|
|
|
Indian Pediatr 2020;57: 1114-1118 |
 |
Effect of Green Banana (Musa paradisiaca)
on Recovery in Children With Acute Watery Diarrhea With No
Dehydration : A Randomized Controlled Trial
|
Dhandapany Gunasekaran, Anandhi Chandramohan, Kadirvel
Karthikeyan, Banupriya Balasubramaniam, Podhini Jagadeesan
and Palanisamy Soundararajan
From Department of Pediatrics, Mahatma Gandhi Medical
College and Research Institute, Puducherry, India.
Correspondence to: Dr Dhandapany Gunasekaran, Professor,
Department of Pediatrics, JIPMER, Puducherry, India.
Email:
[email protected]
Received: March 30, 2020;
Initial review: May 06, 2020;
Accepted: July 07, 2020.
Trial registration: CTRI/2017/05/008623
Published online: September 07, 2020;
PII:S097475591600244
|
Background: Cooked green banana (Musa
paradisiaca) has been observed to be useful in reducing
the duration of diarrheal illness in children.
Objective: To evaluate whether
supplementation of cooked green banana shortens the duration
of diarrhea in children with acute watery diarrhea with no
dehydration.
Study design: Open label randomized
controlled trial.
Participants: Consecutive children
aged 9 months to 5 years who presented with acute watery
diarrhea within 48 hours of onset of illness with no
dehydration.
Intervention: Children in the control
group received standard care, while those in the
intervention group received cooked green banana in addition
to standard care under supervision in the hospital for 72
hours, and then continued at home until diarrhea stopped or
14th day of illness, whichever is earlier.
Outcome measures: Proportion of
children who improved at 72 hours of intervention (passing
formed stools with normal frequency) was considered as the
primary outcome and the incidence of complications such as
dehydration, persistent diarrhea and secondary lactose
intolerance were evaluated as the secondary outcomes.
Results: The proportion of children
who recovered within 72 hours was significantly higher
(62.4%) in the green banana group compared to the control
group (47.2%) [RR 1.3 (95% CI 1.05-1.7), NNT=7].The number
of children with complications such as dehydration and
persistent diarrhea was also signi-ficantly less in the
intervention group.
Conclusion: Supplementation of cooked
green banana in the diet of children with acute watery
diarrhea with no dehydration hastens their recovery.
Key words: Duration, Management, Outcomes.
|
D iarrhea is an
important determinant of childhood mortality and also
predisposes the child to under-nutrition [1,2]. Supportive
measures such as adequate hydration (by frequent breast
feeding, home available fluids and oral rehydration
solution) and oral zinc therapy are the mainstay of
management as per World Health Organization (WHO) [3].
Cooked green banana (Musa
paradisiaca) is shown to have a beneficial effect in
lessening the duration of diarrhea and dysentery [4,5]. The
short chain fatty acids released from the resistant starch,
a major constituent of green banana, has been demonstrated
to increase the absorption of water and electrolytes from
the large intestine and prevent complications such as
dehydration [6]. Literature on green banana in diarrheal
illness is sparse and is limited to resource-constrained
countries like Bangladesh. Given the paucity of data from
India, our objective was to evaluate whether supplementation
of cooked green banana shortened the duration of diarrhea in
children with acute watery diarrhea with no dehydration.
METHODS
This open label randomized controlled
trial was conducted from June, 2017 to June, 2018, in the
department of pediatrics of a tertiary care teaching
hospital in India. Children aged 9 months to 5 years,
presenting within 48 hours of onset of acute watery diarrhea
(AWD) with no dehydration (based on WHO criteria) [3] and
whose parents were willing to admit their children in the
hospital for three days were considered for the study. It
was ensured that the parents did not have any financial
burden due to the hospital stay. From among these, children
who could not be fed orally, who were under-nourished
(weight for age Z score <-2) [7], those having any
concurrent or pre-existing severe illness, and those who had
received any antibiotic or anti-motility agents in the last
seven days were excluded. Children with blood in stool were
also excluded. After getting written informed consent from
the parents, one of the investigators randomized the
eligible children into two groups based on block
randomization with variable block size using
computer-generated randomization sequence. Allocation
concealment was done using sequentially numbered, opaque,
and sealed envelopes. All the investigators enrolled and
assigned the participants to interventions. Blinding could
not be done in view of the logistics involved. Assuming the
proportion of children with formed stools at 72 hours
(primary outcome) to be 60% in the control arm [4] and 80%
in the intervention arm (absolute difference of 20%), the
sample size estimated with a power of 90% and alpha error of
5% was 105 in each group. Considering a dropout rate of 20%,
it was decided to recruit 125 children in each group.
Children in the Control group, received
standard care for acute diarrhea (zinc sulphate 20 mg orally
once daily for 14 days, plus frequent breast milk, if on
breast feeding, plenty of home available fluids, such as
rice kanji, butter milk or tender coconut water, ORS
10 mL/kg/loose stool, and regular diet). Children in Green
banana supplemented diet (GB) group received standard care,
as above, and cooked green banana, in addition. The raw
green banana was boiled for ten minutes following which the
skin was peeled and the pulp was mashed to semi-solid
consis-tency using a spoon. The cooked green banana was
offered either alone (with little salt for taste) or mixed
with any other food of their choice; the dose of green
banana was 50 g twice daily for children younger than 1
year, 100 g twice daily for those aged 1-3 years, and 100g
thrice daily for those aged 3-5 years [4]. The green banana
supplemented diet was continued until diarrhea stopped or
till the 14th day of illness, whichever was earlier.
Children who developed dehydration were managed as per WHO
protocol [3]; other complications were treated uniformly as
per the institutional protocol. Children who persisted to
have diarrhea beyond 72 hours from the beginning of
intervention were advised to continue the standard treatment
at home. The parents of the GB group were also advised to
give cooked green banana daily until cessation of diarrhea –
the cooking method was explained to the parents prior to
discharge. Compliance for home available fluids, ORS and
zinc for both the groups and in addition cooked green banana
for the intervention group was ensured by daily telephonic
contact until the 14th day of illness and the details were
collected. The parents were asked to bring the child for
review if there were any concerns on telephonic discussion.
Children with diarrhea persisting for more than 14 days were
also reviewed again in the hospital.
The primary outcome assessed was the
proportion of children who improved at 72 hours of
intervention (passing formed stools with the usual
frequency), as observed by the mother and verified by one of
the investigators. The incidence of dehydration, persistent
diarrhea (diarrhea persisting beyond 14 days), lactose
intolerance (as evidenced by perianal excoriation and
positive stool reducing substances test) and any other
complications were evaluated as the secondary outcomes. The
study was approved by the Institutional ethics committee,
and the trial was prospectively registered in Clinical
Trials Registry of India.
Statistical analyses: Data collection
was done with the help of a semi-structured pretested
proforma and was transcribed into Microsoft Excel spread
sheet. Data analysis was done using the software STATA
version 12. The baseline socio-demographic variables were
com-pared between groups using chisquare test. An intention
to treat analysis was performed. The proportion of children
recovering within 72 hours, and the development of
complications in both the groups were compared using the
chisquare test. In addition, time to event analysis was
carried out for recovery using Kaplan Meier survival graphs
and the recovery time between the groups was compared using
log rank test. All statistical testing was carried out at 5%
level of significance.
RESULTS
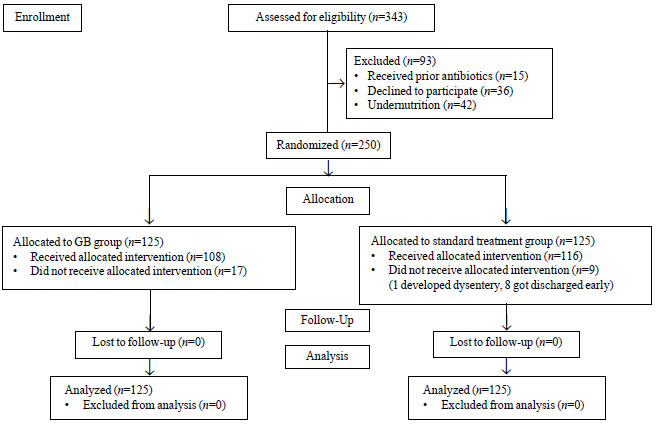
Of the 250 children recruited, 108
children in the green banana group and 116 children in the
control group completed the study (Fig. 1).
There was no significant difference between the groups with
respect to the base-line demographic characteristics,
socioeconomic status, duration of the illness (between the
onset of illness and reporting for treatment), fever,
vomiting and the pre-valence of breastfeeding (Table
I). Children in the intervention group received GB diet
for a median (IQR) duration of 3 (2) days (range, 2-14 day
of illness). depending on the duration of diarrhea. The
proportion of children recovering within 72 hours was
significantly higher (62.4%) in the GB group as compared to
the Control group (47.2%) [RR (95% CI) 1.3 (1.05-1.7),
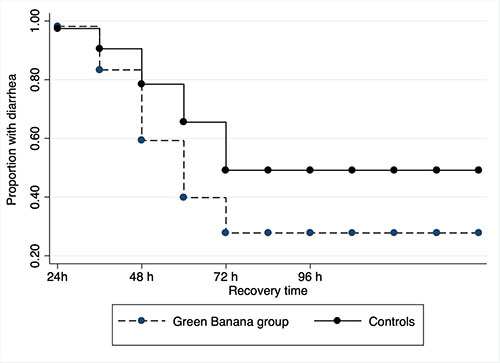
NNT=7; P=0.002] (Table II). Moreover,
on comparing the time to recovery using Kaplan Meier graph,
the pro-portion of children with diarrhea at 72 hours was
significantly less in the green banana group (Fig.
2).
 |
|
Fig. 1 Consort flow
diagram depicting study methodology.
|
Table I Baseline Characteristics of Children With Acute Diarrhea Enrolled in the Study (N=250)
| Characteristics
|
Green banana |
Control group
|
|
group (n=125) |
(n=125) |
| Age, mo |
23 (13.7) |
22.8 (13) |
| Weight for Age |
|
|
| -2 to -1 Z |
72 (57.6) |
67 (53.6) |
| 1 to 0 Z |
44 (35.2) |
52 (41.6) |
| >0 Z |
9 (7.2) |
6 (4.8) |
| Current breastfed |
|
|
| 09-12 mo of age |
25 (20) |
20 (16) |
| 13-24 mo of age |
13 (10.4) |
16 (12.8) |
| 25-36 mo of age |
1 (0.8) |
0 |
| Duration of illness* |
|
|
| 0-12 h |
13 (10.4) |
16 (12.8) |
| 13-24 h |
42 (33.6) |
38 (30.4) |
| 25-36 h |
37 (29.6) |
42 (33.6) |
| 37-48 h |
33 (26.4) |
29 (23.2) |
| Fever* |
46 (36.8) |
42 (33.6) |
| Vomiting (1-3 times/d)* |
32 (25.6) |
37 (29.6) |
| *at presentation;
All values in no. (%) except age in mean (SD);
P>0.05 for all comparisons. |
GB: green banana.
|
|
Fig. 2 Kaplan Meier graph
showing recovery time in the two groups.
|
During the three days of stay in the
hospital, none of the children in the two groups developed
severe dehydration. Significantly higher number of children
in the control group developed some dehydration (P=0.006)
and persistent diarrhea (P=0.01) (Table II).
None of the children in either group developed any other
complications, including acute kidney injury.
Table II Recovery From Acute Diarrhea and Complications in the Study Population (N=250)
| Parameter |
Green banana |
Control group |
Risk ratio |
P value |
|
group (n=125) |
(n=125) |
(95% CI) |
|
| Recovery within 72 h |
78 (62.4) |
59 (47.2) |
1.3 (1.05-1.7) |
0.02 |
| Dehydration within 72 h |
2 (1.6) |
13 (10.4) |
0.15 (0.03-0.7) |
0.006 |
|
Persistent diarrhea
|
4 (3.2) |
15 (12) |
0.3 (0.1-0.8) |
0.01 |
| Secondary lactose intolerance
|
1 (0.8) |
5 (4) |
0.2 (0.02-1.7) |
0.2 |
| Values in no. (%). |
None of the children had any side effects
to the cooked green banana (excessive vomiting or abdominal
pain). Fifteen children (12%) in the green banana group
refused to eat the specified amount of green banana despite
trying multiple times. The green bananas were purchased
daily from the local market and the approximate cost was
three rupees (INR) per child per day.
DISCUSSION
This open label randomized control trial
documented faster recovery following supplementation of
green banana in the diet of under-five children with acute
watery diarrhea with no dehydration. Our findings are in
agreement with the pioneering work from Bangladesh [4],
documenting recovery both on day 3 and day 7 after
supplementation with green banana among 2968 children with
acute diarrhea in a cluster randomized field trial. The
serial assessment over 72 hours of all the recruited
children in the hospital by physicians is one of the
strength of the current study. The present study also
demonstrates the lesser number of children developing
dehydration in the intervention group highlighting stool
volume reduction, as also shown previously [5]. Moore, et
al. [8] noted a six-fold higher incidence of persistent
diarrhea in children with diarrhea lasting for more than
seven days. We noticed only 30% children receiving
intervention to develop persistent diarrhea. Hence, early
initiation of green banana supplemented diet, as in our
study, may limit the number of diarrhea days and may lower
the progression to persistent diarrhea.
The exact mechanism of action of green
banana in acute watery diarrhea remains elusive. The widely
recognized hypothesis involves the role of resistant starch
in diarrhea. Resistant starch, constituting 83.7% of green
banana [9], is refractory to enzyme hydrolysis in the small
intestine, and passes unaltered to the colon where it is
acted upon by the normal commensals to produce short chain
fatty acids (SCFA), which are the primary mediators of the
beneficial activity [10]. The cytoprotective properties of
SCFAs play an active role in the maintenance of the tight
junction integrity through increased claudin expression
[11], regeneration of infected epithelium by stimulation of
the mucosal transglu-taminase activity [12] and positive
jejunotrophic effects through autonomic nervous system [13].
All these mechanisms assist in the absorption of sodium and
water. Moreover, an exclusive Butyrate-HCO 3-
transporter mechanism in absorption of
sodium and water is also demonstrated [14]. Also, by
promoting the growth of the commensals [10] and by producing
antimicrobial peptides at the epithelium [15], SCFAs also
exert non-specific antimicrobial activity. This has been
demonstrated by in vitro studies [16] and in animal
studies [17].
Our study has few limitations. The cooked
green banana was mixed with salt for better palatability.
This could have altered the electrolyte intake and might
have had a potential effect on the outcome as well. As
post-discharge compliance was assessed by daily telephonic
conversations, objective measurement was not possible during
that period. Despite mothers’ efforts, acceptability of
green banana was a major problem (12%) in our study.
Introduction of green banana as a complementary food in
infancy, addition of flavors of infant’s choice to the green
banana diet [18], or use of palatable preparations of green
banana such as papads are suggested [19].
Although oral rehydration solution is the
mainstay of treatment in children with acute watery diarrhea,
we feel that green banana diet with its above-mentioned
proper-ties has a promising role, especially in developing
countries. In conclusion, this open label randomized
controlled trial highlights the role of cooked green banana
supplemented diet as a useful adjunct to standard treatment
(ORS, home available fluids and zinc) in the management of
acute watery diarrhea with no dehydration.
Ethical clearance: Institutional
ethics committee of MGMCRI, Puducherry;
ECR/451/Inst/PO/2013/RR-16 dated 08/06/2016.
Contributors: DG, AC: conceptualized,
designed the study and finalized the manuscript; KK, BB, PJ,
PS: collected, compiled the data and helped in analyzing and
drafting the manuscript. All have approved the final draft.
Funding: None; Competing interests:
None stated.
|
What is Already Known?
• Addition of cooked green banana
in the diet is beneficial in diarrheal illness.
What This Study Adds?
• Cooked green banana diet in addition to
standard treatment reduces the duration of illness
and lessens the chances of complications in
under-five children with acute watery diarrhea
without dehydration.
|
REFERENCES
1. Key facts on Diarrhoeal disease.
Available from:
https://www.who.int/en/news-room/fact-sheets/detail/diarrhoeal-disease.
Accessed June 11, 2020.
2. GBD 2016 Diarrheal Disease
Collaborators. Estimates of the global, regional, and
national morbidity, mortality, and aetiologies of diarrhea
in 195 countries: A systematic analysis for the global
burden of disease study 2016. Lancet Infect Dis.
2018;18:1211-28.
3. World Health Organization. The
treatment of Diarrhea: A manual for Physicians and Other
Senior Health Workers, 4th rev. Available from:
https://apps.who.int/iris/handle/10665/43209. Accessed
June 11, 2020.
4. Rabbani GH, Larson CP, Islam R, Saha
UR, Kabir A. Green banana-supplemented diet in the home
management of acute and prolonged diarrhoea in children: A
community-based trial in rural Bangladesh. Trop Med Int
Health. 2010;15:1132-9.
5. Rabbani GH, Teka T, Zaman B. Majid N,
Khatun M, Fuchs GJ. Clinical studies in persistent diarrhea:
Dietary manage-ment with green banana or pectin in
Bangladeshi children. Gastroenterology. 2001;121:554-60.
6. Rabbani GH, Teka T, Kumar Saha S,
et al. Green banana and Pectin improve small intestinal
permeability and reduce fluid loss in Bangladeshi children
with persistent diarrhea. Dig Dis Sci.2004;49:475-84.
7. World Health Organization. Training
Course on Child Growth Assessment. Geneva, WHO, 2008.
Available from: https://www.who.int/childgrowth/
training/ module_h_ directors_guide.pdf. Accessed June
11, 2020.
8. Moore SR, Lima NL, Soares AM, et
al. Prolonged episodes of acute diarrhea reduce growth
and increase risk of persistent diarrhea in
children. Gastroenterology. 2010;139:1156-64.
9. Faisant N, Gallant DJ, Bouchet B,
Champ M. Banana starch breakdown in the human small
intestine studied by electron microscopy. Eur J Clin Nutr.
1995;49:98-104.
10. Topping DL. Short chain fatty acids
produced by intestinal bacteria. Asia Pac J Clin Nutr.
1996;5:15-19.
11. Yan H, Ajuwon KM. Butyrate modifies
intestinal barrier function in IPEC-J2 cells through a
selective upregulation of tight junction proteins and
activation of the Akt signaling pathway. PLoS One.
2017;12:e0179586.
12. D’Argenio G, Cosenza V, Sorrentini I,
et al. Butyrate, mesalamine, and factor XIII in
experimental colitis in the rat: Effects on transglutaminase
activity. Gastroenterology. 1994;106:399-404.
13. Frankel WL, Zhang W, Singh A,
Klurfeld DM, Don S, Sakata T, et al. Mediation of
trophic effects of short-chain fatty acids on the rat
jejunum and colon. Gastroenterology. 1994;106:375-80.
14. Sandle GI. Salt and water absorption
in the human colon: a modern appraisal. Gut. 1998;43:294-9.
15. Parada Venegas D, De la Fuente MK,
Landskron G, et al. Short chain fatty Acids
(SCFAs)-mediated gut epithelial and immune regula-tion and
its relevance for inflammatory bowel diseases. Front Immunol.
2019;10:277.
16. Fagbemi JF, Ugoji E, Adenipekun T,
Adelowaotan O. Evaluation of the antimicrobial properties of
unripe banana (Musa sapientum L), lemon grass (Cympobogan
citrates S.) and turmeric (Curcuma longa L.) on
pathogens. Afr J Biotechnol. 2009;8:1176-82.
17. Rabbani GH, Albert MJ, Hamidur Rahman
AS, Moyenul Isalm M, Nasirul Islam KM, Alam K. Short-chain
fatty acids improve clinical, pathologic, and microbiologic
features of experimental shigellosis. J Infect.
1999;179:390-7.
18. Mura Paroche M, Caton SJ, Vereijken
MJLC, Weenen H, Houston-Price C. How infants and young
children learn about food: A systematic review. Front
Psychol. 2017;8: 1046.
19. Bhatawale SP, Mohammad UIA, Mirza RSS, Mohammed Zafar
IM, Siddiqui AN, Fatema M. Effect of unripe banana flour
incorporation on resistance starch content of rice papad. J
Nutr Food Sci. 2012;2:143.
|
|
|
 |
|

