|
|
|
Indian Pediatr 2012;49: 17-19
|
 |
Effectiveness of Muskaan Ek Abhiyan
(The Smile Campaign) for Strengthening Routine
Immunization in Bihar, India
|
|
Sonu Goel, *Vishal Dogra, †Satish
Kumar Gupta, PVM Lakshmi, $Sherin
Varkey, $Narottam Pradhan,
Gopal
Krishna and Rajesh Kumar
From the Departments of Health Management, School of
Public Health, PGIMER, Chandigarh; *International Clinical Epidemiology
Network (INCLEN), New Delhi; (Immunization), †UNICEF Office, New Delhi;
$Bihar State UNICEF Office, and
Government of Bihar, Patna.
Correspondence to: Dr Sonu Goel, Assistant Professor
of Health Management, School of Public Health, PGIMER,
Chandigarh 160 012, India.
Email: [email protected].
Received: April 28, 2010;
Initial review: May 13, 2010;
Accepted: October 27, 2010.
Published
online: 2011 March 15.
PII: S097475591000354-1
|
Background: In Bihar State, proportion of fully immunized children
was only 19% in Coverage Evaluation Survey of 2005. In October 2007, a
special campaign called Muskaan Ek Abhiyan (The Smile Campaign)
was launched under National Rural Health Mission to give a fillip to the
immunization program.
Objectives: To evaluate improvement in the
performance and coverage of the Routine Immunization Program consequent
to the launch of Muskaan Ek Abhiyan
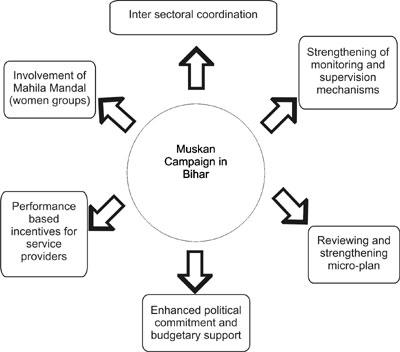
Intervention: The main strategies of the
Muskaan campaign were reviewing and strengthening immunization
micro-plans, enhanced inter-sectoral coordination between the
Departments of Health, and Women and Child Development, increased
involvement of women groups in awareness generation, enhanced political
commitment and budgetary support, strengthening of monitoring and
supervision mechanisms, and provision of performance based incentive to
service providers.
Methods: Immunization Coverage Evaluation Surveys
conducted in various states of India during 2005 and 2009 were used for
evaluation of the effect of Muskaan campaign by measuring the
increase in immunization coverage in Bihar in comparison to other
Empowered Action Group (EAG) states using the difference-in-difference
method. Interviews of the key stakeholders were also done to
substantiate the findings.
Results: The proportion of fully immunized 12-23
month old children in Bihar has increased significantly from 19% in 2005
to 49% in 2009. The coverage of BCG also increased significantly from
52.8% to 82.3%, DPT-3 from 36.5 to 59.3%, OPV-3 from 27.1% to 61.6% and
measles from 28.4 to 58.2%. In comparison to other states, the coverage
of fully immunized children increased significantly from 16 to 26% in
Bihar.
Conclusions: There was a marked improvement in
immunization coverage after the launch of the Campaign in Bihar.
Therefore, best practices of the Campaign may be replicated in other
areas where full immunization coverage is low.
Key words: Evaluation, Immunization, India, Inter-sectoral
coordination, Performance-based incentives.
|
|
Bihar had the second largest
pool of susceptible children in India in year 2001 and routine
immunization (RI) rates have been substantially below national average
[1]. Fully immunized children in the 12-23 months age group was 11.6% in
NFHS-2 and 32.8% in NFHS-3 [2,3]. In eleven districts of the state,
immunization coverage in fact had declined in 2002-04 (DLHS-2) [4]
compared to 1998-2000 (DLHS-1) [5]. Coverage of BCG was 36% in NFHS-2
indicating poor access to immunization services [2]. These findings
indicated a strong need to focus greater efforts on strengthening
immunization in the state. Therefore, Health and Family Welfare
Department of Government of Bihar with the support of Bihar State Office
of UNICEF launched a special campaign in October 2007 called Muskaan
Ek Abhiyan (The Smile Campaign) to give a major fillip to the RI
program. The aim of this study was to evaluate improvement in the
performance and coverage of the Routine Immunization programme
consequent to the launch of Muskaan Ek Abhiyan.
Methods
This observational study was conducted by collecting
program data retrospectively to measure the impact of a package of
interventions implemented under the Muskaan Ek Abhiyan
campaign in Bihar, which were over and above the ongoing routine program
efforts. The study design involved comparison of the immunization
coverage before and after the launch of Muskaan campaign in Bihar
with other Empowered Action Group (EAG) states in the corresponding
period.
Campaign Interventions
The Campaign was guided by the Plan of Action of
National Rural Health Mission (NRHM) prepared by the Bihar Health
Society with the technical support of UNICEF and the National Polio
Surveillance Project (NPSP) supported by WHO [1]. The goal of the
campaign was to provide timely and safe immunization with all antigens
to all eligible children and pregnant women throughout the state. The
guiding principles of the plan were to increase access by increasing the
number and reach of immunization sessions, decreasing the drop outs,
increasing the demand, improving management, and intensifying
supervision for achieving and sustaining high immunization coverage. The
interventions implemented in the Campaign are detailed in Fig. 1.
 |
|
Fig. 1 Interventions during Muskaan
campaign in Bihar.
|
Reviewing and strengthening micro-plans:
Traditionally, Routine Immunization (RI) sessions were held at sub
centers on every Wednesday and in one anganwadi center (AWC) on every
Saturday. The micro plan was revamped and Auxiliary Nurse Midwife (ANM)
also conducted RI sessions on every Friday in 2 to 3 AWCs. In first
phase of Muskaan (October 2007 to August 2009), immunization
sessions were also based at health facilities and AWCs. However, in the
second phase (September 2009 onwards), immunization sessions were also
extended to villages and hamlets where health facility/ AWC’s did not
exist. The revised microplan ensured that all AWCs are covered at least
once every month. Anganwadi workers (AWWs) and Accredited Social Health
Activist (ASHA) of the AWC mobilized the pregnant women and children
using the tracking register. ANMs recorded the service delivered in the
vaccination session on reporting formats, MCH and immunization
registers. After the session, AWW and ASHA updated the tracking
registers on the same day or latest by the next immunization session. In
addition to routine immunization activity, three rounds of special
immunization weeks were carried out throughout the State from December
2006 to April 2007 to reach all vulnerable areas. A special post-flood
catch-up immunization campaign was carried out in the five most flood
affected districts of Bihar following massive floods in year 2007.
Intersectoral co-ordination: Operational strategy
for convergence between Integrated Child Development Scheme (ICDS) and
Health Department was facilitated by joint commitment of the highest
level functionaries in the form of a joint government order which
enforced inter-sectoral coordination. The ANM acted as the team leader
of 5 to 10 AWCs. AWWs and ANMs conducted a time bound cross sectional
house-to-house survey to identify all currently pregnant women and
children in 0–2 year age group. Follow-up surveys were conducted on
monthly basis to identify new pregnancies and newborns. All identified
pregnant women and 0-2 year old children were registered in pregnancy
and newborn tracking registers, respectively. Before each immunization
session, AWW and ASHA conducted mass mobilization activities for
identification and mobilization of eligible children and pregnant women
(based on tracking register) to the immunization site in the village.
Involvement of Mahila Mandals (women groups)
for awareness generation: Mahila Mandal meetings were
organized on third Friday of every month for pregnant women and mothers
of young children to create awareness on issues related to health,
immunization, and nutrition. Initially (2007-08), Rs 150 per month was
allocated per AWC per month for Mahila Mandal meeting expenses,
which was later raised to Rs 250 in 2009. However, this grant was
discontinued in phase-2 as the budget allotted for Mahila Mandal
meetings were tagged with the Village Health and Sanitation Committee
(VHSC) funds.
Performance based incentive to service providers:
In phase-1, incentive of Rs 200 per month each for AWW and ASHA and Rs
150 for ANM was provided for coverage above 90%, and Rs 100 each for AWW
and ASHA and Rs 75 for ANM for 80-90% coverage. For coverage of less
than 60%, explanation were sought in their weekly and monthly review
meetings. Under phase-2, the incentive for AWW and ASHA was Rs 200 each
per session for more than 21 beneficiaries, Rs 150 for 16-20, Rs 100 for
11-15 and Rs 50 for 5-10 beneficiaries. Similarly, the incentive for
vaccinators, i.e., ANM was Rs 100 per session for 15 and more
beneficiaries per session and Rs 50 for 1-15 beneficiaries [1].
Enhanced political commitment and budgetary support:
District Immunization Officers and Medical officer In-charges were
trained at state level; who in-turn trained all health workers in their
respective districts. A system of delivering vaccines at the
immunization site through couriers (a person who delivers and brings
back vaccines from the vaccination site on the same day) was implemented
throughout the state. Alternate vaccinators were proposed to counter the
shortage of ANM in year 2007-08. Alternate vaccinators were paid an
honorarium of Rs 350 per session for up to 4 sessions a month (a maximum
of Rs 1400/- per month). Vacant posts of Medical Officers and ANMs were
filled on contractual basis.
Strengthening of monitoring and supervision mechanism:
Updating and cross verification of beneficiaries was envisaged as a core
component of monitoring wherein 2% of all registers had to be verified
by line supervisors. At the level of primary health centers, an
integrated approach to supportive supervision was adopted by Medical
Officers and Integrated Child Development Scheme officials who randomly
verified immunized beneficiaries using tracking registers to release the
monetary incentives. The percentage of sessions held against those
planned was assessed by monitoring whether the vaccine was lifted from
the storage sites and whether ANM, ASHA and AWW were present at the
vaccination site.
At block level, a steering committee consisting of
Medical Officer In-charge, Child Development Project Officer, Senior
Medical Officer, and Health Manager was formed to facilitate
implementation and monitoring of the campaign related activities. At
district level the campaign was under the control of District Health
Society (DHS). The District Magistrate chaired the meetings of the
District Task Force to review the monthly immunization progress report.
A system of regular monitoring was carried out independently by the
state and district officials of Government of Bihar, UNICEF and
NPSP-WHO. The monitoring feedback was sent to Divisional Commissioners
and Regional Deputy Directors of Health for necessary action. Selective
indicators were reviewed weekly by the Executive Director, NRHM.
Monitoring presentations were made to all District Immunization officers
in monthly meetings. The political leadership also maintained a strong
oversight of all campaign activities.
Performance and Coverage Evaluation
National Family Health Survey (NFHS) [2, 3], Rapid
Household Survey (RHS) [6], Immunization Survey of Bihar (ISB) [7],
District Level Household Surveys (DLHS) [4,5,8], and Coverage Evaluation
Surveys (CES) [9-10], conducted by various agencies that used standard
survey methodology were used for assessment of the immunization
coverage. Super-vision reports were also reviewed to ascertain the
quality of immunization services. Interviews of the key stakeholders in
the state were also conducted to substantiate the findings. The data
collection was done from September to December 2009, and analysis was
done in January and February 2010. Informed consent was obtained from
the Government Officials and UNICEF office of Bihar state.
Results
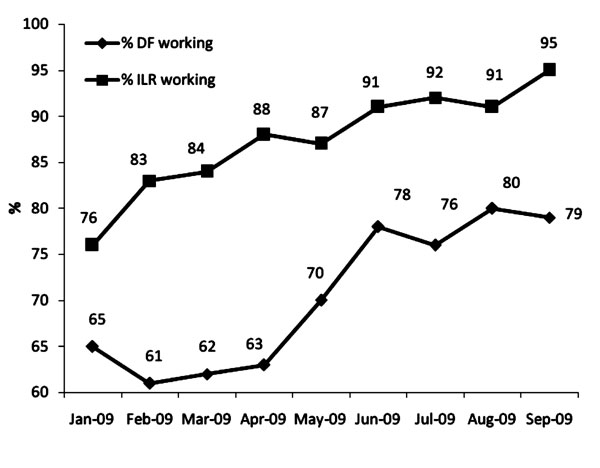
All monitoring indictors related to immunization
performance showed a significant improvement since the launch of the Muskaan
campaign (Table I). It was also found that the
presence of AWW and ASHA workers had increased from 57% and 14% in
2006-07 to 75% and 64% in 2008-09, respectively after the implementation
of the campaign [7]. The functioning of Deep Freezers (DF) and Ice-lined
Refrigerators (ILR) had also improved after the launch of the campaign (Fig.
2). The downtime of various cold chain equipments had decreased
[7].
Table I Monitoring Indicators of Routine Immunization Sessions in Bihar
|
Session indicator |
2005-06 |
2006-07 |
2007-08 |
2008-09 |
|
Sessions held |
91% |
93% |
92% |
91% |
|
Session with |
|
ANM |
91% |
94% |
96% |
95% |
|
ASHA |
0% |
14% |
55% |
64% |
|
AWW |
54% |
57% |
52% |
75% |
|
ANM: Auxiliary Nurse Midwife;
Asha: Accredited Social Health Activitist; AWW: Anganwadi
worker. |
 |
|
Fig. 2 Functional status of Deep freezers and
Ice-lined refrigerators at Primary Health Centers in Bihar.
|
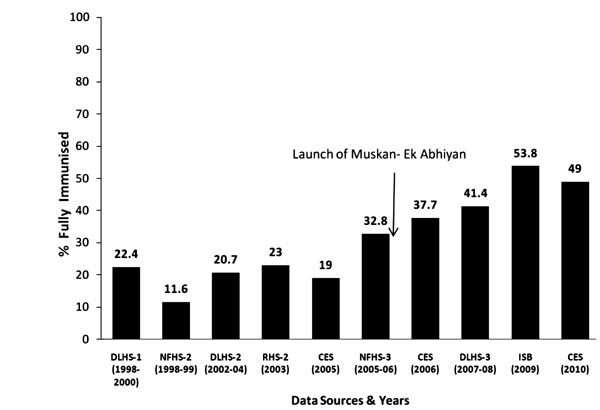
The trend of fully immunized children before and
after the Muskaan campaign is presented in Fig. 3.
The Coverage Evaluation Surveys show that the proportion of fully
immunized children has increased from 19% in 2005 to 49% in 2009 (P<0.001).
The coverage of BCG increased from 52.8% to 82.3% (P<0.001),
DPT-3 from 36.5% to 59.3% (P<0.001), OPV-3 from 27.1% to 61.6% (P<0.001)
and measles vaccine from 28.4% to 58.2% (P<0.001). Between 2005
and 2009, there was a statistically significant improvement (16% to 26%)
in immunization coverage among 12-23 month old children in Bihar as
compared to other EAG states [9,11]
(Table II).
Table II Percentage of Fully Immunized Children (12-23 months) in Empowered Action Group (EAG)
States in Coverage Evaluation Survey 2005 and 2009
| State |
2005a |
2009b |
Difference
d=(b-a) |
*Diff-in-
Diff for Bihar |
| Bihar |
19.0 |
49.0 |
30.0 |
- |
| Chhattisgarh |
44.4 |
57.3 |
12.9 |
17.1 |
| Uttar Pradesh |
33.8 |
40.9 |
7.1 |
22.9 |
| Madhya Pradesh |
38.9 |
42.9 |
4.0 |
26 |
| Orissa |
53.2 |
59.5 |
6.3 |
23.7 |
| Uttaranchal |
61.1 |
71.5 |
10.4 |
19.6 |
| Jharkhand |
45.7 |
59.7 |
14.0 |
16.0 |
| Rajasthan |
49.9 |
53.8 |
3.9 |
26.1 |
*Diff-in-Diff (Difference-in-Difference) = Bihar (column d
first row) – Each State (column d row for each state). It
reflects net increase between 2005 and 2009 in Bihar after
taking into account increase in each of the other states during
the same period; All diff-in-diff were statically significant. |
 |
|
NFHS-National Family and Health Survey, DLHS- District Level
Household Survey, CES- Coverage Evaluation Survey,
ISB-Immunization Survey of Bihar, RHS- Rapid Household Survey
Fig. 3 Fully immunized children (12-23
months) in Bihar.
|
Discussion
The proportion of fully immunized children increased
almost two and a half times after the launch of Muskaan campaign.
Antigen-wise coverage indicates that nearly two third children are being
vaccinated against DPT-3 and measles in Bihar. Several factors such as
the launch of NRHM which has brought additional funding and human
resources (such as ASHAs) may have contributed to this positive change;
however, the package of inter-ventions implemented under the Muskaan
campaign seem to be a key factor behind such positive impact as the
improvements in Bihar were 16 to 26% higher than other EAG states where
NRHM inputs were available over the same time period.
A study in district Yamunanagar in Haryana reported
significant increase in age appropriate immunization coverage with
involvement of Community Health workers and vaccinators, revamping of
micro plans and regular monitoring [11]. It has also been shown in
Indonesia that only training the health workers is not sufficient for
effective routine immunization, but the guidance provided through
supportive supervision has helped in improving various aspects of
immunization such as logistics recording, cold chain management, stock
management, vaccine management and reporting and recording [12]. In this
study also, the supportive supervision mechanism may have helped to
identify the areas of continued weakness which need further on job
training and supervision. Integrated efforts of ICDS and health
department at all levels especially revision of micro plans and hiring
of additional ANMs along with additional day for immunization may have
helped to increase the overall immunization coverage in Bihar. Moreover,
a meticulously planned ‘coverage based incentive’ strategy might also
have worked to increase immunization coverage in Bihar, as it inculcated
a motivation among the service providers and mobilizers at the grass
root level. A global review of performance based incentives by Eichler,
et al. [13]. showed that incentivizing will be effective only
when there is careful planning, implementation, monitoring and
supervision [13]. Muskaan strategy has given importance to all
the components of immunization starting from the planning,
implementation, monitoring and supervision along with provision of
performance based incentives, and political commitment.
The main area of concern has always been to reduce
‘left-outs’ and ‘drop-outs’, which was addressed by tracking registers
and ‘immunization due’ list maintained at sub centre level. In Bihar,
the number of drop-outs and left-outs has decreased since the launch of
Muskaan campaign. It has been observed that improving health
facility practices can increase immunization coverage through reducing
"drop-outs" and "missed opportunities". In Ethiopia, the use of reminder
stickers for parents resulted in nearly 50% decrease in dropout between
DPT1 and DPT3 [14]. The introduction of electronic immunization registry
and tracking system in Rajshahi City Corporation in Bangladesh has
helped in the planning and execution of effective immunization at an
operational level by providing a back-up even if parents forget their
child’s vaccination dates, guiding health workers towards those who need
their doses, and potentially reducing vaccine wastage [15].
Link workers involved as mobilizers encouraged people
to seek immunization services, which were brought closer to the
communities. In our study, the presence of AWW and ASHA workers had
increased after the implementation of the Muskaan campaign.
Similar findings were observed in Bangladesh, where semiliterate and
illiterate local women employed in an urban setting to track defaulters,
to refer them to services and accompany mothers to immunization clinics
has improved immunization coverage rates [16]. In Kenya, school
buildings were utilized as immunization centers, with schoolchildren
circulating immunization information within their communities [17]. In
Nigeria, access to immunization services was improved by increasing the
number of locations offering immunization and adding mobile clinics in
the evenings [18].
It is difficult to extract the effect of individual
interventions of Muskaan campaign. Prospective studies are
required to measure the effect of each intervention; however, it is
often difficult to conduct such studies in program settings. About half
of the children still remain to be immunized against various antigens in
Bihar, and selective use of specific interventions in different district
may reveal the effect of different interventions on the coverage.
Overall, the strategies employed under
Muskaan
campaign seem to be successful in most parts of the state. A key
strength of the model appears to be that the interventions were directed
through existing public health system frontline providers. Improvement
in availability of skilled human resources, quality of microplans,
review of Muskaan registers by supervisors, timely disbursement
of monetary incentives, and inclusion of urban area in micro planning
can further improve immunization coverage in Bihar. Although a sound
supervision mechanism is in place in Bihar, it needs to be sustained in
future as well, since the Muskaan Campaign was very much
dependent on support of partner organizations. A downward trend in
immunization coverage rates was observed in DLHS 2 (2002-04) [4] and in
CES 2009 as well, hence, in-depth review of causes of such reversal
should be looked into so as to sustain the gains in the longer term.
References
1. Bihar State Health Society. Strengthening
Routine Immunizations- Bihar State Action Plan for Routine
Immunization 2005-2010. Available from:
http//statehealthsocietybihar.org/SHS. Accessed on July 16, 2010.
2. International Institute for Population
Sciences (IIPS) and ORC Macro. National Family Health Survey
(NFHS-2). Available from http://www.nfhsindia.org/india2.html.
Accessed on July 16, 2010.
3. International Institute for Population
Sciences (IIPS) and ORC Macro. National Family Health Survey
(NFHS-3). Available from http://mohfw.nic.in/nfhsfactsheet.htm.
Accessed on July 16, 2010.
4. International Institute for Population
Sciences (IIPS). District Level Household and Facility
Survey-2(2002-04). Available from:
http://www.rchiips.org/PRCH-2.html. Accessed on July 16, 2010.
5. International Institute for Population
Sciences (IIPS). District Level Household and Facility
Survey-1(1998-99). Available from:
http://www.rchiips.org/PRCH-1.html. Accessed on July 16, 2010.
6. International Institute for Population
Sciences (IIPS). Rapid Household Survey, Phase-1, under Reproductive
and Child Health Project - India. Mumbai: IIPS, 2000.
7. Immunization Survey of Bihar. Formative
Research and Development Services 2008-09. Available from:
http//www.mohfw.nic.in/NRHM/PIP10_11/Bihar.pps. Accessed on July 16,
2010.
8. International Institute for Population
Sciences (IIPS). District Level Household and Facility Survey-3
(2007-08). Available from: http://www.rchiips.org/ARCH-3.html.
Accessed on July 16, 2010.
9. UNICEF. Review of National Immunization
Coverage. Coverage Evaluation Survey-2005. Available from:
http://www.unicef.org/india/Coverage_Evaluation_Survey_ 2005.pdf.
Accessed on August 10, 2010.
10. UNICEF. Review of National Immunization
Coverage. Coverage Evaluation Survey-2006. Available from:
http://www.unicef.org/india/Coverage_Evaluation_Survey_ 2006.pdf.
Accessed on August 16. 2010.
11. Prinja S, Gupta M, Singh A, Kumar R.
Effectiveness of planning and management interventions for improving
age appropriate immunization in rural India. Bull WHO.
2010;88:97-103.
12. Supportive supervision to sustain health
worker capacity in Nanggroe Aceh Darussalam and North Sumatera.
Available from: http://www.path.org/files/CP _Indonesia_
supp_sprvsn_aceh_fs.pdf. Accessed on April 10, 2010.
13. Eichler R, Levine R. Performance initiatives
for Global health: Potential and Pit Falls. Center for Global
Development Brief. May 2009. Available from:
http//www.festmih.eu/document/1757. Accessed on April 10, 2010.
14. Berhane Y, Pickering J. Are reminder stickers
effective in reducing immunization dropout rates in Addis Ababa,
Ethiopia? J Trop Med Hyg. 1993;96:139-45.
15. Ahmed M. Electronic Immunisation Registry and
Tracking System in Bangladesh. e- Government for Development -
eHealth Case Study. Available from: http://www.
egov4dev.org/health/case/banglaimmune.shtml. Accessed on April 14,
2010.
16. Hughart N, Silimperi DR, Khatun J, Stanton B.
A new EPI strategy to reach high risk urban children in Bangladesh:
urban volunteers. Trop Geogr Med. 1992;44:142-8.
17. Expanded Programme on Immunization: Study of
feasibility, coverage and cost of maintenance immunization for
children by district mobile teams in Kenya. Weekly Epidemiol Rec.
1977;52:197-204.
18. Oruamabo RS, Okoji GO. Immunisation status of children in Port
Harcourt before and after commencing the Expanded Programme on
Immunisation. Public Health. 1987;101:447-52.
|
|
|
 |
|

