|
|
|
Indian Pediatr 2014;51:
53-54 |
 |
Screw-worm Myiasis of Prolapsed Rectum
|
|
Sunil Rathi, *Kailash
Pednekar, Ashish Pathak and Poonam Singh
From the Departments of Pediatrics and *Surgery, RD
Gardi Medical College, Surasa, Ujjain, India.
Correspondence to: Dr Poonam Singh, Assistant
Professor, Department of Pediatrics, RD Gardi Medical College,
Surasa, 456010 Ujjain, India.
Email:
[email protected]
Received: July 23, 2013;
Initial review: August 22, 2013;
Accepted: October 25, 2013.
|
|
Background: Wound myiasis in the Indian subcontinent is most
commonly caused by old world screw-worm (Chrysomya bezziana).
Case Report and management: A 4-year-old malnourished girl presented
with full thickness rectal prolapse following acute diarrhea with a
large wound and screwworm myiasis of the rectum. Turpentine oil was
applied to immobilize the maggots followed by manual extraction.
Prolapse was successfully treated by manual reduction followed by
strapping of the buttocks. Outcome: Child was thriving well and
gained 2 kg weight in follow up after two weeks. Message: Parents
should be educated about taking care of prolapsed rectum.
Keywords: Chrysomya bezziana, Obligate myiasis,
Rectal prolapse
|
|
M
yiasis occurs commonly in unhygienic
environmental conditions in debilitated patients. Although rectal
prolapse and myiasis are common in tropics, association between the two
has not been described. We report a case of myiasis in prolapsed rectum
in a child.
Case Report
A 4-year-old girl belonging to lower socioeconomic
status presented in the outpatient department with complaints of a mass
protruding from anus for 15 days. It was small and reducible initially
but gradually increased in size and became irreducible. The mother
noticed an ulcer on the right lateral aspect of the mass which was
rapidly enlarging with whitish colored worms crawling into it for 4
days. Child also suffered from acute watery diarrhea for 7 days prior to
above symptoms.
On examination, child was grossly emaciated, pale,
sick looking and febrile. She was weighing 8 kg (weight-for-age below
third centile). On systemic examination, abdomen was soft and bowel
sounds were normal. Local examination revealed full thickness rectal
prolapse with a large cavernous ulcer occupying right half of the
circumference of rectum measuring about 5 cm × 3 cm. The ulcer was
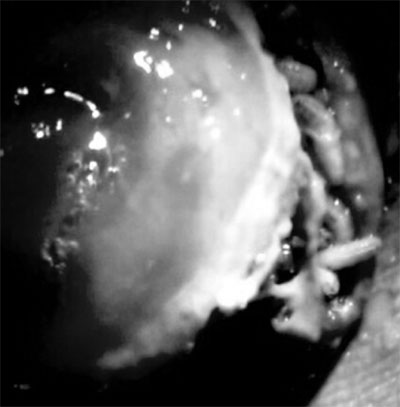
heavily infested with numerous, large actively motile maggots (Fig.
1).
 |
|
Fig. 1 Deep cleft like ulcer on right
lateral aspect of rectum heavily infested with large screw-worm
maggots.
|
Child was admitted; parenteral fluids and antibiotics
were started. Turpentine oil soaked gauze pieces were applied locally
followed by manual extraction of maggots. Wound became maggot free in
four days during which hundreds of whitish briskly motile maggots
measuring 10-18 mm were retrieved. The length and morphology of larva
was suggestive of screw-worm (Chrysomya bezziana) maggots.
Following regular dressing with povidone-iodine,
ulcer healed by 8th day of
admission. Manual reposition of prolapsed rectum was done followed by
strapping of the buttocks for 24 hours. Child was discharged and was
thriving well at follow-up after two weeks.
Discussion
Rectal prolapse is a common condition in children
with a peak incidence around 1-3 years of age [1]. Infestation with
intestinal parasites, malnutrition, acute diarrhea, ulcerative colitis,
pertussis, Ehlers-Danlos syndrome, chronic constipation and
myelomeningocele are some predisposing factors for rectal prolapse
[2,3]. Our patient was undernourished, and developed rectal prolapse
following an acute diarrheal episode. Myiasis may be classified as
obligatory, facultative or accidental [1]. The obligatory parasites
depend on the host for a part of their life cycle [1,4]. The three major
species of obligate parasites implicated for wound myiasis are the New
World screwworm (Cochliomyia hominivorax), the Old World
screwworm, (Chrysomya bezziana) and Wohlfahrt’s wound myiasis fly
(Wohlfahrtia magnifica). Psychiatric illness, immunocompromised
state, exposed wound with foul smelling discharge, vegetative state and
low socioeconomic status are certain predisposing factors for myiasis
[5]. The poor housing condition in this young debilitated child might
have lead to oviposition by the fly on the prolapsed rectal mucosa.
The spices identified in the present case was
Chrysomya bezziana. The adult is a blue-green fly prevalent in
tropical and subtropical countries of Africa and Asia, including India,
Saudi Arabia, Indonesia, the Philippines, Papua, New Guinea, and Persian
Gulf [6]. Adult fly oviposits only on live mammalian tissue, depositing
about 200 eggs at sites of wound or in body orifices such as ear and
nose. The eggs hatch after 12-18 hours liberating the white first-stage
larvae burrowing gregariously, head downwards, into the wound in a screw
worm pattern. The larvae feed voraciously on the living tissue rapidly
expanding the wound. In about four days, the larvae moult into the
second and third stages measuring 10-18 mm. The third-stage larva falls
on the ground to pupate and transforms into adult fly about seven days
later. In our case, there was a rapidly enlarging ulcer explained by
development of third stage larva from the eggs. Screwworm myiasis has
been reported commonly from tropical countries, including India but
rectal involvement has not been reported.
Treatment of myiasis requires removal of all visible
larvae, debridement of the necrotic tissue, irrigation with antiseptic
solution and daily dressing [7]. Fifteen percent chloroform in olive
oil, terpentine oil or ether may be used to immobilize the larvae
facilitating their removal [8]. Rectal prolapse spontaneously resolves
in most of the children; medical management with stool
softeners/laxatives and avoidance of prolonged straining are sufficient.
Contributors: SR: diagnosed and managed the case;
PS and AP: were involved in review of literature and preparation of the
manuscript; SR and PS: prepared the final manuscript. KP: Surgical
management.
Funding: None; Competing interests: None
stated.
References
1. Stafford PW. Other Disorders of the Anus and
Rectum, Anorectal function. In: O’Neill-Pediatric Surgery. 5th
ed. Mosby, Company; 1998. p. 1433-54.
2. Alberto Pena. Surgical Considerations of the
Anus-Rectum and Colon. Nelson Textbook of Pediatrics. 16th ed. W.B
Saunders Company; 2000. p. 1182.
3. Zumpt F. Myiasis in man and animals in the Old
World 1st ed. London: Butterworths; 1965.
4. Arora S, Sharma JK, Pippal SK, Sethi Y, Yadav A.
Clinical etiology of myiasis in ENT: a retrograde period—interval study.
Brazilian J Otorhinolaryngol. 2009;75:356-61.
5. Vitavasiri MDA, Charoenchasri MDP, Kaewmanee MSS,
Bhaibulaya MDM. Subdermal myiasis caused by maggots of Chrysomyia
bezziana. Siriraj Hospital Gazette. 1995;47:419-22.
6. Spradbery JP. Screw-worm fly: a tale of two
species. Agricultural Zoology Reviews. 1994;6:1-62.
7. Sesterhenn AM, Pfützner W, Braulke DM, Wiegand S,
Werner JA, Taubert A. Cutaneous manifestation of myiasis in malignant
wounds of the head and neck. Eur J Dermatol. 2009;19:64-8.
8. Mariwalla K, Langhan M, Welch KA, Kaplan DH.
Cutaneous myiasis associated with scalp psoriasis. J Am Acad Dermatol.
2007;57:51-2.
|
|
|
 |
|

