|
|
|
Indian Pediatr 2020;57:1143-1146 |
 |
Clinical Profile of
SARS-CoV-2 Infected Neonates From a Tertiary Government Hospital
in Mumbai, India
|
|
Pavan Kalamdani, Thaslima Kalathingal, Swati Manerkar and Jayashree
Mondkar
From Department of Neonatology, Lokmanya Tilak Municipal Medical
College and General Hospital, Sion, Mumbai, Maharashtra, India.
Correspondence to: Dr Swati Manerkar, Department of Neonatology,
Lokmanya Tilak Municipal Medical College and General Hospital, Sion,
Mumbai 400 022, Maharashtra, India.
Email:
[email protected]
Received: August 20, 2020;
Initial review: September 05, 2020;
Accepted: September 30, 2020.
Published online: October 12, 2020;
PII: S097475591600251
|
Objectives: To describe the clinical and
laboratory profile of severe acute respiratory syndrome coronavirus 2
(SARS-CoV-2) infected neonates. Methods: This is a review of
hospital records, conducted in a tertiary care public hospital. Medical
records of neonates born from 1 April, 2020 to 31 May, 2020 were
reviewed. Women admitted in labor were screened for SARS-CoV-2 infection
based on the guidelines issued by Indian Council for Medical Research.
Neonates were tested for SARS-CoV-2 infection once mother tested
positive, which was after day 2 of life. Demographic, clinical features,
laboratory tests and chest radiographs of SARS-CoV-2 infected neonates
were reviewed and neonates were telephonically followed up till the age
of 2 months. Results: Out of 1229 mothers, 185 tested positive
(15.05%); 12 neonates (6.48%) tested positive for SARS-CoV-2 infection.
All neonates were exclusively breastfed. Symptoms, if any, were mild and
self-limiting. Serum lactate dehydrogenase and liver enzymes were
elevated. All neonates were healthy and thriving well on follow-up.
Conclusion: SARS-CoV-2 infected neonates are mostly asymptomatic and
thrive well on exclusive breastfeeding.
Keywords: Breastfeeding, COVID -19, Management, Outcome.
|
|
R eports of SARS-CoV-2 infections in
neonates are still emerging. There is little literature
available about the clinical features, outcomes and the mode of
transmission of severe acute respiratory syndrome coronavirus-2
(SARS-CoV-2) infection in neonates, especially from India.
Recently, a meta-analysis has described 58 SARS-CoV-2 positive
neonates from across the globe [1]. We present the clinical and
laboratory profile of SARS-CoV-2 positive neonates admitted to a
tertiary-care public hospital.
METHODS
This was a review of case records of
SARS-CoV-2 positive neonates, conducted in a tertiary care
hospital in Mumbai, India after obtaining approval from
Institutional ethics committee. Medical records of neonates born
between 1 April,
2020 and 31 May, 2020 were reviewed. All neonates who tested
positive for SARS-CoV-2 infection during the birth-admission or
readmitted any-time in the neonatal period were included in the
study.
During this period, Indian Council for
Medical Research (ICMR) recommended that all pregnant women in
labor or who were likely to deliver in the next 5 days, residing
in clusters/containment areas or in large migration gatherings,
from hotspot districts should be tested for SARS-CoV-2 infection
with Real time reverse transcriptase-polymerase chain reaction
(RT-PCR) of nasopharyngeal swab, even if asymptomatic [2].
Mothers readmitted for post-partum complications were also
tested. Neonates were tested for SARS-CoV-2 by RT-PCR on a
nasopharyngeal swab sample if mother tested positive. All babies
showing symptoms suggestive of coronavirus disease (COVID-19)
were also tested. The usual turnover time for the test was 24
hours, which was the same for mother and baby. All the
SARS-CoV-2 positive neonates were retested after 5 days. If
negative on repeat testing, they were discharged. Those who
continued to test positive on day 5 were discharged on day 10,
if asymptomatic, without repeating the test.
Stable neonates, whether positive or
negative, were roomed-in with their SARS-CoV-2 positive mothers
in a separate COVID postnatal ward as recommended by Federation
of Obstetric and Gynaecological Societies of India (FOGSI) and
National Neonatology Forum (NNF) guidelines on the management of
perinatal SARS-CoV-2 infection [3]. Neonates and mothers were
kept on the same bed due to space constraints. Mothers were
encouraged to breastfeed immediately after birth and educated
about maintenance of proper hand and respiratory hygiene.
Lactation counseling and support were provided in person by a
trained counselor. All the neonates were monitored twice daily
for development of any COVID related symptoms like fever,
hypothermia, respiratory distress, lethargy, cough, rhinorrhea,
irritability, rash, diarrhea and feeding intolerance. If the
neonates became symptomatic, they were shifted to the isolation
area and managed.
Data regarding epidemiologic, demographic,
clinical features, laboratory tests and chest radiographs of
COVID positive neonates were recorded. Telephonic follow up of
these neonates was done till 2 months of age. General health
status, need for re-hospitalization, feeding status, weight gain
and immunization were enquired about.
Descriptive statistics were used and outcomes
expressed as proportions. Calculations were done using Microsoft
Excel software.
RESULTS
Out of the total 1229 tested mothers, 185
(15.05%) tested positive for SARS-CoV-2 infection. Three (1.7%)
mothers had fever and two of these three also had mild
breathless-ness and responded favorably to treatment in the
COVID ward (Fig. 1). Twelve neonates
(6.48%) tested positive for SARS-CoV-2 infection; 75% of these
at 48 to 72 hours of life during the birth-admission. Three
neonates were re-admitted with their mothers on day 13, 15 and
20, respectively for maternal complications and tested
subsequently. All these neonates were roomed-in with their
mothers in the COVID postnatal wards. The clinical and
laboratory profile of all the SARS-CoV-2 positive neonates have
been summarized in Table I.
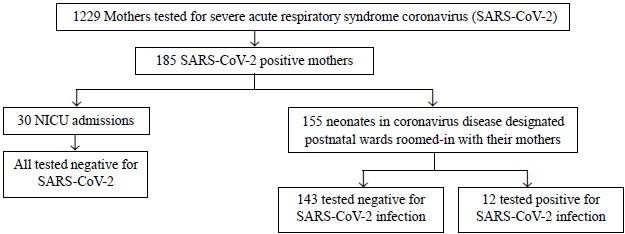 |
|
Fig. 1 Flowchart showing
patients during the study period.
|
Table I Characteristics of SARS-CoV-2 Infected Neonates (N=12)
| Characteristics |
Value |
| Male, n (%) |
8 (66.6) |
| Gestation (wk), median (IQR) |
38 (37.8, 39.3) |
| Birthweight (g)^ |
2734.1 (346) |
| Caesarean section, n (%) |
10 (83.3) |
| APGAR at 1 min, median (IQR) |
8 (8, 8.2) |
| Breastfeeding, n (%) |
12 (100) |
| Feeding difficulty, n (%) |
2 (16.6) |
| Fever, n (%) |
3 (25) |
| Phototherapy, n (%) |
3 (25) |
|
Pre-ductal SpO2 (%), median (IQR) |
98 (97.7, 98) |
| Hospitalization (d), median (IQR) |
13 (12,14) |
|
*Hemoglobin (g/dL) ^ |
14.8 (2.4) |
| *leukocyte count (×109/L) ^ |
10.5 (3.3) |
|
*Absolute neutrophil count (×109/L) ^ |
4.6 (1.4) |
| *Absolute lymphocyte count
(×109/L)^ |
5.02 (1.8) |
| #AST (IU/L), median (IQR) |
75 (65,88) |
| #ALT (IU/L), median (IQR) |
29 (25,39) |
| #CRP (mg/L), median (IQR) |
5 (4.2,7) |
|
#Creatinine (mg/dL), median (IQR) |
0.4 (0.3, 0.6) |
| ‡LDH (IU/L), median (IQR) |
1462 (1148.2, 1604.5) |
|
Values in ^mean (SD) or as detailed; Investigation
carried out in *11, #9 or ‡8 neonates; No baby had
respiratory symptoms or lethargy/neurological symptoms;
AST: Aspartate transaminase, ALT: Alanine transaminase,
CRP: C reactive protein, LDH: Lactate dehydrogenase. |
Telephonic follow up was done for all
positive infants till 2 months of age. Two infants received
their 6-week immunization at 9 weeks, delayed by 3 weeks due to
concerns of safety of visiting a health center during the
pandemic and lockdown. All positive neonates were healthy,
exclusively breastfed at 2 months follow up and did not require
re-hospitalization after discharge following their SARS-CoV-2
infection.
Thirty (16.2%) neonates required NICU
admission for neonatal problems and all of them tested negative
for SARS-CoV-2 infection. The remaining 143 (77.2%) neonates
tested negative and continued to be roomed-in with their
mothers.
DISCUSSION
This is one of the earliest reported cohorts
of COVID positive neonates from India. The exact incidence of
SARS-CoV-2 infection in neonates is largely unknown. The
proportion of SARS-CoV-2 positive neonates in our study was 6.5%
as compared to 3.9% in a meta-analysis of 58 neonates [1].
Although a few authors have reported vertical
trans-mission in neonates, there is still controversy regarding
the same [4]. To prove intra uterine viral infection, testing of
RT-PCR assay on tissue samples derived from placenta, amniotic
fluid, cord blood and neonatal pharyngeal swab in the immediate
post-partum period is required [5]. In our study, the maternal
reports were available after 24 to 48 hours of delivery. Hence
50% neonates were tested at 48 hours, 25% neonates at 72 hours
and the three re-admitted neonates were tested between 13-20
days. The median gestational age was 38 weeks in this study and
the ratio of male to female was 2:1, similar to that described
by Bernardo, et al. [6].
Mode of delivery does not impact transmission
of the infection to the baby [3]. Still, the caesarean section
rates have been found to be higher among SARS-CoV-2 infected
mothers, and in our study too it was 83.3%. Respiratory problems
requiring ventilation have been reported as the most common
presenting symptom amongst SARS-CoV-2 positive neonates [1].
However, none of babies in this cohort had respiratory symptoms.
We found mild and self-limiting symptoms in our cohort, with 3
neonates having fever. However, two out of these three neonates
also had feeding difficulties and excessive weight loss, which
responded to improved feeding practices and supplementary
feeding with expressed breast milk. Hence, these could be cases
of dehydration fever and may not be related to SARS-CoV-2
infection. One neonate had mild fever, which could not be
attributed to any cause, therefore we presumed that the fever
was caused by SARS-CoV-2 infection.
Very few studies have described laboratory
abnormalities in SARS-CoV-2 positive neonates. The study by
Henry, et al. [7] in pediatric COVID patients described
lymphopenia, raised liver enzymes and raised LDH levels as the
common lab abnormalities. Raised LDH levels in adult studies on
SARS CoV-2 infection suggest greater severity of illness [8]. In
our study, marked elevation of LDH levels and mild transaminitis
were observed in the SARS-CoV-2 positive neonates. However, the
significance of raised liver enzymes and LDH in neonates is yet
to be understood. Bernardo, et al. [6] has reported
radiological abnormalities in 44% of SARS-CoV-2 positive
neonates but we did not find any radiological abnormalities in
our study. Current evidence does not recommend any blood or
radiological investigations in any asymptomatic SARS-CoV-2
positive neonates.
The World Health Organization and most
professional bodies recommend rooming-in of asympto-matic
mother-baby dyad, exclusive breastfeeding and maintaining a
distance of 6 feet between them [3,9,10]. All stable neonates in
our study were not only roomed in but also bedded in with their
mothers and exclusively breastfed. Maintaining a distance of 6
feet was not possible due to lack of space in our hospital. In
the study by Salvatore, et al. [11], despite rooming in,
there was no horizontal transmission of SARS-CoV-2 infection as
these babies were kept in Giraffe isolette incubators. Around
6.5% of our neonates had possible horizontal trans-mission due
to prolonged close contact with their SARS-CoV-2 positive
mothers during bedding in.
There is no conclusive evidence that the
virus is transmitted through breastmilk [12,13]. Also, the
benefits of breastfeeding far outweigh the negligible risk of
transmitting the virus. In our center, we counselled and
encouraged mothers to follow strict hand hygiene and respiratory
hygiene all the time, especially while breast-feeding, but the
exact compliance was not studied.
The limitations of our study were its
retrospective design and small number of subjects. The
manifestations in SARS-CoV-2 positive preterm neonates and those
born to severely symptomatic mothers is not known and needs to
be further explored. Exclusive breastfeeding is an integral part
of neonatal care and has to be strongly promoted.
Ethics clearance: Institutional Ethics
Committee Human Research, Lokmanya Tilak Municipal Medical
College and General Hospital; No: IEC/28/20 dated June 11, 2020.
Contributors: PK, TK, SM: conceptualizing
the study, writing the study protocol, collecting data and
preparing the manuscript; JM: critically editing the manuscript.
All authors approved the final manuscript.
Funding: None; Competing interest:
None stated.
|
WHAT THIS STUDY ADDS?
•
The clinical features of
SARS-CoV-2 infection in neonates are mostly
mild/asymptomatic, and such mother-baby dyad can be
successfully roomed-in and breastfed.
|
REFERENCES
1. Dhir SK, Kumar J, Meena J, Kumar P.
Clinical features and outcome of SARS-CoV-2 infection in
neonates: A systematic review. J Trop Pediatr. 2020;0:1-14.
2. Indian Council for Medical Research.
Testing strategy [Internet]. Accessed August 16, 2020. Available
from https://www.icmr.gov.in/cteststrat.html
3. Chawla D, Chirla D, Dalwai S, et al.
Perinatal-Neonatal Management of COVID-19 Infection - Guidelines
of the Federation of Obstetric and Gynaecological Societies of
India (FOGSI), National Neonatology Forum of India (NNF), and
Indian Academy of Pediatrics (IAP). Indian Pediatr.
2020;57:536-48.
4. Kotlyar A, Grechukhina O, Chen A, et al.
Vertical transmission of COVID-19: A systematic review and
meta-analysis. Am J Obstet Gynecol. 2020, Jul 31. [Epub ahead of
print]
5. Wang C, Zhou YH, Yang HX, Poon LC.
Intrauterine vertical transmission of SARS-CoV-2: What we know
so far. Ultrasound Obstet Gynecol. 2020;55:724-25.
6. De Bernardo G, Giordano M, Zollo G, et
al. The clinical course of SARS-CoV-2 positive neonates. J
Perinatol. 2020, Jul 6. [Epub ahead of print]
7. Henry B, Benoit S, de Oliveira MH, et
al. Laboratory abnormalities in children with mild and
severe coronavirus disease 2019 (COVID-19): A pooled analysis
and review. Clin Biochem. 2020;81:1-8.
8. Henry B, Aggarwal G, Wong J, et al.
Lactate dehydro-genase levels predict coronavirus disease 2019 (CoVid
-19) severity and mortality: A pooled analysis. Am J Emerg Med.
2020;38:1722-26.
9. WHO. Breastfeeding advice during COVID-19
outbreak [Internet]. Accessed August 16, 2020. Available from
http://www.emro.who.int/nutrition/nutrition-infocus/breastfeeding-
advice-during-CoVid-19-outbreak.html
10. UNICEF. Breastfeeding during the CoVid-19
pandemic [Internet]. Accessed August 16, 2020. Available from
https://www.unicef.org/eap/breastfeeding-during-CoVid-19
11. Salvatore CM, Han JY, Acker KP, et al.
Neonatal management and outcomes during the COVID-19 pan-demic:
An observation cohort study. Lancet Child Adolesc Health. 2020
Jul 23. [Epub ahead of print].
12. Wang S, Guo L, Chen L, et al. A
case report of neonatal 2019 coronavirus disease in China. Clin
Infect Dis. 2020;71:853-57.
13. Chen Y, Peng H, Wang L, et al.
Infants born to mothers with a new coronavirus (COVID-19). Front
Pediatr. 2020; 8:1-5.
|
|
|
 |
|

