|
|
|
Indian Pediatr 2021;58:726-728 |
 |
Clinical Profile of
Adolescent Onset Anorexia Nervosa at a Tertiary Care Center
|
|
Kavitha Esther Prasad, 1
Roshni Julia Rajan,1 Mona M
Basker,1 Priya Mary Mammen2,
YS Reshmi1
From 1Division of Adolescent Medicine, Department of Pediatrics, and
2Department of Child and Adolescent Psychiatry, Christian Medical
College and Hospital, Vellore, Tamil Nadu.
Correspondence to: Dr Roshni Julia Rajan, Child Health III Unit,
Christian Medical College and Hospital, Vellore, Tamil Nadu.
Email: [email protected]
Received: March 25, 2020;
Initial review: April 11, 2020;
Accepted: September 22, 2020.
Published online: January 02, 2021;
PII: S097475591600267
|
Objectives: To study the
clinical profile and outcome of adolescent onset anorexia nervosa at a
tertiary care center in Southern India. Method: Review of
hospital records of adolescents diagnosed with anorexia nervosa. Outcome
was assessed for those with a follow-up of atleast one year, by
outpatient visit or by a telephonic interview. Findings: Data of
43 patients (28% males) with mean (SD) age at presentation of 13.4 (1.7)
years were included. The mean (SD) BMI at presentation was 13.8 (3.2)
kg/m2, the lowest being 8.3 kg/m2. 33 (76%) patients were hospitalized
for nutritional rehabilitation. Of the 15 patients followed up 1-5 years
later, one had died and 11 had achieved normal weight for age.
Conclusion: As compared to other studies, this study showed a higher
proportion of boys with anorexia nervosa. Further research is necessary
to understand factors affecting long-term outcome.
Keywords: Eating disorder, Management, Outcome.
|
|
A
norexia nervosa is an
eating disorder
characterized primarily by an altered
perception of body image, resulting in
significant weight loss and is influenced by bio-psychosocial
factors. In India, anorexia nervosa is increasingly recognized
as a cause of morbidity and mortality among adolescents. The
reported lifetime prevalence of anorexia nervosa is 0.5-2%, with
a peak age of onset around 13-18 years [1]. Literature reveals a
changing epidemiology of this disorder, with increasing rates of
eating disorder being diagnosed in younger children and in males
[2-5]. Though the prevalence of eating disorders is higher in
Western countries, there is an increasing trend of case reports
from India [5]. With increasing incidence of anorexia nervosa in
children, pediatricians become the first point of contact for
many cases.
Our study aims to describe the clinical
profile of adolescents admitted with anorexia nervosa in a
tertiary care center in Southern India.
METHODS
This was a hospital record review of
adolescents hospitalized with anorexia nervosa and their follow
up after atleast one year of discharge. We reviewed the data of
adolescents (aged 10 to 18 years) who were admitted either in
the adolescent medicine facility or the child and adolescent
psychiatry unit between May, 2006, and December, 2019, and
details of patients with a diagnosis of eating disorder or
anorexia nervosa were extracted. Adolescents who fulfilled the
DSM-V criteria for anorexia nervosa or other specified eating
and feeding disorders (OSFED) were included in this study. Those
with diagnoses of bulimia nervosa, psychogenic vomiting or
unspecified feeding disorders were excluded.
Data regarding the clinical profile and
hospitalization was collected from the hospital database. Follow
up of these patients was done after atleast one year of hospital
discharge following initial hospitalization, either by an
outpatient visit or a telephonic interview. Information
regarding clinical symptoms, weight gain, and school performance
was collected.
Data entry and analysis was done using
Epidata software.
RESULTS
Over the 13 year 8 month period, 43
adolescents of whom 12 (27.9%) were males, were studied.
Anorexia nervosa restricting type was the diagnosis in 23
(53.4%) adolescents, and 9 (20.9%) had binge-purge type. Other
specified feeding and eating disorders (OSFED) were diagnosed in
11 (25.5%).
The mean (SD) age at presentation was 13.4
(1.7) years and the mean (SD) age at onset was 12.4(1.8) years.
The youngest patient was 10 years old. 21 (48.8%) adolescents
had a BMI below the 3rd centile, with one patient having a BMI
of 8.3 Kg/m 2. Loss
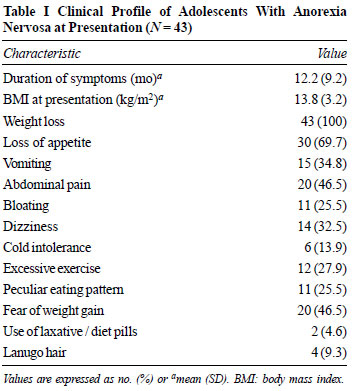
of appetite and abdominal pain were the two most common
presenting symptoms seen in 30 (69.7%) and 20 (46.5%) patients,
respectively (Table I). The mean (SD) calorie intake at
presentation was 388 (247) calories per day. The most common
triggers were peer pressure seen in 15 (34%) patients and family
history of overt eating disorders or a significant adult who was
reportedly health conscious in 8 (18.6%) patients. Men-strual
irregularities were present in 19 (61.2%) adolescent girls, of
whom 5 (26.3%) had primary amenorrhea and 10 (52.6%) had
secondary amenorrhea. Co-morbid conditions such as obsessive
compulsive disorder or depression were present in 11 (25.5%)
patients. There was a family history of psychiatric illness in 9
(20.9%) patients.
 |
| |
Microcardia was present in 21 (48.8%)
adolescents. The ECG changes seen in 6 (13.9%) adolescents
included sinus bradycardia, QT prolongation and T wave changes.
Echocardiography was done in five adolescents and was normal.
Seven adolescents had MRI of the brain and abnormal findings
were present in 5 (71.4%) of them. The abnormal findings
included cerebral atrophy, white matter volume loss,
periventricular hyperintensities and pituitary changes. Bone
mineral density was done in 4 patients, 2 (50%) of whom had low
mineral density.
Of the 43 adolescents, 33 (76.7%) were
admitted for nutritional rehabilitation [mean (SD) stay, 13.7
(5.5) days]; the remaining 10 did not require hospitalization
for medical treatment. Of the 33 admitted, 15 required initial
feeding via nasogastric tube, while 1 patient required
nasogastric feeds even at discharge. Hemodynamic instability was
present in 12 (36.3%) of these patients, and refeeding syndrome
was diagnosed in 10 (30.3%) of these patients. At discharge, the
average daily calorie intake was 1935 calories and the average
weekly weight gain was 1.1 kg.
Of the 43 patients, 10 (23.2%) were yet to
complete a 1-year follow-up period, and 18 (41.8%) were lost to
follow-up. One child died 18 months later with severe
hemo-dynamic instability, and complications of electrolyte
imbalance, coagulopathy and shock. Of the remaining 14 (32.5%)
patients, 2 (14.2%) persisted to have symptoms, 1 (7.1%) patient
had become overweight, and the remaining 11 (78.5%) had normal
weight for age.
DISCUSSION
The proportion of males in the study was
higher than that reported in other studies (9-15%) in
adolescents [4,6]. Possible reasons include improved awareness
and diagnoses, and the ease of families to attend an adolescent
medicine clinic, thereby avoiding the stigma of referral to
psychiatry. The age of presentation and onset was similar to
data from Western studies [6,7], while the age of onset was
lower than that reported in Asian studies [8,9]. The average BMI
at presentation was similar to other studies [8,10]. Some
adolescents who were overweight or obese prior to onset of
symptoms, had a significant weight loss over a short period of
time and their BMI at presentation was normal; the adolescents
in this group were either the binge-purge type or the OSFED
category.
Adolescents in the younger age group had a
higher percentage of the binge-purge type of anorexia nervosa,
while those in the older age group were of restrictive type.
This finding is slightly different from previous studies, which
show the younger age group to be more of the restrictive type
[9]. The most common identified trigger factors were peer
pressure and family influence, similar to data from other
studies [9-11].
Mortality rates reported in adolescents
[7,12,13] are lower compared to adults with anorexia [9,14,15].
Our small cohort size precludes comment on mortality, but
further studies are required to better estimate mortality and
outcome. The poor follow-up in our patients reflects the
inability of the family to understand the severity of disease,
stigma of a psychiatric illness and financial burden of
treatment on the family.
Our data will assist pediatricians in
identifying anorexia nervosa early, and lead to appropriate
diagnosis and management to improve overall outcome.
Ethics clearance: Ethics Committee,
Institutional Review Board, CMC, Vellore; No. 11511, dated
September 3, 2018.
Contributors: MMB: concept and the
study design was done; KEP, RJR, RYS, MMB: material preparation,
data collection and analysis were performed; RJR, KEP: written
first draft of the manuscript; MB, PM: revision of the
manuscript; MB: final approval of the manuscript. All authors
have read and approved the manuscript.
Funding: None; Competing interests:
None stated.
|
WHAT THIS STUDY ADDS?
• Profile of adolescents with anorexia nervosa at a
tertiary center is described.
|
REFERENCES
1. Weaver L, Liebman R. Assessment of
anorexia nervosa in children and adolescents. Curr
Psychiatry Rep. 2011;13: 93-8.
2. Smink FR, van Hoeken D, Hoek HW.
Epidemiology of eating disorders: Incidence, prevalence and
mortality rates. Curr Psychiatry Rep. 2012;14:406-14.
3. Limbers CA, Cohen LA, Gray BA. Eating
disorders in adolescent and young adult males: Prevalence,
diagnosis, and treatment strategies. Adolesc Health Med Ther.
2018; 9:111-16.
4. Pinhas L, Morris A, Crosby RD, Katzman
DK. Incidence and age-specific presentation of restrictive
eating disorders in children: A Canadian paediatric
surveillance program study. Arch Pediatr Adolesc Med.
2011;165:895-99.
5. Basker MM, Mathai S, Korula S, Mammen
PM. Eating disorders among adolescents in a tertiary care
center in India. Indian J Pediatr. 2013;80:211-14.
6. Petkova H, Simic M, Nicholls D, et al.
Incidence of anorexia nervosa in young people in the UK and
Ireland: A national surveillance study. BMJ Open.
2019;9:e027339.
7. Wentz E, Gillberg I, Anckarsäter H,
Gillberg C, Råstam M. Adolescent-onset anorexia nervosa:
18-year outcome. Br J Psychiatry. 2009;194:168-74.
8. Kuek A, Utpala R, Lee HY. The clinical
profile of patients with anorexia nervosa in Singapore: A
follow-up descriptive study. Singapore Med J.
2015;56:324-28.
9. Lee HY, Lee EL, Pathy P, Chan YH.
Anorexia nervosa in Singapore: An eight-year retrospective
study. Singapore Med J. 2005;46:275-81.
10. Tanaka H, Kiriike N, Nagata T, Riku
K. Outcome of severe anorexia nervosa patients receiving
inpatient treatment in Japan: An 8-year follow-up study.
Psychiatry Clin Neurosci. 2001;55:389-96.
11. Hilbert A, Pike KM, Goldschmidt AB,
et al. Risk factors across the eating disorders. Psychiatry
Res. 2014;220:500-6.
12. Herpertz-Dahlmann B, Müller B,
Herpertz S, Heussen N, Hebebrand J, Remschmidt H.
Prospective 10-year follow-up in adolescent anorexia nervosa
– course, outcome, psychiatric comorbidity, and psychosocial
adaptation. J Child Psychol Psychiatry. 2001;42:603-12.
13. Katzman DK. Medical complications in
adolescents with anorexia nervosa: A review of the
literature. Int J Eat Disord. 2005;37:S52-9.
14. Kameoka N, Iga J, Tamaru M, et al.
Risk factors for refeeding hypophosphatemia in Japanese
inpatients with anorexia nervosa. Int J Eat Disord.
2016;49:402-06.
15. Fichter MM, Quadflieg N, Hedlund S. Twelve-year course
and outcome predictors of anorexia nervosa. Int J Eat Disord.
2006;39:87-100.
|
|
|
 |
|

