|
|
|
Indian Pediatr 2017;54:116 -120 |
 |
Behavioral Problems in
Indian Children with Epilepsy
|
|
Om P Mishra, Aishvarya Upadhyay, Rajniti Prasad,
Shashi K Upadhyay and *Satya K Piplani
From Department of Pediatrics and *Division of
Biostatistics, Department of Community Medicine; Institute of Medical
Sciences, Banaras Hindu University, Varanasi, India.
Correspondence to: Prof OP Mishra, Department of
Pediatrics, Institute of Medical Sciences, Banaras Hindu University,
Varanasi 221005, India.
Email: [email protected]
Received: February 05, 2016;
Initial review: March 28, 2016;
Accepted: November 29, 2016.
Published online: December 05, 2016.
PII:S097475591600030
|
Objective: To assess prevalence of behavioral
problems in children with epilepsy.
Methods: This was a cross-sectional study of
children with epilepsy, and normal controls enrolled between July 2013
to June 2015. Child Behavior Checklist (CBCL) was used as a tool to
assess the behavior based on parents reported observation.
Results: There were 60 children with epilepsy in
2-5 years and 80 in 6-14 years age groups, and 74 and 83 unaffected
controls, respectively. Mean CBCL scores for most of the domains in
children of both age groups were significantly higher than controls.
Clinical range abnormalities were mainly detected in externalizing
domain (23.3%) in 2-5 years, and in both internalizing (21.2%) and
externalizing (45%) domains in children of 6-14 years. Younger age of
onset, frequency of seizures and duration of disease had significant
correlation with behavioral problems in both the age groups.
Antiepileptic drug polytherapy was significantly associated with
internalizing problems in older children.
Conclusion: Age at onset, frequency of seizures
and duration of disease were found to be significantly associated with
occurrence of behavioral problems.
Keywords: Child behavior checklist, Co-morbidity, Outcome.
|
|
C
hildren with epilepsy suffer from symptoms of
disease, effect of therapy, risk of recurrence, impairment of brain
function and development of behavioral problems [1]. Psychopathology has
been reported to be associated with epilepsy [2,3]. Psychiatric
disorders can occur in 50-60% of patients with epilepsy [4], and
behavioral co-morbidities to the tune of 43% of cases [5].
Previous studies have reported that these children
have problems of attention, hyperkinesias, thought, low self-esteem,
anxiety and depression [6-10]. Further, cognitive and behavioral
impairments can even occur following a single seizure, and antiepileptic
drugs may also alter behavior to some extent [11].
Previous studies done in children with epilepsy have
addressed a mixed age group (4-16 years) and shown variable results in
different domains [12, 13]; using child behavior checklist (CBCL), a
well standardized tool for detection of behavioral problems in epilepsy
[14,15]. In the present
study, we have assessed behavioral problems in two separate age groups
(2-5 and 6-14 years) using standard CBCL tool for each group and have
tried to find out the differences in pattern of occurrence of behavioral
problems. Additionally, factors associated with development of these
problems were also analyzed in both younger and older age groups.
Methods
This was a cross -sectional study conducted on
children with epilepsy who were recruited from the Epilepsy Clinic and/
or Out Patient Department (OPD) at Institute of Medical Sciences,
Banaras Hindu University, Varanasi. Purposive sampling method was used
for the selection of cases during the period of July 1, 2013 to June 30,
2015. The protocol of the study was approved by institutional ethical
committee, and informed consent was obtained from the parents or
authorized representative of each child.
Children of 2-14 years age group of both gender
having idiopathic epilepsy, defined as history of occurrence of 2 or
more episodes of unprovoked focal or generalized seizures having normal
cranial CT/MRI scan and normal/ abnormal electroencephalogram (EEG)
[16]. Controls were recruited from the OPD of Pediatrics who came for
their routine health check-up and were found healthy, and they belonged
to similar age group as of patients with epilepsy. Exclusion criteria:
Patients with the diagnosis of symptomatic epilepsy syndromes, epileptic
encephalopathy, febrile seizures, cerebral palsy, developmental delay,
mental retardation, neuro-degenerative and metabolic disorders,
neurotuberculosis, and neurocysticercosis were excluded from the study.
Developmental delay was labelled on the basis of
history and developmental assessment, and Binet-Kulshrestha Intelligence
Scale was used for intelligent quotient (IQ) assessment in all cases.
Moderate and severe developmental delay/mental retardation cases were
excluded. Detailed information regarding age of onset, types of seizures
(partial/generalized), frequency, duration of disease, antiepileptic
medications, compliance to treatment, control of seizures and family
history were recorded. The IQ was categorized as average when score was
ranging between 90-109 and below average when it was between 75-89. The
frequency of seizure was defined as per Sabbagh, et al. [17]. All
patients were receiving antiepileptic drugs (phenytoin sodium/ sodium
valproate/ carbamazepine/ clobazam) either as monotherapy or in
combinations of two or three. Children who were admitted for acute
control of seizures were assessed once it was controlled and they were
discharged from the hospital. Contolled seizure was defined as cases who
were seizure free for at least 6 months before assessment and those who
had recurrence of seizures despite antiepileptic medications were
considered as uncontrolled seizure. Revised Kuppuswamy scale was [18]
was used for the assessment of socio-economic status.
Assessment for behavioral problems was done by a
clinical psychologist. The native language of the study population was
Hindi and the questions were translated from English version of CBCL by
a language expert, and same questions were asked to each
parent/caregiver and also to those who could not read, and the responses
were recorded in the three-point scale of the Achenbach CBCL [19]. The
CBCL (2001 version) included 100 items for 2-5 years age-group and 113
for 6-14 years age-group, and parents reported inventory was used for
the study. Parents rated their child’s behavior on a three-point Likert
scales: 0 (not true), 1 (somewhat or sometimes true), and 2 (very true
or often true) and took 30-45 min to complete. The scale has
standardized normative scores for age and gender encompassing behavioral
dimensions such as emotionally reactivity, anxious/depressed, somatic
complaints, withdrawn, sleep problems, attention problems, and
aggressive behavior in 2 to 5 year age group; and anxious/depressed,
withdrawn/depressed, somatic complaints, social problems, thought
problems, attention problems, rule breaking and aggressive behavior
problems in the age group of 6-14 years. It also provided a total
behavior problem score and two second-order factor scores for
internalizing problems (emotionally reactive, anxious/depressed, somatic
complaints, withdrawn and sleep problems) and externalizing behavior
(attention problems and aggressive behavior in younger age group and
rule breaking and aggressive behavior in older children). Counseling was
provided to children and families having clinical range abnormalities,
and non-responders were referred to psychiatrist for pharmacotherapy.
Statistical analysis: Data were analyzed using
SPSS software version 16.0 (Chicago, IL, USA). Student’s t-test was used
to compare the observations of patients with controls. Chi-square test
was applied for comparisons of data of proportions. Yates correction was
done wherever required and relative prevalence with confidence intervals
were also calculated. Pearson’s correlation coefficients were calculated
for the factors such as age of onset, frequency of seizure and duration
of disease and Spearman’s correlation coefficient for antiepileptic drug
polytherapy with the development of behavioral problems. A P
value of <0.05 was considered as statistically significant.
Results
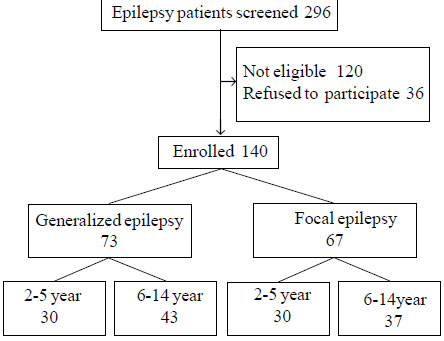
A total of 140 children with epilepsy and 157 healthy
controls in a similar age group were enrolled (Fig. 1),
and were further sub-divided into two age-groups: 2-5 years (60 epilepsy
and 74 controls) and 6-14 years (80 epilepsy and 83 controls). The mean
(SD) age of onset of disease was 2.6 (1.8) years and 4.9 (2.3) years in
2-5 and 6-14 years age-group, respectively. There were 41 males in 2-5
years and 51 in 6-14 years age-groups in cases with epilepsy. In 2-5
years age group, 31(51.7%) received sodium valproate, 10 (16.7%)
phenytoin sodium and 19 (31.7%) cases drugs in combinations (levetiracetam,
carbamazepine/oxcarbamazepine, clobazam); The corresponding figures in
6-14 years age-group were 45 (56.2%), 10 (12.5%) and 25 (31.3%),
respectively.
 |
|
Fig. 1 Details of enrolment of the
children with epilepsy.
|
There were no significant differences as regard to
total behavioral problems between children on monotherapy as compared to
polytherapy in both younger (10.5% vs 17.1 %, P=0.35) as
well as older age groups (35% vs 41.5%, P=0.41),
respectively. A relatively higher percentage of children with below
average IQ had total behavioral problems in comparison to those who had
average IQ in both younger (18.6% vs 13.6%, P=0.96,
relative prevalence (RP) 1.15, confidence interval (CI) 0.25- 5.30) as
well as older age group (49% vs 34%, P=0.15, RP 1.03, CI
0.39-2.75), but the differences were found to be insignificant.
Thirty nine (65%) children in 2- 5 years group and 44
(55%) in 6-14 years had controlled seizures and the rest had
uncontrolled seizures at the time of assessment. In younger age-group,
there was no significant difference in the occurrence of behavior
problems between children with controlled and uncontrolled seizures
(2.5% vs 9.5%, P=0.25, RP 0.18, CI 0.48-12.37). However,
in the older age group, children with uncontrolled seizures had higher
incidence of behavior problems than children with controlled seizures
(50% vs 18.1%, P=0.003; RP 2.44, CI 0.07-0.50). None of
the parents of cases had any history of psychological problems. No
significant differences in mean values of different domains were found
in children on monotherapy versus polytherapy in both age groups.
However, in the 6-14 years age-group, uncontrolled seizures were
significantly (P<0.05) associated with internalizing behavioural
problems.
TABLE I CBCL T Scores in Controls and Children With Epilepsy in 2-5 Years-Age Group
|
Domains |
Controls(n=74) |
Epilepsy(n=60) |
|
†Emotionally reactive |
53.4 (5.0) |
55.5 (5.0) |
|
Anxious/depressed |
52.8 (3.5) |
52.5 (3.4) |
|
Somatic complaints |
51.1 (3.2) |
50.7 (2.5) |
|
#Withdrawn |
51.2 (3.2) |
53.6 (5.9) |
|
Sleep problems |
50.6 (1.4) |
50.9 (2.1) |
|
*Attention problems |
54.6 (5.1) |
61.2 (6.2) |
|
*Aggressive behavior |
54.3 (4.3) |
59.5 (6.7) |
|
Internalizing problems |
45.7 (7.6) |
48.1 (7.6) |
|
*Externalizing problems |
51.4 (7.6) |
60.2 (5.5) |
|
*Total behavior problems |
48.3 (9.1) |
53.0 (5.5) |
|
All values in mean (SD); *P<0.001; #P=0.004,† P=0.021. |
TABLE II CBCL T Scores in Controls and Children With Epilepsy in 6-14 Years Age-group
|
Domains |
Controls |
Epilepsy |
P value |
|
(n=82) |
(n=80) |
|
|
Anxious/depressed |
50.3 (2.4) |
53.9 (5.7) |
<0.001 |
|
Withdrawn/depressed |
55.2 (5.2) |
58.6 (8.6) |
0.003 |
|
Somatic complaints |
56.7 (6.4) |
55.8 (7.2) |
0.788 |
|
Social problems |
53.7 (3.7) |
57.2 (5.7) |
<0.001 |
|
Thought problems |
50.8 (2.3) |
51.0 (3.6) |
0.622 |
|
Attention problems |
53.5 (3.9) |
57.6 (6.0) |
<0.001 |
|
Rule breaking behavior |
53.4 (5.2) |
55.1 (5.8) |
0.021 |
|
Aggressive behavior |
58.9 (7.9) |
65.9 (9.6) |
0.001 |
|
Internalizing problems |
49.4 (7.6) |
53.9 (10.1) |
0.002 |
|
Externalizing problems |
56.3 (7.1) |
61.9 (8.5) |
<0.001 |
|
Total behavior problems |
50.9 (6.2) |
56.6 (7.8) |
<0.001 |
|
All values mean (SD). |
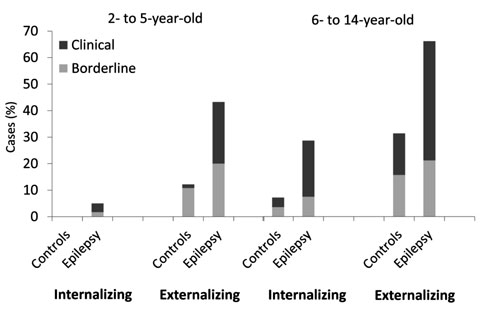
Mean values of behavioral scores in patients with
epilepsy aged 2-5 years were significantly higher as compared to control
in the CBCL domains of emotional reactivity (P=0.021), withdrawn
(P=0.004), attention problems (P<0.001), aggressive
behavior (P<0.001), externalizing (P<0.001) and total
behavior problems (P<0.001) (Table I). In the 6-14
years age group, all the domains showed significantly higher scores in
patients than controls, except somatic complaints and thought problems (Table
II). Further, 23.3% children with epilepsy of 2-5 years had
externalizing behavior scores, and 21.2% and 45% of 6-14 years had
internalizing and externalizing behavior scores in the clinical range,
respectively (Fig. 2).
 |
|
Fig. 2 Internalizing and externalizing
behavioral problems in 2-5 and 6-14 years age-groups in controls
and children with epilepsy.
|
Age of onset of seizure had negative correlations
with total behavior problems (r= -0.289, P<0.05) in 2- 5 years,
and with internalizing (r= -0.230, P<0.05), externalizing (r=
-0.243, P<0.05) and total behavior problems (r= -0.339, P<0.01)
in 6-14 age groups. Frequency of seizure had positive correlations with
externalizing (r=0.41) and total behavior problems (r=0.37)
in younger age-group, and also in older age-group older (r= 0.251 and
0.410, respectively). Duration of disease had positive correlations with
internalizing behavior problems in both younger (r= 0.307) and older age
groups (r= 0.251). Further, in older children, significant positive
correlations were found for antiepileptic drug polytherapy (r= 0.293)
with internalizing behavior problems.
Discussion
In the present study, most of the behavior domains in
children with epilepsy had higher mean scores than controls, but below
the cut-off levels. Externalizing behavioral problems appeared to affect
patients of both the age-groups, but internalizing behavior such as
depression and anxiety were mostly limited to school-age children.
Impaired attention, anxiety, depression,
hyperkinetic, impulsivity, low self-esteem and thought problems are some
of the co-morbidities reported earlier, mostly in mixed age-group of
children [5-7,9]. In
addition, educational underachievement has been also observed in these
children [20]. Behavior problems may not only occur following idiopathic
epilepsy but also due to secondary causes like neurocysticercosis [21].
Abnormal excitability and disrupted synaptic plasticity in the
developing brain can result in epilepsy and subsequently behavior
problems in these patients
[22].
We did not observe any difference in the incidence of
behavioral problems in children with below average IQ in comparison to
cases with average IQ in both the age groups. It may be possible that
effect of IQ was not distinctly seen because of lesser number of cases
in the sub-groups. In contrast, Buelow, et al. [23] observed a
higher risk of occurrence and mean problem scores in cases with low IQ
as compared to patients having middle or high IQ groups, and all types
of problems were found in children with low IQ. Similar to our findings,
Powell, et al. [24] also observed no significant difference in
behavior between children with epilepsy having decreased
seizure-frequency as compared to those with good seizure-control.
A significant effect of age of onset, frequency of
seizures and number of antiepileptic drugs in relation to behavioral
problems have been reported earlier [5,10, 17]. We found younger age of
onset, and frequency of seizures were significantly associated with
behavioral problems. In addition, duration of disease in both age groups
and anti-epileptic drugs in older children also affected the
internalizing problems. However, no difference in behavioural problems
was observed between mono and polytherapy. In contrast, effect of
polytherapy over behavioural problems was found by Datta, et al.
[25] in their patients with epilepsy. It appears that multiple factors
affect the behavioral domains in children with epilepsy. Further, it is
likely that the child’s psychological perception of the disease
situation, especially in older children, could be another contributing
factor to the patient’s behavior during the course of illness. Thus, use
of minimum number of anti-epileptic drugs for seizure-control should be
aimed, to minimize the occurrence of behavioral impairment in these
children.
The strength of the present study is the use of a
standardized validated measurement tool, applied in two age-groups of
population to observe the different behavioral pattern. However, it has
certain limitations as findings are based only on parent-reported
observations. We did not observe the effect of parental educational
level and teacher-report of school-going children, which may limit the
generalizability of the results up to some extent. Further, it would be
also be pertinent to carry out follow-up assessments to document
resolution of problems after discontinuation of treatment.
In conclusion, due attention should be given for
recognition of behavioral co-morbidities in children with epilepsy. They
need periodic assessment during epilepsy treatment and if abnormalities
are detected, may need counseling and also adjustment on behalf of
parents.
Contributors: OPM, AU, SKU: involved in
the design, conduction, analysis of data and drafting of manuscript; RP:
helped in conduct of study and drafting of manuscript; SKP: performed
the statistical analysis of data.
Funding: None; Competing
interest: None stated.
|
What is Already Known?
• Children with epilepsy can develop
behavioral problems in various domains.
What This Study Adds?
• Behavioral co-morbidities differ in
children with epilepsy in different age-groups, with affection
of externalizing behavior in younger children and both
internalizing and externalizing behavior in older age-group.
|
References
1. Malhotra S, Malhotra A. Psychological adjustment
of physically sick children: Relationship with temperament. Indian
Pediatr. 1990; 27:577-84.
2. Jones R, Rickards H, Cavanna AE. The prevalence of
psychiatric disorders in epilepsy: a critical review of the evidence.
Funct Neurol. 2010;25: 191-4.
3. Gaitatzis A, Trimble MR, Sander JW. The
psychiatric co-morbidity of epilepsy. Acta Neurol Scand.
2004;110:207-20.
4. Marsh L, Rao V. Psychiatric complications in
patients with epilepsy: A review. Epilepsy Res. 2002;49:11-33.
5. Choudhary A, Gulati S, Sagar R, Kabra M, Sapra S.
Behavioral comorbidity in children and adolescents with epilepsy. J Clin
Neurosci. 2014; 21:1337-40.
6. Gulati S, Yoganathan S, Chakrabarty B. Epilepsy,
cognition and behavior. Indian J Pediatr. 2014;81: 1056-62.
7. Otero S. Psychopathology and psychological
adjustment in children and adolescents with epilepsy. World J Pediatr.
2009; 5:12-7.
8. Hoare P, Mann H. Self-esteem and behavioral
adjustment in children with epilepsy and children with diabetes. J
Psychosom Res. 1994; 38:859-69.
9. Rodenburg R, Stams GJ, Meijer AM, Aldenkamp AP,
Deković M. Psychopathology in children with epilepsy: A meta-analysis. J
Pediatric Psychol. 2005;30:453-68.
10. Austin JK, Risinger MW, Beckett LA. Correlates of
behavior problems in children with epilepsy. Epilepsia. 1992;33:
1115-22.
11. Aldenkamp AP, Bodde N. Behavior, cognition and
epilepsy. Acta Neurol Scand. 2005;182: S19-25.
12. Kobayashi K, Endoh F, Ogino T, Oka M, Morooka T,
Yoshinaga H, et al. Questionnaire based assessment of behavioral
problems in Japanese children with epilepsy. Epilepsy Behav.
2013;7:238-42.
13. Eom S, Eun SH, Kang HC, Eun BL, Nam SO, Kim SJ,
et al. Epilepsy-related clinical factors and psychosocial
functions in pediatric epilepsy. Epilepsy Behav. 2014;37:43-8.
14. Allison Bender H , Auciello D, Morrison CE,
MacAllister WS, Zaroff CM. Comparing the convergent validity and
clinical utility of the Behavior Assessment System for Children-Parent
Rating Scales and Child Behavior Checklist in children with epilepsy.
Epilepsy Behav. 2008;13:237-42.
15. Gleissner U, Fritz NE, Von Lehe M, Sassen R,
Elger CE, Helmstaedter C. The validity of the Child Behavior Checklist
for children with epilepsy. Epilepsy Behav. 2008;12:276-80.
16. Fisher RS, van Emde Boas W, Blume W, Elger C, Genton
P, Lee P, et al. Epileptic seizures and epilepsy: definitions
proposed by the International League Against Epilepsy (ILAE) and the
International Bureau for Epilepsy (IBE). Epilepsia. 2005;46:470-2.
17. Sabbagh SE, Soria C, Escolano S, Bulteau C,
Dellatolas G. Impact of epilepsy characteristics and behavioral problems
on school placement in children. Epilepsy Behav. 2006;9:573-8.
18. Kumar N, Gupta N, Kishore J. Kuppuswamy’s
socioeconomic scale: updating income ranges for the year 2012. Indian J
Public Health. 2012;56: 103-4.
19. Achenbach TM. Achenbach system of empirically
based assessment (ASEBA). Manual for the child behavior checklist
Pre-school (1.5–5 year), 2000 and School (6–18 year). Burlington, USA:
Research Centre for Children Youth and Families, 2001.
20. Singh H, Aneja S, Unni KE, Seth A, Kumar V. A
study of educational underachievement in Indian children with epilepsy.
Brain Dev. 2012; 34:504-10.
21. Prasad R, Shambhavi, Mishra OP, Upadhyay SK,
Singh TB, Singh UK. Cognitive and behavior dysfunction of children with
neurocysticercosis: a cross sectional study. J Trop Pediatr. 2014;
60:358-62.
22. Brooks-Kayal A. Molecular mechanisms of cognitive
and behavioral co-morbidities of epilepsy in children. Epilepsia.
2011;52:S13–20.
23. Buelow JM, Austin JK, Perkins SM, Shen J, Dunn
DW, Fastenau PS. Behavior and mental health problems in children with
epilepsy and low IQ. Dev Med Child Neurol. 2003;45:683-92.
24. Powell K, Walker RW, Rogathe J, Gray WK, Hunter
E, Newton CR, et al. Cognition and behavior in a prevalent cohort
of children with epilepsy in rural northern Tanzania: A three-year
follow-up study. Epilepsy Behavi. 2015;51:117–23.
25. Datta SS, Premkumar TS, Chandy S, Kumar S,
Kirubakaran C, Gnanamuthu C, et al. Behaviour problems in
children and adolescents with seizure disorder: associations and risk
factors. Seizure. 2005;14: 190-7.
|
|
|
 |
|

