|
Hypothermia, particularly in preterm infants, is
associated with increased morbidity and mortality [1,2]. The
polyethylene wrap is a secure device to pro-mote temperature adaptation
in newborns and it does not interfere with the immediate newborn care or
resuscitation [3]. However, its efficacy in promoting adequate
thermoregulation, with or without prior drying of the newborn in
unclear. Only one previous study has com-pared these two techniques;
however, it was conducted in term neonates and was not randomized [4].
The aim of this study was to determine if the polyethylene wrap is
equally effective for thermoregulation of preterm newborn, with or
without pre-drying versus pre-warmed towels.
Methods
We performed a controlled clinical trial in a General
Hospital in Celaya, Mexico. Infants of 28-37 weeks of gestation, and
weighing 1000-2499 g at birth were included [5]. Infants
suffering from loss of cutaneous integrity, or suspected congenital
heart disease (based on inspection and auscultation
findings such as the presence of cyanosis and abnormal heart rate,
rhythm, regularity, and heart sounds) were not included. The study was
approved by the Institutional Ethics Committee and informed written
consent was obtained from the parents.
We considered 30 infants per group to detect a
significant difference of 0.9ºC in axillary temperature between
preheated field and use of polyethylene bag, with
a=0.05 and
power of 90%.
Immediately after birth, all infants were kept under
a radiant warmer at 36.5ºC (Blosson, Series 900). In group I, infants
were routinely dried with a sterile preheated field (heated under the
radiant warmer for 10 minutes at 36.5ºC), according to the International
Guidelines for Neonatal Resuscitation [6], and wrapped with another
preheated field until they were placed into the incubator where airway
and vital signs were managed conventionally (traditional care). In group
II, they were dried similarly and wrapped with a polyethylene bag. In
group III without previous body drying (only the head was dried), they
were wrapped with the polyethylene bag. Later, all infants were placed
in a single walled incubator (Medix TR 306).
We estimated the time to achieve axillary temperature
(AT) of 36.5ºC and compared AT at 120 minutes from baseline at birth
between all the groups. The incubator temperature was registered at
baseline and every 15 minutes until two hours after birth. Glucose
levels were determined with a (Optium Xceed) monitor and blood pressure
was measured by the flushing technique.
For comparison of continuous variables between
groups, ANOVA test and Sheffé’s test were used. In case of skewed
distribution, we used Krushkal-Wallis and chi-square tests. SPSS
software (version 17) was used.
Results
Birthweight was higher in the preheated field group
than the other groups without difference in other variables (Table
I). No difference was found on heart rate, respiratory rate or blood
pressure levels between groups.
TABLE I Clinical Characteristics of Study Newborns
|
Variable |
Group I ( n=30) |
Group II (n=30)
|
Group III (n=30) |
|
Traditional care
|
Polyethylene bag with
|
Polyethylene bag without
|
|
|
previous drying
|
previous drying |
|
Gender (females/males) |
14/16 |
15/15 |
15/15 |
|
Gestational age (wks) |
35.6 ± 1.68 |
35.2 ± 1.8 |
34.5 ± 2.6 |
|
Weight (g)* |
2173 ± 275 |
2101 ± 319 |
1934 ± 456 |
|
Small for gestational age
|
9 (30%) |
6 (20%) |
8 (26.6%) |
|
Adequate for gestational age
|
21 (70%) |
24 (80%) |
22 (73.3%) |
|
Apgar score (5 min) |
9.0 (5-9) |
9.0 (7-9) |
9.0 (7-9) |
|
Mode of delivery |
|
|
|
|
Eutocic delivery |
4 (13.3%) |
9 (30%) |
8 (26.7%) |
|
Distocic delivery |
1 (3.3%) |
1 (3.3%) |
1 (3.3%) |
|
Elective Cesarean delivery |
14 (46.7%) |
9 (30%) |
9 (30%) |
|
Urgent Cesarean delivery |
11 (36.7%) |
11 (36.7%) |
12 (40%) |
|
Complications |
|
|
|
|
Gestational diabetes mellitus
|
– |
– |
1 (7.1%) |
|
Preeclampsia/Eclampsia |
3 (37.5%) |
2 (18.2%) |
6 (42.9%) |
|
Premature rupture of membranes |
2 (25%) |
6 (54.5%) |
4 (28.6%) |
|
Other |
3 (37.5%) |
3 (27.3%) |
3 (21.4%) |
|
Glucose at birth (mg/dL) |
70.0 (56.0-98.0) |
66.0 (49.0-77.0) |
69.5 (56.2-81.2) |
|
Glucose at 120 min# (mg/dL) |
64.0 (48.5-79.0) |
67.5 (47.5-99.0) |
97.0 (58.0-159.0) |
|
Data are shown as mean±SD, median (interquartile range) or
as proportions according to the variable distribution;
*Significant difference between group I and III (P=0.04); #of
extrauterine life. |
Axillary temperature in the to groups at different
time intervals is depicted in Table II. Both groups of
polyethylene use achieved a mean AT of 36.5ºC at 30 minutes compared
with 75 minutes for the group of traditional care (Table II).
However, no difference was found in AT between those newborns that were
small or adequate for gestational age. Hypothermia was reported in 5
(16.6%) newborns in group I, and their gestational age was not different
from the rest of the group (34.1±2.7 vs 34.7± 2.4; P=0.59).
One case of hyperthermia was found in the polyethylene bag without
previous drying (37.7ºC). None of the neonates in whom polyethylene bag
was used developed lesion of the skin or infection. Incubators in all
cases started at 34ºC. However, temperature of the incubator at 120
minutes, was higher in group I (35.15±0.89ºC) than group II
(34.20±1.14ºC) and III (34.20±0.75ºC) (P=0.0001).
TABLE II Comparison of Axillary Temperature Between Groups
|
Axillary
|
Group
I
|
Group
II Polyethylene
|
Group
III Polyethylene
|
P
|
|
temperature
|
Traditional
|
bag
with previous drying
|
bag
without previous
|
value
|
| at |
care
(n=30) |
(n=30) |
drying
(n=30) |
|
| birth |
36.4 ± 0.51 |
36.3 ± 0.40 |
36.4 ± 0.41 |
0.49 |
| 15 minutes |
36.2 ± 0.41 |
36.4 ± 0.33 |
36.4 ± 0.37 |
0.11 |
| 30 minutes |
36.2 ± 0.41 |
36.5 ± 0.29 |
36.5 ± 0.36 |
0.01
|
| 45 minutes |
36.3 ± 0.44 |
36.5 ± 0.32 |
36.6 ± 0.34 |
0.001
|
| 60 minutes |
36.3 ± 0.44 |
36.6 ± 0.31 |
36.7 ± 0.38 |
0.001
|
| 75 minutes |
36.5 ± 0.42 |
36.7 ± 0.33 |
36.8 ± 0.47 |
0.001
|
| 90 minutes |
36.5 ± 0.41 |
36.8 ± 0.29 |
36.9 ± 0.46 |
<0.001
|
| 105 minutes |
36.6 ± 0.39 |
37.0 ± 0.33 |
37.0 ± 0.39 |
<0.001
|
| 120 minutes |
36.7 ± 0.37 |
37.1 ± 0.26 |
37.0 ± 0.31 |
<0.001 |
 |
|
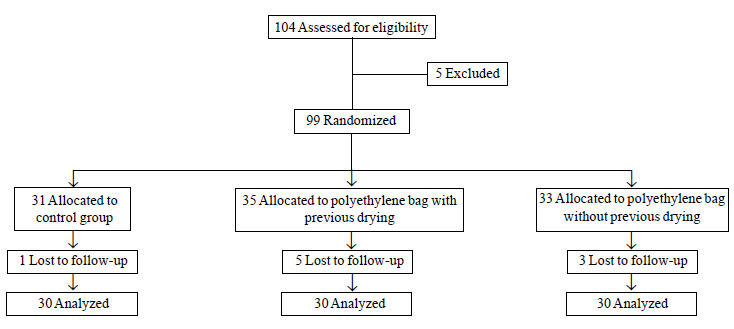
Fig. 1 Flow diagram depicting the
distribution of newborns in the three groups.
|
Discussion
We have confirmed that polyethylene occlusive skin
wrapping immediately after birth in preterm infants provides better
thermal protection in the delivery room than conventional drying,
independently of previous body drying or not. The polyethylene bag was
placed immediately after birth until two hours after birth in our study,
compared with previous studies where the bag was placed at different
times after birth [3,6-10]. Furthermore, all these studies only
compared traditional care and one group of intervention (with or without
previous drying), and studied infants of different birthweight and
gestational age. Vohra, et al. [7] found better corporal
temperature in the intervention group in those <28 weeks of gestational
age (difference = 1.9ºC, P<0.001) but Duman, et al. [6]
found this difference in both <28 weeks and >28 weeks of gestational
age. In our study, the thermal protection of the polyethylene bag was
independent of the stratification of birthweight according to
gestational age.
In addition to the more appropriate control of the
temperature in those infants who used the polyethylene bag, none had
hypothermia and only one had hyperthermia, contrary to the group with
the traditional care where five infants had hypothermia. Previous
reports also found higher proportion of hypothermia in infants with the
traditional care, and a borderline increase in hyperthermia [3,9]. The
risk of overheating is a potential concern when using the polyethylene
wrap and it has to be monitored. Care should be taken to avoid
hyperthermia, especially in those infants who are at risk of hypoxic
ischemic encephalopathy [11]. The wrap procedure was well accepted by
the neonatal staff and did not interfere with resuscitation in the
delivery room.
Contributors: CLM and AN concieved and designed
the study and revised the manuscript for important intellectual content.
The AN will act as guarantor of the study. GML and JMG analyzed the data
and helped in manuscript writing. The final manuscript was approved by
all authors.
Funding: None; Competing interests: None
stated.
|
What This Study Adds?
• Polyethylene film wrapping helps to correct
hypothermia in preterm infants independently of previous body
drying.
|
References
1. Mullany LC, Katz J, Khatry SK, LeClerq SC,
Darmstadt GL, Tielsch JM. Neonatal hypothermia and associated risk
factors among newborns of southern Nepal. BMC Med. 2010;8:43.
2. Watkinson M. Temperature control of premature
infants in the delivery room. Clin Perinatol. 2006;33:43-53.
3. Vohra S, Roberts R, Zhang B, Janes M, Schmidt
B. Heat loss prevention in the delivery room: A randomized
controlled trial of polyethylene occlusive skin wrapping in very
preterm infants. J Pediatr. 2004;145:750-3.
4. Mena P, Meneses R. Termoregulación del recién
nacido (Thermoregulation of the newborn). Rev Chil Pediatr.
2002;73:184-91.
5. Norma oficial Mexicana NOM-007-SSA2-1993.
Atención de la mujer durante el embarazo, parto y puerperium y del
recién nacido (The woman’s attention during the pregnancy,
childbirth and puerperio and of the newborn). Available from:
http://www.salud.gob.mx/unidades/cdi/nom/007ssa23.html. Accessed May
8, 2009.
6. Duman N, Utkutan S, Kumral A, Koroglu TF,
Ozkan H. Polyethylene skin wrapping accelerates recovery from
hypothermia in very low-birthweight infants. Pediatr Int. 2006;48:
29-32.
7. Vohra S, Frent G, Campbell V, Abbott M, Whyte
R. Effect of polyethylene occlusive skin wrapping on heat loss in
very low birth weight infants at delivery: A randomized trial. J
Pediatr. 1999;134:547-51.
8. Gathwala G, Singh G, Kunal, Agrawal N. Safety
and efficacy of vinyl bags in prevention of hypothermia of preterm
neonates at birth. Indian J Public Health. 2010;54:24-6.
9. Lenclen R, Mazraani M, Jugie M, Couderc S,
Hoenn E, Carbajal R, et al. Use of a polyethylene bag: a way
to improve the thermal environment of the premature newborn at the
delivery room. Arch Pediatr. 2002;9:238-44.
10. Rohana J, Wan Khairina W, Boo N, Shareena I.
Reducing hypothermia in preterm infants with polyethylene wrap.
Pediatr Int 2010; Nov 24. [Epub ahead of print].
11. Gunn AJ, Bennet L. Is temperature important in delivery room
resuscitation? Semin Neonatol. 2001;6:241-9.
|

