients [23].
Similarly, much of leadership and teamwork content can also be
folded in the form of community healthcare responsibilities by
providing an opportunity to appreciate teamwork principles
associated with patient management and safety challenges in
community settings. Structured reflections could be obtained to
understand how the students benefitted from the clinical and
community postings.
Opportunity for networking and near peer
assisted teaching learning: Peer networking refers to a
network of like-minded individuals who can support, encourage
and offer opportunities to each other to learn and develop and
also to take on new leadership roles [24,25].
Networking with senior leaders provide a
wide range of contacts, offers an entirely diverse range of
perspectives, and can provide powerful supplementary teaching
mechanisms for leadership development [13,14].
We believe participants in leadership
training will learn best through multi modal learning strategies
involving active participation. Institutes need to identify
methodology for leadership training in alignment to the
respective learning objectives and availability of
institu-tional resources. Readers are referred to some other
publications for more detailed discussion of teaching learning
methodology for leadership [10,18].
Assessment Methods
The assessment plan should focus on
leadership competencies pre-identified and defined in the
insti-tutional framework. During the clinical/community
postings, students can be asked to reflect on any one incident
wherein team-based care had a positive effect on patient care
and another incident where dysfunctional team collaboration and
failure of effective communication amongst team members and
leader resulted in a major lapse in patient care. While the
students are learning to reflect on an experience, it is
important to make them understand to go beyond a mere
description of events; instead, they should analyze and gather
critical evidence of learnings from the event and how they will
apply these learnings for their development as a leader.
Students should be encouraged to undertake various change
initiatives in hospital and community settings; these can be
discussed in the student leadership cell, highlighting the key
areas of teamwork and deliberating on the leadership challenges
that were involved. These can be assessed by reflective writing
assignments and scored by a rubric, with a pre-decided score
designated for a particular level of competency. E-portfolio can
be used for the whole documentation process including various
reflective writing sessions, experiential learning activities
with critical analysis and comments for satis-factory
performance, record of student’s participation in other
leadership activities like student organizations and community
participation.
An important point to ensure is that students
are being assessed on ‘doing’ in addition to ‘learning’ of
leadership traits. During the implementation of leadership
program at our institute, the participants completed at least
one team based experiential learning assignments in hospital
and/or community settings with multisource feedback on the
assignments [15]. These were presented in the student leadership
cell and critically analyzed by a panel of faculty members;
those who performed exceptionally well were felicitated by
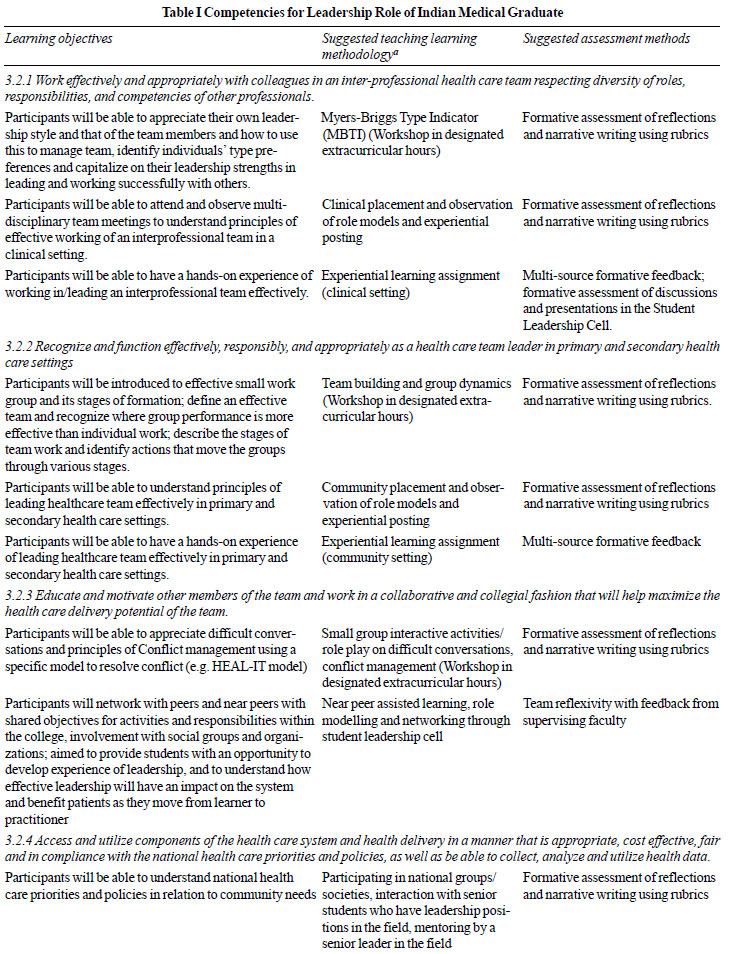
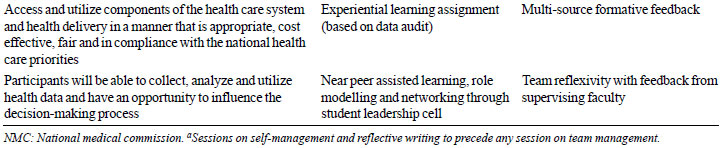
institutional student leadership awards. Table I
describes a few leadership competencies from the document [3]
and suggests the corresponding teaching learning and assessment
methods. These are just suggestions and it is up to the
institute to decide how to approach the particular competency.
If required, any of the validated leadership assessment
instruments readily available in literature may be utilized
[26], ensuring that it is aligned with the institutional
framework and the pre-decided leadership model.
 |
 |
Evaluation
We suggest a mixed method design including
both quantitative and qualitative methods of evaluation.
Qualitative methods of evaluation like focus group discussions,
structured interviews or interactive feedback sessions are
helpful in understanding of students’ perspectives and the
underlying factors, which makes the whole learning process
effective. In our leadership program, students shared their
leadership journey though reflections written at the end of each
session which were later qualitatively analyzed through content
analysis [15]. Questionnaire-based feedback usually target
participants’ perceptions (Kirkpatrick level-1) and thus may not
truly represent effectiveness of the program; targeting level-2
(learning of leadership skills) and 3 (transfer of learned
skills to real life situations) is desirable. This can be well
achieved through evaluation of the experiential learning
activities and ensuring long term follow up for concrete results
like changes in organizational practices.
The Timetable
Three block experiences can be created and
incorporated in the timetable vertically and horizontally in the
CBME viz., block-1 for introduction to basic teamwork and
leadership principles, block-2 for experiential learning through
clinical/community postings and electives and block-3 for
networking and mentoring.
Block-I: Introduction to key leadership and
teamwork principles: Extracurricular hours in phase-I and II
can be utilized for introducing participants to key
self-manage-ment and team management principles longitudinally
through methodology as described earlier. Timings and duration
of individual sessions can be decided by the institute; however,
group size should not exceed more than fifteen students to
ensure an effective interaction of all participants. Sessions of
self-management should precede those of team management,
following the basic principle that one needs to manage ‘self’
first and then ‘others’. Reflective practice needs to be
initiated early and practiced throughout; sufficient
opportunities for this are already available in the curriculum
e.g., small group teaching activities such as problem-based
learning sessions and tutorial/seminar presentations can be
explored as opportunities for leadership training from the first
year onwards. Anatomy dissection teams are their first
professional exposure to teamwork and a good opportunity to
illustrate basic principles of group dynamics. Discussions can
be initiated on how to define roles and responsibilities of
members, identify one’s own leadership style, establish team
goals, lay down strategies for improved team performance,
illustrate success and frustrations within the team etc.
Similarly, in second professional year, when the clinical
postings are initiated, a pharmacology session can be integrated
with clinical case discussion wherein the student learns the use
of available literature in pharmacology to plan an effective
multidisciplinary treatment plan for the patient.
Block-2: Experiential learning through
clinical and community postings and elective posting:
Further leadership training can be continued as an optional
4-weeks elective (block-1) through the leadership cell; since
students will also be continuing their clinical and community
postings, there will be lots of opportunities for reinforcement
and application of what has been learnt. Specific modules can be
developed in community health or chronic illness or in emergency
medicine with pre-defined learning objectives e.g., the chronic
diseases modules can be used to understand the importance of
working with other health professionals, while at the same time,
having a particular health care professional as patient’s care
coordinator. Small group discussions, student presentations and
reflections may be used and students can be given exercises
addressing leadership and teamwork directly related to the
modules. Above all, this is the most appropriate time for
students to ‘do’ what they have learnt, they should complete at
least two team based experiential learning assignments during
the elective posting; examples and assessment methods of team
based experiential learning assignments have already been
discussed.
Block-3: Networking and near peer assisted
learning: In third professional year part-2, students with
particular interests can attend activities held by the
leadership cell outside curricular hours and undertake
activities for bringing changes in organizational practices,
they also continue networking and mentoring the new
participants. Members of the club can meet once in a month or
fortnightly to discuss and deliberate on various teamwork and
leadership related issues.
The Rationale
Medical students have always been expected to
evolve as physician leaders and take on leadership roles from
the beginning of their professional career; it is ironical that
the traditional undergraduate medical curriculum did not address
leadership training formally. Recognition of ‘leader and member
of healthcare team’ as a role for the IMG in the new CBME
curriculum is a much-desired move towards ushering in formal
leadership training; however, there are a few questions that
need to be addressed before planning leadership training. The
first and foremost is ‘whether leadership can be taught’; if
yes, what leadership models will guide the whole process? What
will be the goals for the program and what will be the most
effective learning experiences to achieve them? When should the
training be initiated and how will the leadership competencies
be assessed? We have tried to address these questions while
proposing this longitudinally incorporated framework for
leadership training. Yes, leadership does consist of a series of
definable skills that can be well taught; while a few may have
inherent characteristics that make them better leaders, adequate
training and experiences could create successful leaders [7,27].
Different models and theories like
transformational leadership, authentic leadership, servant
leadership, self-leadership and appreciative leadership have
their own characteristics [7,26,28-30]; it is important to develop feasible models
for various branches of health-care, in different regions of the
country for respective institutions. Another important point to
consider is ‘when’ and ‘how’ to introduce this training; one
school of thought is that once negative perceptions develop as a
result of negative role modelling during clinical postings, it
becomes more difficult to change; other school of thought is
that such training will be effective only when sufficient
clinical experience has been gained [17]. There is no approach
which is specifically ‘right’ or ‘wrong’; it is essential that
the institute has a clarity for the specific aims of the program
and design the framework accordingly. Having an institutional
commitment is desirable; Janke, et al. [8] emphasized the
importance of weaving leadership development into the mission
and goals of the institute; including financial support, support
of administrators responsible for resource management,
in-organization recognition awards and appropriate faculty
development and reward systems [8].
Leadership training is not just meant to
prepare students for particular leadership roles; instead, it is
targeted to develop strong personal and professional values and
a range of non-technical skills such as communication skills,
strong emotional intelligence, negotiation skills, etc. which
will allow them to lead across professional boundaries and
influence many facets of life including healthcare [4].
Any one-time opportunity for development
of leadership will not be sufficient and the importance of
providing continuous opportunities for practicing leadership
skills, networking and mentoring cannot be over emphasized.
There are student bodies, student clubs, community and other
group activities in almost all medical schools; these
opportunities can be explored and utilized for formal leadership
training. Chaudry, et al. [31] proposed a medical leadership
society at medical schools as an easier to implement solution to
cater to the growing demand for leadership training for students
who demonstrate a special interest in leadership. We suggest the
introduction of student leadership cells with opportunities for
networking and peer mentoring to keep them engaged in leadership
activities in different stages of professional development.
Challenges and Limitations
Some institutes may already have one or the
other formal or informal leadership program in place; however,
if such training is being introduced for the first time in the
institute, many challenges would be expected. Hiring
professional managers or trainers might work as a one-time
solution to initiate the program but if it has to run as an
institutional program, it is important that faculty members are
sufficiently trained. There will be requirement of faculty
development activities targeting leader-ship skills to help the
faculty develop as trainers as well as role models. In the
initial phase of introduction of leadership training, not having
sufficient number of trained faculty in the institute will be a
major limitation. Under such circumstances, if training is made
compulsory for all students, it will tend to inherently dilute
the quality and the whole drive because there will simply be too
many students and too less trainers. On the other hand, if only
a few students are included, the whole concept of including
leadership as a core competency for students will not be
fulfilled. As an intermediate solution, we suggest utilizing
near peer mentoring through the institutional leadership cell
till the faculty development program on leadership is completed.
Furthermore, we will be mistaken by assuming that any one-time
course will make our students evolve as leaders; to achieve this
goal, longitudinal integration of leadership training in the
curriculum is to be ensured. This will require meticulous
planning and involvement of all the stakeholders i.e., members
of curriculum committee and medical education unit and other
faculty members. Another major challenge will be evaluation of
the program. As discussed earlier, only quantitative form of
evaluation will not be sufficient and more of qualitative
information targeting higher Kirkpatrick’s levels of learning
will be required; this will create severe time limitations.
Above all, long-term follow-up and evaluation will be needed to
provide concrete results in the form of change in organizational
practice as a result of leadership training.
CONCLUSION
The new competency-based curriculum not only
addresses a well-recognized gap in our medical undergraduate
training by recognizing the role of ‘leader’ for the IMG but
also provides scope for formal leadership training in the
already crowded undergraduate curriculum, through dedicated
extracurricular hours and electives. It is exciting to propose a
formal framework for explicit leadership training including team
training, community and clinical experiences, student leadership
opportunities, experiential learning, mentoring and networking.
The framework can be finalized by the institute itself according
to its own desired competencies, preferred teaching methods and
available resources. We believe that this framework could be
aligned with the current curriculum, without stretching either
the time or the resources. It is of foremost importance to have
institutional commitment and develop a supportive atmos-phere,
conducive for the students to evolve as leaders and for faculty
as role models through administrative and financial support,
appropriate allotment of resources, and training and incentives
for faculty.
Funding: None; Competing interest:
None stated.
REFERENCES
1. Medical Council of India. Regulations
on Graduate Medical Education 2019 - Addition as Part II of
the Regulations on Graduate Medical Education, 1997;
E-gazette. Accessed Dec 2, 2019. Available from:
mciindia.org/documents/Gazette/GME-06.11. 2019
2. The Accreditation Council for Graduate
Medical Education (ACGME). The outcome project 2014.
Accessed February 12, 2019. Available from:
www.acgme.org.
3. National Medical Commission:
Competency based Undergraduate curriculum for the Indian
Medical Graduate 2018. Accessed January 7, 2018. Available
from:
https://www.nmc.org.in/information-desk/for-colleges/ug-curriculum
4. Hargett CW, Doty JP, Hauck JN, et al.
Developing a model for effective leadership in healthcare: A
concept mapping approach. J Healthc Leadersh. 2017;9:69-78.
5. NHS Institute for Innovation and
Improvement and Academy of Medical Royal Colleges (NHS III).
Medical leadership competency framework: enhancing
engagement in medical leadership. 3rd edition. 2010 NHS
Institute for Innovation and Improvement and Academy of
Medical Royal Colleges.
6. Webb AM, Tsipis NE, McClellan TR, et
al. A first step toward understanding best practices in
leadership training in undergraduate medical education: A
systematic review. Acad Med. 2014; 89: 1563-70.
7. Varkey P, Peloquin J, Reed D, et al.
Leadership curriculum in undergraduate medical education: A
study of student and faculty perspectives. Med Teach.
2009;31:244-250.
8. Janke KK, Nelson MH, Bzowyckyj AS, et
al. Deliberate integration of student leadership development
in doctor of pharmacy programs. American J Phar Edu.
2016;80:2.
9. Shulman LS. Signature pedagogies in
the professions. Daedalus. 2005;134:52-9.
10. Jenkins DM. Exploring signature
pedagogies in undergraduate leadership education. Journal of
Leadership Education. 2012; 11:1-27.
11. Russell SS. An overview of
adult-learning processes. Urologic Nursing. 2006;26:349-52.
12. Sethi S. Leadership development
programs in undergraduate medical education: Understanding
the need, Best practices and Challenges. In:
Jespersen EA, editor. Exploring the opportunities and
challenges of medical students. NOVA Publishers; 2019.
p.32-57.
13. Till A, Mc Kimm J, Swanwick T. Twelve
tips for integrating leadership development into
undergraduate medical education. Med Teach. 2018;40:1214-20.
14. Warren OJ, Carnall R. Medical
leadership: Why it’s important, what is required, and how we
develop it. Postgrad Med J. 2011;87:27-32.
15. Sethi S, Chari S, Shah H, Aggarwal R,
Dabas R, Garg R. Implementation and evaluation of leadership
program for medical undergraduate students in India. In:
Abstract book of Annual conference of AMEE (Association for
Medical Education in Europe): The virtual conference; 2020
September 7-9.p.166.
16. Till A, Dutta N, McKimm J. Vertical
leadership in highly complex and unpredictable health
systems. British J Hosp Med. 2016;77: 471-5.
17. Banerjee A, Slagle JM, Mercaldo ND,
et al. A simulation-based curriculum to introduce key
teamwork principles to entering medical students. BMC
medical education. 2016;16:295.
18. Shah H, Ladhani Z, Morahan PS, et al.
Global leadership model for health professions education
Part 2: Teaching/learning methods. The J Leadership Educ.
2019;18:193-203.
19. Orr T, Cleveland-Innes M.
Appreciative leadership: Supporting education innovation.
International Review of Research in Open and Distributed
Learning. 2015;16:235-41.
20. West MA, Lyubovnikova J. Illusions of
team working in health care. J Health Organ Manag.
2013;27:134-42.
21. Sandars J. The use of reflection in
medical education: AMEE Guide No. 44. Medical Teacher.
2009;31:685-95.
22. Schippers MC, Edmondson AC, West MA.
Team reflexivity as an antidote to team
information-processing failures. Small Group Research.
2014;45:731-69.
23. O’Connell MT, Pascoe JM.
Undergraduate medical education for the 21st century:
Leadership and teamwork. Fam Med. 2004;36: S51-6.
24. Gaufberg EH, Batalden M, Sands R, et
al. The hidden curriculum: what can we learn from third-year
medical student narrative reflections? Acad Med.
2010;85:1709-16.
25. Chen TY. Medical leadership: An
important and required com-petency for medical students. Ci
Ji Yi Xue Za Zhi. 2018;30:66-70.
26. Houghton JD, Dawley D, DiLiello TC.
The abbreviated self-leadership questionnaire (ASLQ): A more
concise measure of self-leadership. Int J Leadership
Studies. 2012;7:216-32.
27. Clyne B, Rapoza B, George P.
Leadership in undergraduate medical education: Training
future physician leaders. R I Med J. 2015;98:36-40.
28. Trastek VF, Hamilton NW, Niles EE.
Leadership models in health care-case for servant
leadership. Mayo Clinic Proceedings. 2014;89:374-81.
29. Stoller JK. Developing physician
leaders: A perspective on rationale, current experience, and
needs. Chest. 2018;154:16-20.
30. Judge TA, Bono JE. Five-factor model
of personality and transformational leadership. Journal of
Applied Psychology. 2000;85: 751-65.
31. Chaudry A, Amar Sodha AN. Expanding management and
leadership education in medical schools. Adv Med Educ Pract.
2018;9:275-78.
|
|
|
 |
|

