The Government of India has recently released the
National and State level factsheets of the Rapid Survey on Children (RSoC)
that was conducted jointly by the Ministry of Women and Child
Development and UNICEF [1]. This state-level dataset was awaited as it
is about a decade from the previous comparable data from the third
National Family Health Survey (NFHS-3) in 2005-06 [2]. The recently
released Global Hunger Report and the Global Nutrition Report portend
some of these gains [3,4]. We focus on two key aspects: (i) the
emerging trends, and (ii) and the contemporary policy discourse.
What’s Up and What’s Down?
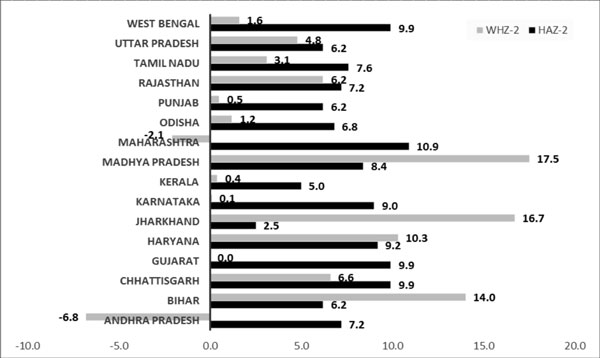
There is a significant improvement in the child
malnutrition levels between NFHS-3 and the RSoC. The prevalence for
stunting in under-five children has decreased from 48% to 38.7%; and
there is also a decline in prevalence of underweight (42.5% to 29.4%)
and wasting (from 19.8% to 15.1%). The absolute levels of child
malnutrition continue to be high. Most states showed improvements in
levels of stunting; remarkable gains (among the large states) were noted
in Andhra Pradesh, Chhattisgarh, Gujarat, and Madhya Pradesh. Jharkhand
reported very little improvement in stunting (2.5%) but large gains in
wasting (16.7%) (Fig. 1).
 |
|
Fig. 1 Percentage changes between
NFHS3 and RSOC in stunting and wasting.
|
The distribution of stunting and wasting in states
showed interesting shifts. With declines in stunting, some states have
recorded higher prevalence of wasting, a phenomenon noted as well in the
changes between NFHS-2 and NFHS-3. Table I shows the
distribution by RSoC data by following the earlier method of mapping
inter-state distribution of acute and chronic malnutrition by computing
terciles for wasting and stunting and tracking the changes in their
respective positions [5,6]. A notable change is Bihar and Gujarat
switching places between high wasting and high stunting category and
medium wasting and high stunting category. This is explained by Gujarat
reporting no change in the status of wasting despite an impressive 9.9
percentage point improvement in stunting. With decreases in stunting,
quite a few states now feature in the axis of high wasting (Table
I).
|
TABLE I Distribution of Stunting and Wasting
Across States |
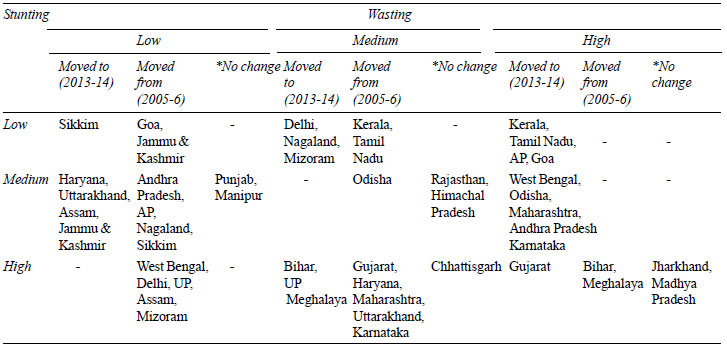
* from NFHS-3 (2005-06) to RSoC (2013-14); UP: Uttar Pradesh;
AP: Arunachal Pradesh. |
A comparison of levels of stunting in Indian and
African children with similar multi-dimensional poverty index is
instructive - Bihar (49.4%) and Liberia (42%) / Sierra Leone (45%);
Jharkhand (47.3%) and Angola (29%) / Mozambique (43%); Madhya Pradesh
(41.6%), Chhattisgarh (43%), Uttar Pradesh (50.6%) and Senegal (19%)/
Malawi (48%)/ D R Congo (25%). The South Asian Enigma therefore
continues (despite recent declines), and requires an understanding
beyond anthropometric indicators.
There is large-scale improvement in exclusive
breastfeeding rates among children under six months of age (from 46.4%
to 64.9%). Of concern is the decline in infant and young child feeding
(IYCF) practices; this was already quite poor. The proportion of
children aged 6-23 months who had a minimum dietary diversity has
significantly gone down. The NFHS reports minimum dietary diversity
separately for breastfed and non-breastfed children (the average of both
has been reported here). The RSoC factsheet on the other hand has not
made such a distinction. The full report and data may clarify if there
is an issue of definitional inconsistencies between the two surveys.
What’s not new?
High levels of stunting indicate continuing
large-scale prevalence of chronic malnutrition. Other correlates of
social determinants such as open defecation and sanitation, while
recording some improvement, continue to be abysmally low. Critical
indicators that continue to be worrying are low birth weight, early age
at marriage and low adolescent BMI. Equally serious are issues of
complementary feeding, dietary diversity and breastfeeding indicators.
High prevalence of chronic malnutrition with acute
exacerbations exemplifies chronic poverty and multiple deprivations [7].
The percentage of children in the 6-35 months age group accessing
supplementary nutrition is as low as 22.8% in Uttar Pradesh, while it is
much higher at 65.3% in Andhra Pradesh, 70.3% in Himachal Pradesh, 82.8%
in Chhattisgarh and 89.2% in Odisha.
Treatment as an Attractive Illusion
In this epidemiologic backdrop, two news items call
for a careful examination. A civil society collective appealed to
policymakers (in a press release) on July 23, 2015 to "declare
malnutrition as a medical emergency to save India’s children dying of
hunger" [8]. The Press Trust of India quoted the Union Minister for
Tribal Affairs on August 4 that his Ministry will identify and document
medicinal herbs helpful in the treatment of malnutrition [9].
The moot question: can malnutrition be ‘treated’?
Current mainstream global notions draw upon African experiences where
Severe Acute Malnutrition (SAM) is triggered by acute crises such as
drought, crop failure and civil wars. Classical SAM is a medical
emergency (with high risks of mortality) requiring feeding with ready to
use therapeutic foods (RUTF) along with other medical interventions. The
predominant form of malnutrition in India is significantly different
from the classical SAM and standardized protocols for treatment are not
as effective, requiring much longer duration to achieve targeted weight
gains even with RUTF. This is on account of high levels of underlying
stunting. Stunting signifies chronic undernutrition and has no scope for
‘cure’ in a therapeutic mode.
Programmatic implications are thus primarily
two-fold: (i) blend and combine multiple approaches for
management of malnourished children in community and institutional
settings; and (ii) a breadth of interventions to address
multi-dimensional poverty and prevent chronic malnutrition through
long-term and multi-sectoral efforts at building community capacity and
support structures. Critical weaknesses include shortage of
pediatricians even at the district hospital level (recently released
rural health service data point to shortfalls up to 90% in high burden
states), and a cogent strategy for continuum of care [10].
Bridging the Gap
Gaps remain in nutrition programming in the country
at all levels. The release of the much-delayed RSoC data is welcome.
Regrettably, there is no institutional mechanism in place to ensure
regular availability of anthropometric data at national, state and
district levels. The NFHS-4 seems to be indefinitely delayed. The first
step towards meaningful planning and monitoring would be to put in place
a regular and comprehensive nutrition surveillance system and
incorporate it with the Mother and Child Tracking System (MCTS). It is
hoped that this, long with a multi-sectoral comprehensive approach
towards tackling malnutrition in all its forms, is what the long-awaited
National Nutrition Mission will encompass. The Sustainable Development
Goal 2.2 calls for ending all forms of malnutrition by 2030, including
achieving by 2025 the internationally agreed targets on stunting and
wasting in children under five years of age. It’s a rocky road ahead;
difficult, if not impossible!
1. Rapid Survey on Children 2013-2014. India
Factsheet. Provisional. Ministry of Women and Child Development.
Government of India. Available from: http://wcd.nic.in/issnip/National_Fact%20sheet_RSOC%20_02-07-2015.pdf.
Accessed August 29, 2015
2. International Institute for Population Sciences
(IIPS) and Macro International. 2007. National Family Health Survey
(NFHS-3), 2005-06;I:273.
3. Bread for the World Institute. 2015. Global Hunger
Report: When Women Flourish. We can end Hunger. Washington, DC.
4. International Food Policy Research Institute.
2014. Global Nutrition Report 2014: Actions and Accountability to
Accelerate the World’s Progress on Nutrition. Washington, DC.
5. Bergeron G, Castleman T. Program responses to
acute and chronic malnutrition: divergences and convergences. Adv Nutr.
2012;3:242-9.
6. Dasgupta R, Sinha D, Yumnam V. Programmatic
response to malnutrition in India: Room for more than one elephant?
Indian Pediatr. 2014;51:863-8.
7. Alkire S, Santos ME. Acute Multidimensional
Poverty: A New Index for Developing Countries. United Nations
Development Programme Human Development Reports Research Paper 2010.
8. Express Health News Bureau. Civil Society appeals
to policymakers to declare malnutrition as a medical emergency.
9. Press Trust of India. Centre to collaborate with
Ramdev in finding cure of malnutrition: Union Minister Juel Oram.
Available from:
http://www.news18.com/news/uttarakhand/centre-to-collaborate-with-ramdev-in-finding-cure-of-malnutrition-union-minister-juel-oram-781345.html.
Accessed August 20, 2015.
10. Dasgupta R, Yumnam V, Ahuja S, Roy S. The
Conundrum of continuum of care: Experiences from the NRC model, Madhya
Pradesh. Oral presentation at the South Asia Conference on Policies and
Practices to Improve Nutrition Security, SAC-OP-07-05; 2014 July 30-31,
New Delhi, India. Available from:
http://www.nutritioncoalition.in/thematic-oral-presentations.
Accessed June 16, 2014.

