|
|
|
Indian Pediatr 2010;47:
198-199 |
 |
Pseudoaneurysm Following Modified Blalock
Taussig Shunt |
|
Syed Ahmed Zaki and Preeti Shanbag,
Department of Pediatrics, Lokmanya Tilak Municipal
General Hospital, Sion, Mumbai, India.
Email:
[email protected]
|
|
The modified Blalock-Taussig (BT) shunt is a common palliative procedure
for congenital cyanotic heart disease (CHD) with diminished pulmonary
blood flow(1). In developing countries, definitive surgery usually gets
delayed due to limited resources and expertise(2). Children with cyanotic
CHD and BT shunt often present to the pediatrician resulting in some of
the complications of BT shunt being misdiagnosed(3,4).
A 1-year-old boy was admitted with cough and fever for
7 days, and breathlessness for 1 day. He was diagnosed to have tetralogy
of Fallot at 3 months of age. Echocardiography revealed a normal
visceroatrial arrangement (situs solitus) and non-restrictive ventricular
septal defect with an overriding aorta. There was infundibular and valvar
pulmonary stenosis and a right-sided aortic arch. At 11 months of age a
left-sided modified BT shunt was done for frequent cyanotic spells. The
present symptoms developed a month after surgery.
On admission, the child was afebrile with heart rate
180/minute, respiratory rate 60/minute with intercostal retractions and
blood pressure 94/52 mm Hg. There was a grade 3/6 ejection systolic murmur
in the 2nd left intercostal space. Bronchial breathing was heard in the
left infraclavicular and axillary areas. The liver was palpable 4 cm and
the spleen 2 cm below the costal margin. Hemoglobin was 12 g/dL and total
leukocyte count was 13,500/cu.mm (polymorphs 85%, lymphocytes15%). Chest
X-ray showed an opacity in the left upper zone. Intravenous
cefotaxime and amikacin were started for a presumptive diagnosis of
pneumonia. Anti-failure management with digoxin and furosemide was
initiated. However there was no improvement even after 7 days. A repeat
chest X-ray showed persistence of the opacity in the left upper
lobe, hence shunt- related pathology was suspected. High-resolution
computed tomography scan of the chest showed regression of the distal end
of the BT shunt from the left pulmonary artery with a large hematoma in
the left upper lobe causing atelectesis of the underlying lung parenchyma
with a shifting of mediastinum to the right. There was aneurysmal
dilatation of the left subclavian artery with a large crescentric thrombus
(Fig.1). The child was taken up for surgical resection of
the pseudoaneurysm. Intraoperatively, the shunt was found to be completely
occluded and the distal end of the
graft had partially dehisced from the anastomotic site. There was
aneurysmal dilatation of the left subclavian artery with a large
crescentric thrombus. However the patient did not survive the procedure.
 |
|
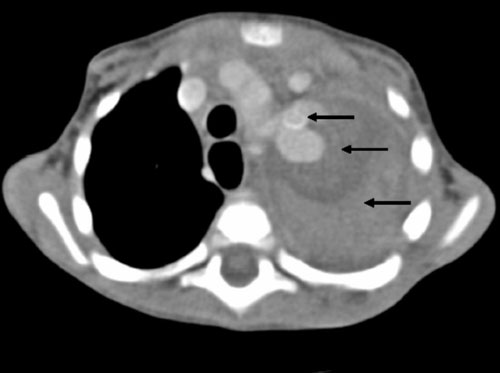
Fig.1
High-resolution computerized tomography scans of
chest showing from above below: Pseudoaneurysm of the BT shunt
(first arrow) with hematoma around the shunt (second arrow) causing
atelactasis of the underlying lung (third arrow). |
Common complications of BT shunt include shunt stenosis
and occlusion, nerve damage at the time of operation, excessive pulmonary
blood flow, serous fluid leak and false aneurysm(3). A pseudoaneurysm
after a modified BT shunt may cause rupture or compression of mediastinal
structures, collapse of underlying lung parenchyma, and shunt occlusion
and bacteraemia. The appearance of a localized mass on the chest film
surrounding the BT shunt requires the exclusion of hematoma, aneurysm, or
inflammation(5). Such patients may be misdiagnosed and treated as
pneumonia.
Through this case we wish to highlight that
shunt-related pathology should be kept in mind when dealing with children
with a BT shunt.
Acknowledgment
Dr Sandhya Kamath, Dean and Dr Anupama Mauskar for
permitting to publish and patient management, respectively.
References
1. Laks H, Marco JD, Willman VL. The Blalock-Taussig
shunt in the first six months of life. J Thorac Cardiovas Surg 1975; 70:
687-691.
2. Rana JS, Ahmad KA, Shamim AS, Hassan SB, Ahmed MA.
Blalock-Taussig Shunt: Experience from the Developing World. Heart Lung
Circ 2002; 11: 152-156.
3. Pongprot Y, Silvilairat S, Woragidpoonpol S,
Sittiwangkul R, Phornphutkul C. Pseudoaneurysm following modified Blalock-Taussig
shunt: a rare complication mimicking pulmonary disease. J Med Assoc Thai
2003; 86:365-368.
4. Coren ME, Green C, Yates R, Bush A. Complications of
modified Blalock- Taussig shunts mimicking pulmonary disease. Arch Dis
Child 1998; 79: 361- 362.
5. Tabaee SA, Rostami A, Givtaj N, Mali S, Pourabasi
SM, Arefi S. Modified Blalock-Taussig Shunt and Giant Perigraft Reaction.
J Teh Univ Heart Ctr 2007; 3: 173-176.
|
|
|
 |
|

