|
|
|
Indian Pediatr 2018;55: 69 -70 |
 |
Trypanosomiasis in a Young Infant from Rural
Gujarat, India
|
|
Dilip Bharodiya 1,
Tanu Singhal2, GS
Kasodariya1, PS
Banerjee3 and
Rajat Garg3
From 1Department of Pediatrics, Apple Hospital, Surat;2Kokilaben
Dhirubhai Ambani Hospital and Medical Research Institute, Andheri West,
Mumbai; and 3ICAR-Indian Veterinary Research Institute,
Izatnagar, UP; India.
Correspondence to: Dr. Tanu Singhal, Department of
Pediatrics, Kokilaben Dhirubhai Ambani Hospital and Medical Research
Institute, Andheri West, Mumbai, India.
Email: tanusinghal@yahoo.com
Received: December 25, 2016;
Initial review: December 27, 2016;
Accepted: October 10, 2017.
|
Background: Human trypansomiasis due to infection
by animal trypanosomes is rarely reported from India. Case
characteristics: We describe clinical presentation of a 2-month-old
boyfrom a rat infested house in rural Gujarat who was diagnosed to be
havinginfection with the rodent parasite Trypanosoma lewisi.
Observation: The fever and parasitemia resolved on treatment with
liposomal amphotericin B, Ceftriaxone and Amikacin, and there was no
recurrence of parasitemia over a 2 month follow-up. Message: The
case highlights the need for increased awareness and heightened
surveillance for this rare zoonotic infection.
Keywords: Protozoa, Pyrexia of unknown origin, T. Lewisi.
|
|
T
rypanosomes are flagellated protozoans affecting
humans and animals. Human trypanosomiasis is endemic in Africa as
sleeping sickness (caused by Trypanosoma brucei) and Latin
America as Chagas disease (caused by T. cruzi). Human
trypanosomiasis is not known to exist in India. However, animal
trypanosomiasis is endemic in India, and is caused by either T.
evansi in cattle/ horses (causing a disease called "surra") or T.
lewisi in rats [1]. Only sporadic cases of human infection with
animal trypanosomes have been reported from India. We report the case of
a young infant who had T. lewisi infection.
Case Report
A 2-month-old infant born to farmer parents of
lower-middle socioeconomic status in Dhari village of Amreli district of
Gujarat presented to a private hospital in Surat with history of fever
of 5 days duration. The mother reported an insect/flea bite (common in
cattle and termed as "itardi" in local language) in the infant’s axilla
about 2 weeks prior to this episode of fever.The insect was removed
following which there was some local bleeding but thereafter the baby
was asymptomatic. There was a history of the house being infested by
rats. At presentation, the baby was playful and active but had pallor
and hepatomegaly. Routine investigations revealed hemoglobin (Hb) of 8.3
g/dL, total leucocyte count of 10.5×10 9/L,
platelet count of 130×109/L
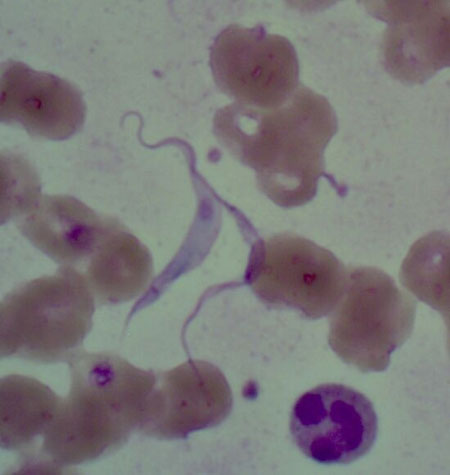
and an elevated ALT (582 IU/l). A peripheral smear, sent for malarial
parasite, incidentally showed flagellated parasites suggestive of
Trypanosoma (Fig. 1). Blood samples, peripheral smears
and filter paper samples were sent to the ICAR – Indian Veterinary
Research Institute (IVRI) at Izatnagar, UP for confirmation and
identification.
 |
|
Fig.1 Peripheral smear showing
flagellated parasites with subterminal kinetoplast resembling
trypanosoma.
|
The child was hospitalized, blood cultures were sent,
and therapy with ceftriaxone, amikacinand liposomal amphotericin B was
initiated. This treatment was for presumed bacterial sepsis and
trypanosomiasis based on experience from a previous similar case
reported from India [2]. We could not procure pentamidine and
suramin.The baby was followed up clinically and with daily blood counts,
Alanine aminotransferase (ALT) and peripheral smear. Over the next five
days, the hemoglobin dropped from 8.3 g/dL to 6.9 g/dL but platelet
count increased to 522×109/L.
The ALT levels increased to 1120 IU/L. The peripheral smear showed
reduction in parasitemia from 3-4 parasites per high power field to 1
parasite per 3-4 fields by day 3 and no parasites by day 5 of treatment.
Antimicrobials were stopped after 5 days and the baby was discharged. A
week later, the liver enzymes had normalized and there was sustained
absence of parasites.The child was well over the next 2 month follow-up
period with no reappearance of parasitemia. The hemoflagellate in the
smear was identified as T. lewisi on the basis of morphology and
PCR amplification of ITS1 region with flanking 18S and 5.8S rRNA (Web
Fig.1).
Discussion
The clinical differentials in this young febrile
infant were bacterial sepsis, malaria or viral fever. The diagnosis of
trypanosomiasis was unanticipated, surprising and incidental as this
parasitic infection in humans is very rare in India. The characteristic
morphology and the PCR made the diagnosis unequivocal. However, as the
baby cleared the fever and infection without any trypanocidal drugs, a
causal association between the parasite and the febrile illness is
difficult to establish.
Theoretically, infection of humans with animal
trypanosomes cannot occur because of a trypanolytic factor
apolipoprotein L1 present in human serum [1]. Human infection with T.
evansi was first reported by Joshi, et al. [3] in an
immunocompetent adult from rural Nagpur, India. This patient was
successfully treated with suramin, a drug used for treatment of human
African trypanosomiasis [3]. Authors hypothesized that the patient was
infected through a wound in the index finger while delivering infected
cattle or through bite by Tabanidstriatus flies that transmit
infection in animals. Subsequent to this case, a serologic study was
conducted in the same village that showed that the sera of 81 of 1806
people (4.5%) were seropositive for T. evansi infection by the
card agglutination test but none had parasitemia on peripheral blood
[4].
In India, infection with T. lewisi has been
reported more frequently than T.evansi [1,2,5-7]. It is
postulated that infection is transmitted to humans from infected rats
through bite of rat fleas or contamination of open wounds with rat
feces. Shrivastava, et al. [5] in 1974 reported two cases in
adults from Raipur who recovered spontaneously [5]. Shah, et al.
[7] reported a 6-week-girl living in a rat-infested flat in urban Mumbai
who presented with fever, hepatosplenomegaly, anemia, thrombocytopenia
and hepatitis; and trypanosomes morphologically resembling T. lewisi
were detected in blood. She recovered spontaneously over a 2 week
period. Verma, et al. [2] reported a case of a 37-day-old infant
from Uttar Pradesh who presented with fever, lethargy and convulsions,
and who had a history of painful insect bite the day before admission
[2]. Treatment was initiated with ceftriaxone (for presumed sepsis) and
liposomal amphotericin B (since it works for Leishmania), and later
pentamidine. The parasitemia disappeared on day 7 of admission (2 days
after starting pentamidine).
Our index case and those reported earlier probably
reflect the tip of the iceberg of this possibly self-resolving
infection. Nonetheless, it is important to increase awareness of this
entity to ensure early diagnosis, avoidance of potentially toxic anti-trypansomal
therapy in stable and improving patients, and more importantly to detect
any change in disease epidemiology of this rare zoonotic infection.
Acknowledgements: Kirit Naik and Frenil Munim for
their contribution in clinical care of the infant.
Contributors: DB: pediatrician incharge of
clinical care and preparing the case summary; TS: opined on the strategy
for management and prepared the manuscript. GSK: pathologist who first
identified the trypansoma on the peripheral smear and participated in
preparing the manuscript. PB and RG: identified the parasite as T.
lewisi on basis of morphology and by PCR, and provided critical
inputs to the preparation of the manuscript.
Funding:None Stated; Competing interest:
None.
References
1. Joshi PP. Human trypanosomiasis in India: is it an
emerging new zoonosis? In: Munjal YP, Editor, API Textbook of
Medicine. 9thedition. New Delhi:Jaypee Brothers; 2013.p.10-13.
2. Verma A, Manchanda S, Kumar N, Sharma A, Goel M,
Banerjee PS, et al. Trypanosoma lewisi or T. lewisi-like
infection in a 37-day-old Indian infant. Am J Trop Med Hyg.
2011;85:221-4.
3. Joshi PP, Shegokar VR, Powar RM, Herder S, Katti
R, Salkar HR, et al. Human trypanosomiasis caused by Trypanosoma
evansi in India: the first case report. Am J Trop Med
Hyg.2005;73:491-5.
4. Shegokar VR, Powar RM, Joshi PP, Bhargava A, Dani
VS, Katti R, et al. Human trypanosomiasis caused by Trypanosoma
evansi in a village in India: preliminary serologic survey of the
local population. Am J Trop Med Hyg. 2006;75:869-70.
5. Shrivastava KK, Shrivastava GP. Two cases of Trypanosoma (Herpetosoma)
species infection of man in India. Trans R Soc Trop Med Hyg. 1974;68:3-4.
6. Doke PP,Kar A. A fatal case of Trypanosoma
lewisi in Maharashtra, India. Ann Trop Med Public Health.
2011;4:91-5.
7. Shah I, Ali US, Andankar P, Joshi RR. Trypanosomiasis in an infant
from India. J Vector Borne Dis. 2011;48:122-3.
|
|
|
 |
|

