|
|
|
Indian Pediatr 2020;57:
1181-1182 |
 |
A Unique Case of Cardiac Echinococcus
multilocularis
|
|
Neetu Talwar,* Nikita Agarwal and Krishan Chugh
Division of Pediatric Pulmonology, Fortis Memorial
Research Institute, Sector 44, Gurugram 122 002, Haryana, India.
Email:
[email protected]
|
|
H uman alveolar echinococcosis
(AE) or alveolar hydatid disease is extremely rare in children due to
the prolonged incubation period of 5-15 years [1]. A tumor-like
infiltrative growth characterizes it. Metacestodes of AE can infiltrate
into adjacent areas resulting in its spread to different organs,
primarily liver and lungs [1].
We report the case of a 7-year-old child from Iraq
who presented with the complaints of cough and breathing difficulty,
with progressive worsening over two months before presentation. Parents
had also noticed increasing yellowish discolouration of eyes and skin,
loss of appetite and weight in the previous month. The patient had a
low-grade, intermittent fever for the past 20 days. The child had been
diagnosed to be a case of hepatic failure and had been referred for
liver transplant. On examination, the child had tachycardia, tachypnea
and mild subcostal, intercostal retractions. Breath sounds were absent
on the right side. There was non-tender hepatomegaly, with the liver
span of 16 cm and smooth surface. Minimal ascites was present. Liver
functions were deranged (serum glutamic oxaloacetic transaminase or
SGOT/ serum glutamic pyruvic transaminase or SGPT 145 / 345 U/L, gamma-glutamyl
transferase or GGT 528 U/L, total bilirubin and direct 6.4/2 mg/dL,
total protein 8.1 g/dL, serum albumin 2.8 g/dL). The international
normalized ratio (INR) was 1.37. He also had severe anemia (hemoglobin –
5.8 g/dL), with absolute eosinophil count of 2.45×109/L and high
pro-inflammatory markers. Chest radiograph revealed right-sided pleural
effusion with underlying collapse and consolidation. Pleural tap
revealed almost bile-like pleural fluid with high bilirubin level
suggestive of a trans-diaphragmatic extension of the hepatic disease.
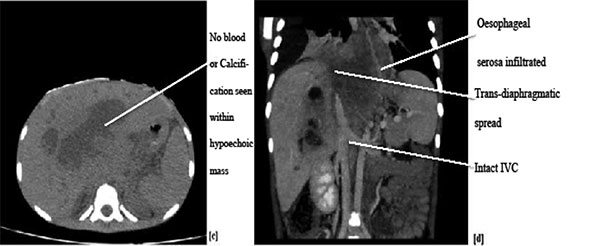
Evaluation of the fluid for infection was negative. Contrast-enhanced,
multiphasic, multi-detector computed tomographic (MDCT) scan of abdomen
revealed hepatomegaly with a large hypodense lesion in the liver,
invading the inferior vena cava and serosa of the oesophagus with cystic
changes, and was reported by the radiologist to possibly be mitotic
etiology of the biliary tract or Echinococcus alveolaris.
Qualitative Echinococcus (E) IgG was positive. Endoscopy revealed normal
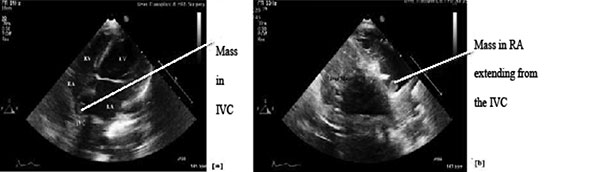
esophageal and gastric mucosa. Echocardiography demonstrated inferior
vena cava infiltration by a mass extending into the right atrium.
Ultrasound-guided liver biopsy revealed an inflammatory pathology with
the possibility of mass forming E. multi-locularis. The child was
treated with 15 mg/kg/day divided in two doses of continuous albendazole
therapy and other supportive treatment, and was under regular follow up.
Unfortunately, the child died 2 months later.
 |
 |
|
Fig. 1 (a) 2-D Echocardiography
(modified 4 chamber view) showing mass in IVC (b) Modified
subcostal view with mass clearly seen in RA (c) CT: Nature of
disease seen here – hypoechoic lesion with no
blood/calcification within, unlikely to be carcinoma (d) Venous
Phase of Triphasic CT: Trans diaphragmatic spread seen into the
adjoining tissue, oesophageal serosa infiltrated. IVC, inferior
vena cava; RA, right atrium; CT, computed tomography.
|
Alveolar echinococcosis, due to E. multilocularis
is extremely unusual, accounting for < 5% of all cases of hydatid liver
disease and, less frequently, lung disease. The mean age of presentation
is 55 years [1,2], with children being rarely affected. Liver is the
primary site of cyst development in almost all patients. The
characteristic feature of E. multilocularis is that they behave
just like malignant tumors with invasion and destruction of surrounding
tissue, spread into contiguous areas and metastasis to distant organs,
with the most common organ being lung [3]. Lung manifestations always
appear after the involvement of the liver [3]. Cardiac echinococcosis is
very rare (0.03%-1% of all cases) [2], with the left ventricle being
most frequently affected (55–60%).
We diagnosed our patient to be a confirmed case of
alveolar echinococcosis based on clinical findings, contrast-enhanced
MDCT, histopathology and serology [4]. We further classified the case as
per the WHO-IWGE (WHO-Informal Working Group on Echinococcosis) PNM
classification as P4N1M1 [5].
The focus of management in these patients is early
diagnosis and radical (tumour-like) surgery, which is followed by
anti-infective prophylaxis with benzimidazoles [1,3,4]. However, as in
our case, most patients are diagnosed at an advanced stage, when radical
surgery (a distance of larval to liver tissue of >2 cm) cannot be
achieved. Hence, as per current recommendations, the cornerstone of
treatment remains the continuous medical treatment with albendazole,
with individualized interventional measures at the appropriate time
[1,4]. Radical surgery could not be done in our patient as R0 (no
residue) resection was not possible. Palliative surgery was not possible
as the lesion was unresectable due to invasion into the oesophagus, as
well as into a blood vessel, leading to its spread to distant organs
(both lungs and heart) [1]. Liver transplant was contraindicated due to
the presence of extra-hepatic locations [1].
The first reported case of cardiac alveolar
echinococcosis in adults, has been recently published [6]. In another
interesting recent case report, E.
granulosus causing
cystic echinococcosis (CE) in left
ventricle has been described in an 8-year-old child [2]. Yet another
publication reports a giant hydatid cyst of the left ventricle in an
11-year-old child, also reviewing the 18 cases of cardiac echinococcosis
reported thus far, all of which were due to cystic echinococcosis (CE)
[7]. This is the first reported case of cardiac AE in children and
highlights the need to consider this rare entity in patients with
extensive liver disease extending into heart and lungs.
REFERENCES
1.
Bulakci M,
Kartal MG, Yýlmaz S, et al. Multimodality imaging in diagnosis
and management of alveolar echinococcosis. Diagn Interv Radiol. 2016;
22:247-56.
2. Su L, Yu J, Dai C, Liu Y, Peng L. Echinococcosis
in left ventricle: a case report. Medicine (Baltimore). 2019;98:e15267.
3. Morar R, Feldman C. Pulmonary echinococcosis. Eur
Respir J. 2003;21:1069-77.
4. Brunetti E, Kern P, Vuitton DA. Writing panel for
the WHO-IWGE. Expert Consensus for the Diagnosis and Treatment of Cystic
and Alveolar Echinococcosis in Humans. Acta Trop. 2010;114:1-16.
5. Kern P, Wen H, Sato N, et al. WHO
classification of alveolar echinococcosis: Principles and application.
Parasitol Int. 2006;55:S283-87.
6. Zhang X, Wei X, Ran L, Tang H. A rare case of
cardiac alveolar echinococcosis. Eur Heart J. 2020;41:2698.
7. Fiengo L, Bucci F, Giannotti D, Patrizi G, Redler A, Kucukaksu DS.
Giant cardiac hydatid cyst in children: Case report and review of the
literature. Clin Med Insights Case Rep. 2014;7:111-16.
|
|
|
 |
|

