|
|
|
Indian Pediatr 2010;47: 185-187 |
 |
Diaphragmatic Hernia Presenting as
Gastrointestinal Bleeding |
|
Syed Ahmed Zaki, Deepak Dadge, Preeti Shanbag
From the Department of Pediatrics, Lokmanya Tilak
Municipal General Hospital, Mumbai, India.
Correspondence to: Dr Syed Ahmed Zaki, Room No.509,
New RMO quarters, Sion, Mumbai 400 022, India.
Email: [email protected]
Received: November 14, 2008;
Review Initial: December 8, 2008;
Accepted: January 7, 2009.
|
|
Abstract
We report a 5-year-old girl who presented with
persistent iron-deficiency anemia. She had a history of abdominal pain
and recurrent gastrointestinal bleeding. High-resolution computed
tomography, esophagogastroduodenoscopy and barium meal examination
revealed a congenital diaphragmatic hernia with intermittent gastric
volvulus. The anemia was the result of Cameron lesions associated with
diaphragmatic hernia.
Key words: Anemia, Diaphragmatic hernia, Gastric volvulus,
Iron Deficiency.
|
|
D
iaphragmatic hernia with
intermittent gastric volvulus is an uncommon condition in children.
Potential complications such as gastrointestinal bleeding (acute, chronic
and obscure) and anemia make the condition clinically relevant(1). There
are many studies describing adult patients with diaphragmatic hernia
presenting with anemia(2-4). However, diaphragmatic hernia with
intermittent gastric volvulus and gastrointestinal bleeding resulting in
persistent iron-deficiency anemia has never been described in a child. We
report a 5-year-old girl who presented with this condition and was managed
successfully.
Case Report
A 5-year-old female child presented for persistent
anemia not responding to adequate hematinics and blood transfusion. There
was history of abdominal pain and malena, off and on for the last 7
months. There was no history of fever, vomiting, abdominal distension,
constipation, history of trauma to the abdomen, jaundice, or bleeding from
any other site. The diet of the child was adequate in iron-rich foods.
On admission, child was afebrile and hemo-dynamicaly
stable. Severe pallor was present. The weight was 10 kg and height was 82
cm, both below the 5th percentile for age.
There was no icterus, clubbing or petechiae. Abdominal examination
revealed a soft, non-tender liver with a smooth surface and a span of 7
cm. The spleen was not palpable. Other systems were normal. Investigations
revealed a hemoglobin of 4.8 g/dL, total leukocyte count of 13,800/cumm
and platelet count of 6.8 lac/cumm. Hematological indices and peripheral
smear were suggestive of iron-deficiency anemia. Corrected reticulocyte
count was 1.05%. Liver function, renal function tests and serum lactate
dehydrogenase were normal. Stool analysis was normal at this admission.
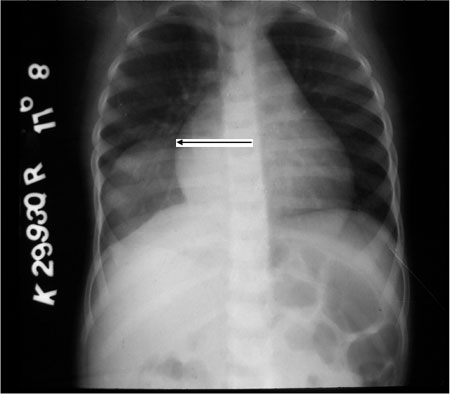
Chest X-ray showed a homogenous opacity in the right lower zone not
silhouetting the cardiac borders (Fig. 1). The patient
underwent esophagogastroduodenoscopy (EGD) which showed multiple linear
gastric erosions on the mucosal folds on the lesser curve of the stomach.
No active bleeding was seen hence no endoscopic therapy was instituted. A
nasogastric tube passed into the stomach without any difficulty.
 |
|
Fig. 1
Homogenous opacity noted in
right lower zone not silhouetting with cardiac border. |
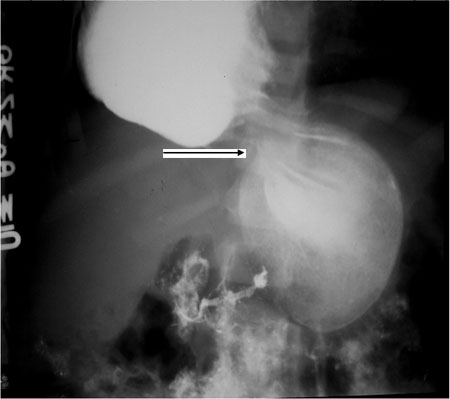
Barium meal showed a mesentrico-axial type of gastric
volvulus with the fundus in the right hemithorax probably through a
diaphragmatic defect and pylorus in left hypochondriac region (Fig.
2). During the test, the gastric volvulus reduced spontaneously
and hence intermittent gastric volvulus with diaphragmatic hernia was
suspected. High-resolution computed tomography of the chest showed
mesentrico-axial volvulus of the stomach with a diaphragmatic defect (type
2) with fundus and body of stomach lying within the right hemithorax. The
patient was transfused with packed red cells. Right thoracoscopy was done
and a 5 cm × 7cm defect in the right dome of diaphragm was closed. The
stomach got reduced spontaneously because of pres-sure created for
thoracoscopy procedure. Post operative recovery was uneventful. The
patient was discharged on oral hematinics and is well on follow up.
 |
|
Fig. 2
Barium meal showing
mesentrico-axial type of volvulus with gastric fundus in the right
hemithorax and pylorus in left hypochondriac region. |
Discussion
Diaphragmatic hernia with gastric volvulus in children
is a rare subtype with only few cases reported in literature. A review of
the literature revealed one such study in which the authors described
three children, all of whom had an acute presentation and had to be
operated on an emergency basis(5). Late
presentation of diaphragmatic hernia as anemia has been described in
adults(2).The cause of anemia has been attributed to Cameron lesions which
are linear gastric ulcers or erosions on the mucosal folds at the
diaphragmatic impression in patients with a large hiatal hernia(6,7).
These gastric erosions can cause iron deficiency anemia from chronic blood
loss.
Gastric volvulus may be idiopathic or secondary to
various congenital or acquired conditions. Among the associated problems,
diaphragmatic defects predominate(8). The presentation can be acute,
chronic, acute-on-chronic or intermittent in type. The clinical symptoms
depend on the degree of rotation and obstruction. Severe epigastric pain
and distension, violent unproductive retching and inability to pass a
nasogastric tube comprise the classical triad of Borchardt(5).
Intermittent type of gastric volvulus may cause diverse gastrointestinal
symptoms in children. In our patient, the chest X-ray done in a
private hospital was normal, the nasogastric tube could be passed into the
stomach easily and stool analysis on admission was normal. This may be
because of spontaneous reduction of the gastric volvulus. Thus
intermittent gastric volvulus causes symptoms intermittently. Routine
investigations done in the asymptomatic period may not reveal any
abnormality and hence diagnosis may be missed.
Treatment of Cameron lesions is primarily medical and
surgery is reserved for refractory cases and a few complicated cases.
Surgical treatment (fundoplication, laparoscopic or open) is recommended
in patients with medically refractory disease, uncontrolled bleeding from
the lesions and in patients in whom the hernia is complicated with
volvulus, incarceration and perforation(1). With growing use of
laparoscopic surgery, patients benefit from a minimally invasive approach
and several authors have reported favourable outcomes after performing
laparoscopic diaphragmatic hernia repairs and gastropexy(9,10).
Acknowledgment
Dr Sandhya Kamath, Dean of our institution, for
permitting to publish and Dr Mamta Manglani, Head of Department of
Paediatrics for her encouragement.
Contributors: SAZ managed the case, reviewed
literature and wrote the paper. DD helped in collecting data and in
literature review. PS critically reviewed and helped in finalising the
article.
Funding: None.
Competing interests: None stated.
References
1. Maganty K, Smith RL. Cameron lesions: Unusual cause
of gastrointestinal bleeding and anemia. Digestion 2008; 77: 214-217.
2. Pauwelyn KA, Verhamme M. Large hiatal hernia and
iron deficiency anaemia: clinico-endoscopical findings. Acta Clin Belg
2005; 60: 166-172.
3. Panzuto F, Di Giulio E, Capurso G, Baccini F,
D’Ambra G, Delle Fave G, et al. Large hiatal hernia in patients
with iron deficiency anaemia: a prospective study on prevalence and
treatment. Aliment Pharmacol Ther 2004; 19: 663-670.
4. Fireman Z, Zachlka R, Abu Mouch S, Kopelman Y. The
role of endoscopy in the evaluation of iron deficiency anemia in
premenopausal women. Isr Med Assoc J 2006; 8: 88-90.
5. Karande TP, Oak SN, Karmarkar SJ, Kulkarni BK,
Deshmukh SS. Gastric volvulus in childhood. J Postgrad Med 1997; 43:
46-47.
6. Cameron AJ, Higgins JA. Linear gastric erosion. A
lesion associated with large diaphragmatic hernia and chronic blood loss
anemia. Gastroenterology 1986; 91: 338-342.
7. Moskovitz M, Fadden R, Min T, Jansma D, Gavaler J.
Large hiatal hernias, anemia, and linear gastric erosion: studies of
etiology and medical therapy. Am J Gastroenterol 1992; 87: 622-626.
8. Singal AK, Vignesh KG , Mathai
J. Acute gastric volvulus secondary to eventration
of the diaphragm in a child. J Indian Assoc Pediatr Surg 2006; 11: 44-46.
9. Naim HJ, Smith R, Gorecki PJ. Emergent laparoscopic
reduction of acute gastric volvulus with anterior gastropexy. Surg
Laparosc Endosc Percutan Tech 2003; 13: 389-391
10. Casaccia M, Torelli P, Troilo BM, Savelli A, Valente U. Composite
mesh repair of a large paraoesophageal hiatus hernia. J Laparoendosc Adv
Surg Tech A 2006; 16: 381-385.
|
|
|
 |
|

