|
|
|
Indian Pediatr 2020;57:
760-761 |
 |
Plastic Bronchitis: A Manifestation of Dander
Hypersensitivity
|
|
Ritika Chhawchharia1, Neeraj Gupta1*,
Dhiren Gupta1 and Poojan Agarwal2
Departments of 1Pediatric Pulmonology and
Allergy, 2Pathology, Sir Ganga Ram Hospital, New Delhi,
India.
Email: [email protected]
|
|
Plastic bronchitis, an entity with grave prognosis, is characterized by
formation of large, branching bronchial casts obstructing the
tracheobronchial tree. It has been previously reported in children with
cyanotic congenital heart disease (CHD), asthma, allergic broncho-pulmonary
aspergillosis (ABPA) and cystic fibrosis. A 9-month old boy presented
with severe respiratory distress which required invasive ventilation for
type-2 respiratory failure. He had received inhaled bronchodilators
twice for recurrent cough in last 3 months. His grandfather had asthma
and required inhaled medications. The child had exposure to animal
dander (buffalo and cow) and wheat dust from nearby farm since birth. At
admission, child had end-expiratory wheeze in left axillary area. High
requirement of lung inflation pressures and loss of alpha-angle on
end-tidal carbon dioxide graphic suggested obstructive airway.
Salbutamol and ipratropium bromide nebulization along with systemic
glucocorticoids partially reduced ventilatory requirements. Negative
sepsis screen (CRP, procalcitonin, blood and tracheal culture) ruled out
possibility of infection. Chest imaging (X-ray and CECT)
suggested complete left lung collapse. Flexible bedside-bronchoscopy
revealed thick, tenacious mucus plug, completely occluding the left main
bronchus which could not be aspirated by multiple lavage attempts. A
tree shaped, branching bronchial cast was removed from the left main
bronchus via rigid bronchoscopy (Fig. 1a). Baby was weaned
off from ventilator over next 24 hours. Nebulized 3% saline was used
along with chest physiotherapy for pulmonary toileting. Charcot-Leyden
crystals with eosinophils and polymorphs were demonstrated on
cytopathological examination of broncho-alveolar lavage (BAL) (Fig.
1b). Cast histopathology showed eosinophils with necrotic background
(type1 variety). Total immunoglobulin E (IgE) level was raised (276
IU/ml) with positive skin prick test (SPT) for buffalo dander. SPT for
milk, egg, house dust, house dust mite, cow dander and wheat grass were
negative. SPT was done with commercially available allergen extracts (Alcure
Pharma) for local flora and fauna with valid positive and negative
controls. Sweat chloride test and echocardiography was normal. The
eczematous lesions over his back responded well to topical therapy. With
a suggestive history of atopy, skin and respiratory manifestations,
presence of Charcot Leyden crystals with eosinophils in cast and
positive SPT for buffalo dander, an IgE-mediated allergic phenomenon was
the most appropriate possibility. He was discharged on inhaled
corticosteroids and oral montelukast with instructions to avoid buffalo
dander, by shifting to maternal grandparentsí home, and an emergency
action-plan. Inhaled steroids were tapered over next 9 months. The child
remained asymptomatic at 1-year in follow-up on montelukast alone and
allergen avoidance measures.
 |
|
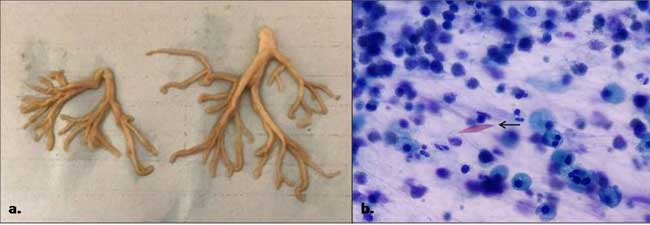
Fig.1 (a) Branching bronchial cast
removed from left main bronchus; (b) red-colored diamond shaped
Charcot-Leyden crystal (arrow) seen in the background of
eosinophils and polymorphs in cytopathological examination of
BAL fluid.
|
Plastic bronchitis is a rare disease, with unknown
prevalence, characterized by formation of thick, cohesive casts leading
to complete or partial occlusion of the airway. Type I casts have
cellular infiltrates, fibrin and are primarily associated with pulmonary
disease like asthma, cystic fibrosis and ABPA, while type II are
acellular casts with, mucin and few mononuclear cells, mainly seen in
cardiac conditions. It has been classified as per underlying etiology
into mucinous (structural CHDs), chylous (lymphatic disorders),
inflammatory (atopy-asthma), and fibrinous casts in sickle cell acute
chest syndrome (SCACS) [1]. It has also been documented after Fontan
procedure, probably due to maladaptation to cavo-pulmonary circulation
[2]. Casts associated with atopy or asthma are described as inflammatory
with eosinophils, Charcot Leyden crystals and occasional neutrophils in
a fibrinous background [1]. While expectoration of thick, rubbery,
branching casts is pathogmonic, patients usually present with cough,
dyspnea or sometimes respiratory failure with suspicion of foreign body
aspiration [3]. Management involves cast removal, chest physiotherapy,
Dornase- a or
hypertonic-saline or N-Acetylcysteine nebulization along with treatment
of underlying disease [4]. With adequate supportive management, allergen
identification and targeted measures (including immunotherapy) play an
important role. Only one case of a 10-month infant with milk allergy and
mucinous cast has been reported earlier [5].
Plastic bronchitis is one of the extreme
presentations of allergic airway disorders. Animal dander exposure is
common in developing world where increasing number of allergies are
being recognized. The index case highlights the unique presentation of
possible buffalo dander hypersensitivity in an atopic infant.
REFERENCES
1. Madsen P, Shah SA, Rubin BK. Plastic bronchitis:
New insights and a classification scheme. Paediatr Respir Rev. 2005; 6:
292-300.
2. Singhi AK, Vinoth B, Kuruvilla S, Sivakumar K.
Plastic bronchitis. Ann Pediatr Cardiol. 2015;8:246-8.
3. Werkhaven J, Holinger LD. Bronchial casts in
children. Ann Otol Rhinol Laryngol. 1987;96:86-92.
4. Kumar A, Jat KR, Srinivas M, Lodha R. Nebulized N-Acetylcysteine
for management of plastic bronchitis. Indian Pediatr. 2018;55:701-3.
5. Bowen AD, Oudjhane K, Odagiri K, Liston SL,
Cumming WA, Oh KS. Plastic bronchitis: Large branching mucoid bronchial
casts in children. Am J Roentgenol.1985; 144: 371-5.
|
|
|
 |
|

