|
Childhood fever is one of the
commonest reason for medical consultation in
children, being responsible for 15-25% visits in
primary care, and also presentations to the
emergency departments (ED) [1,2], and is known to
cause significant anxiety in parents [3]. Most
children undergo evaluation for at least one febrile
illness before their third birthday [4]. Western
studies report good parental awareness about fever
[5], but studies from India [6,7] have shown
conflicting results. Frequently, parents do not
document temperature or record it improperly,
leading to undue anxiety and over-crowding of the ED
[6-8]. We studied the correlation of temperatures
measured at home by parents with recordings done at
presentation in the ED among infants with acute
illnesses.
This cross-sectional study was
conducted from April, 2018 to January, 2019 at the
pediatric ED of a public hospital in northern India,
after taking clearance from the Institutional Ethics
Committee. Febrile children aged 3 month to 2 year,
with fever of at least 4 days were considered for
enrollment. A febrile child was defined as one with
history of fever e"38ÚC recorded at least once at
home in previous 24 hours. Those suffering for fever
for >7 days, children with any underlying heart
disease, and children with any diagnosed
immunodeficiency disorder or conditions predisposing
to recurrent infections (like type 1 diabetes,
vesico-ureteric reflux) were excluded. Consecutive
children were enrolled on one pre-decided day every
week.
After taking written informed
consent, enrolled children were evaluated clinically
and initial management provided. Subsequently, based
on history, and clinical and laboratory information,
they were treated as inpatient or outpatient. For
all enrolled children, demographic details, contact
information and details of education and income of
parents were collected. History was taken regarding
highest temperature recorded at home and any
associated symptoms, treatment taken if any before
presentation, relevant history of co-morbidities,
immunization and feeding history. Anthropometric
measurements were taken for all included children as
per standard guidelines, and Z-scores were
calculated using Anthrocalc application.
All the data were recorded in a
structured pre-tested form. Rectal temperature was
taken at presentation for all enrolled children, The
various diagnoses were made and management carried
out according to the departmental protocols guided
by standard management guidelines [9,10]. Mean (SD)
or median (IQR) were calculated for the baseline
characteristics. Pearson correlation coefficient was
calculated for temperature documented at home and in
the ED. Comparisons were done between children with
fever documented in ED, and those without fever
documented in ED.
Out of overall study population
of 150 children with history of fever of 4-7 days in
respective age group attending ED, only 108 (68.3%
boys) had documented fever at home. The median (IQR)
age of the study population was 12 (3-20) months.
The median Z scores for all anthropometric variables
(weight, length and head circumference) were greater
than –3. Majority (88%) of children belonged to the
lower middle (III) and upper lower (IV)
socioeconomic classes, and majority of mothers (62%)
had at least secondary school education (Table
I). Along with fever, the most common
presenting complaint was respiratory problems.
Table I. Baseline Characteristics of the Study Population (N=108)
| Characteristics |
No. (%) |
| Weight, Z-score# |
-2.05 (4.62) |
| Height, Z-score# |
-1.525 (2.57) |
| HC, Z-score# |
-1.66 (1.64) |
|
Immunization statusa |
|
| Partially immunized |
9 (8.3) |
| Fully immunized |
78 (72.2) |
|
Socioeconomic statusb |
|
| Upper middle class |
13 (12) |
| Lower middle class |
51 (47.2) |
| Upper lower class |
42 (38.8) |
| Lower class |
2 (1.9) |
| Maternal education |
|
| Illiterate |
24 (22.2) |
| Primary school |
17 (15.7) |
| Secondary school |
56 (51.9) |
| Graduate |
11 (10.1) |
|
HC: Head circumference; bModified Kuppuswamy
socioeconomic status scale for year 2018.
aImmunization details not known. |
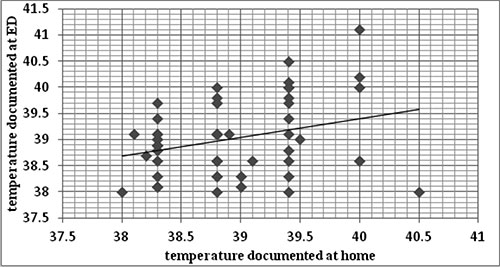
Of the children for whom fever
was documented at home, nearly half (46.3%) did not
have fever at presentation in the ED. Mean (SD)
temperatures documented at home and ED were [38.8
(0.16)°C vs 39 (0.7)°C; P=0.03]. Among
those who were febrile in ED, the correlation
coefficient (r) of fever documented at home
and in ED was 0.3 (95% CI, 0 to 0.6), suggesting a
weak correlation of axillary fever documented by
parents at home and that of rectal temperature
documented in ED (Fig. I).
 |
|
Fig.1 Correlation
between fever documented at home and in ED
(r=0.3).
|
For five children, rectal
temperature could not be documented in view of their
critical condition at presentation to ED, and
axillary temperature was documented in them so as
not to hinder required resuscitative measures. Of
the illiterate mothers, 42% did not document the
fever as compared to 205 of those with a secondary
school education (P=0.02). There was no
increased risk of having a severe infection if
temperature is documented at ED versus if
fever is not documented at presentation [OR (95%
CI): 0.96 (0.32-2.85); P=0.94].
In our study majority of parents
measured temperature at home by axillary or oral
thermometry, There was a weak correlation between
axillary/ oral temperature measured at home and
rectal temperature documented at ED. Findings in our
study are in agreement with the internet-based
survey done by de Bont, et al. [5] in
Netherlands, which showed 71.5% parents document
fever if their child is ill, although majority
documented rectal temperature. None of the parents
in our study documented rectal temperature, as home
measurement of rectal temperature by parents is
uncommon in Indian settings. Other studies from
hospitals in various regions in India report
conflicting results on proportion measuring
temperature of febrile children at home (14.5-71%)
[6,7]. These differences may be based on regional
socio-cultural factors. The finding of association
of temperature documentation at home with higher
educational level of mother is in agreement with
previous reports [8].
The small sample size in our
study may be a limiting factor for applying results
of this study to general population. Most of the
children had already received antipyretics before
presenting to ED, and may have been exposed to
varying environmental temperatures while travelling
to hospital; thus explaining the poor correlation
between temperature documented at home and in ED.
Additional analysis could have been done for
temperature correlations in different disease
groups, but the numbers for individual diseases were
less for valid comparisons. Further studies may need
to study the relationship of domiciliary temperature
measurements and fever at presentation, as triage
and evaluation of pediatric patients in crowded EDs
is frequently dependent on the presence/absence of
fever.
Ethics clearance:
Institutional ethics committee of MAM College; No.
17/IEC/MAMC/2017/Peds/07 dated 10 October, 2017.
Contributors: PP: subject
assessment, management under supervision, data
analysis, and preparing first draft of manuscript;
RB: important contribution in study concept, data
analysis and manuscript preparation; DM: Study
concept, supervision and finalization of manuscript.
All authors approved the final manuscript.
Competing interests: None
stated; Funding: None.
REFERENCES
1. Muth M, Statler J, Gentile DL,
Hagle ME. Frequency of fever in pediatric patients
presenting to the emergency department with
non-illness-related conditions. J Emerg Nurs.
2013;39:389-92.
2. Sands R, Shanmugavadivel D,
Stephenson T, Wood D. Medical problems presenting to
paediatric emergency departments: 10 years on. Emerg
Med J. 2012;29:379-82.
3. Purssell E, Collin J. Fever
phobia: The impact of time and mortality - A
systematic review and meta-analysis. Int J Nurs
Studies. 2016;56:81-9.
4. Finkelstein JA, Christiansen
CL, Platt R. Fever in pediatric primary care:
occurrence, management, and outcomes. Pediatrics.
2000;105:260-6.
5. de Bont EG, Francis NA, Dinant
GJ, Cals JW. Parents’ knowledge, attitudes, and
practice in childhood fever: an internet-based
survey. British J Gen Pract. 2014;64:e10-6.
6. Thota S, Ladiwala N, Sharma
PK, Ganguly E. Fever awareness, management practices
and their correlates among parents of under five
children in urban India. Int J Contemp Pediatr.
2018;5:1368-76.
7. Agrawal RP, Bhatia SS, Kaushik
A, Sharma CM. Perception of fever and management
practices by parents of pediatric patients. Int J
Res Med Sci. 2013;1:397-400.
8. Bertille N, Fournier-Charriere
E, Pons G, Chalumeau M. Managing fever in children:
A national survey of parents’ knowledge and
practices in France. PLoS One. 2013; 8:e83469.
9. Sharma S, Sethi GR, eds.
Standard Treatment Guidelines: A Manual for Medical
Therapeutics. Delhi Society for Promotion of
Rational Use of Drugs & Wolters Kluwer Health, 5th
ed, 2018.
10. Mahajan P, Batra P, Thakur N, et al.
Consensus Guidelines on Evaluation and Management of
the Febrile Child Presenting to the Emergency
Department in India. Indian Pediatr. 2017;54:
652-60.
|

