|
|
|
Indian Pediatr 2020;57:
753-754 |
 |
Novel Coronavirus Mimicking Kawasaki Disease in an Infant
|
|
Bhaswati C Acharyya1*, Saumyabrata
Acharyya2 and Dhritabrata Das3
Departments of 1Pediatric Gastroenterology,
2Pediatrics, and 3Pediatric Cardiology, AMRI Hospitals,
Kolkata, West Bengal, India.
Email: [email protected]
Published online: May
22, 2020;
PII: S097475592000659
|
|
C
oronavirus disease (COVID-19) caused by
severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
uncommonly causes severe disease in children [1]. Over the last
two months; however, a new hyper inflammatory condition
manifesting as Kawasaki disease or Kawasaki-like shock syndrome
has been described in children above 4 years of age, across
Europe and USA [2-4], with increased risk of mortality. One case
from India has also been reported [5]. Here we report an infant
presenting with fever and clinical manifestations of Kawasaki
disease and subsequently screening positive for COVID-19.
A 4-month-old healthy baby, weighing 5.6 kg,
and born to non-consanguineous parents, presented with
high-grade fever for 4 days. Fever was spiking 6-8 hourly
reaching 39 0C. He developed an erythematous macular rash over
the trunk, palm and sole on second day. On admission the child
was hemodynamically stable and was breastfeeding normally. He
was very irritable with red lips, congested throat and small
cervical lymphadenopathy without any cough or nasal congestion.
He had clear chest, normal regular heart sounds and a saturation
of 97-98% in air. Investigations revealed a hemoglobin of 9.9 g/dL,
total leucocyte count of 14770/mm3 with 50% neutrophils,
platelet count 4.25×109/L, C-reactive protein (CRP) of 115.6
mg/L, normal liver enzymes with albumin 30 g/L and globulin of
22 g/L, and a normal chest X-ray. His nasopharyngeal swab
was sent for SARS-CoV-2 RT-PCR and other viral PCR tests.
Treatment was started with meropenem and vancomycin after
sending blood and urine culture, but fever continued till the
third day of admission, when he developed non-purulent
conjunctivitis with left subconjunctival hemorrhage. Repeat CRP
showed a higher value of 178.2 mg/L. With evolving clinical
signs simulating Kawasaki disease, an echocardiography was
performed. It showed normal left ventricular function,
perivascular brightness and diffuse ectasia of coronary arteries
with left middle coronary artery (LMCA) of 2.7 mm (Z
score +2.6) (Fig. 1a), left anterior descending
artery of 2 mm (Z score +2.9) and proximal right coronary
artery (RCA) of 2.4 mm (Z score +3.6) (Fig. 1b).
Oral aspirin (80 mg/kg) and intravenous immune-globulin (IVIG)
(2 g/kg) therapy was started. He stayed stable clinically and
did not need intensive care. Fever subsided after 24 hours of
finishing IVIG infusion, and the child became playful.
Subsequently, SARS-CoV-2 reverse transcriptase polymerase chain
reaction (RT-PCR) showed a positive result and he was shifted to
a COVID-designated hospital. All cultures were negative till 7
days. Repeat blood test revealed a downward trend of CRP (148
mg/L). Swab for other viruses was negative. To date the baby is
stable, afebrile, and is kept under observation in the pediatric
ward. His mother was also subsequently found positive for
SARS-CoV-2.
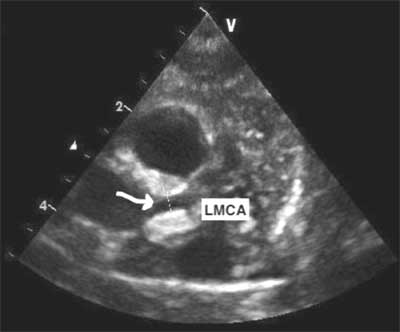
(a) |
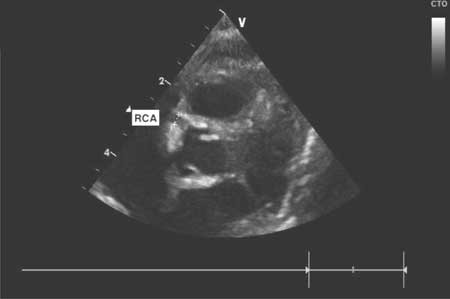
(b) |
|
Fig. 1 Ectasia of (a)
left main coronary artery (LMCA) and (b) right coronary
artery (RCA).
|
Children of all ages can acquire COVID-19,
although they appear to be affected less commonly than adults
[1,6,7]. The most common symptoms in pediatric SARS-CoV2
infection are fever and cough [1,6]. This infant also presented
with fever but his extreme irritability was unusual. In a
previous series, approximately 11% of infants had severe or
critical disease [1]. This infant was never critical throughout
the period of hospitalization.
During this pandemic, Jones, et al.
[2] published the first case of a 6-month-old female admitted
and diagnosed with classic Kawasaki disease, which tested
positive for COVID-19. This was followed by more similar reports
of children with COVID-19 and clinical features that are similar
to those of toxic shock syndrome and atypical Kawasaki disease
and laboratory findings associated with increased inflammation
[3-5]. Royal College of Paediatrics and Child Health (RCPCH)
labeled this new inflammatory entity as Paediatric multisystem
inflam-matory syndrome temporally associated with COVID-19 [8].
Case definitions include persistent fever, inflammation and
evidence of single or multi-organ dysfunction after exclusion of
other microbial causes. The case mentioned showed a rise of CRP
without any neutrophilia, lymphopenia or organ dysfunction.
Our case was very similar to that described
by Jones, et al. [2] but that girl had persistent
tachycardia and most of the clinical features of KD with normal
echocardiography. Riphagen, et al. [3] reported a case
series of 8 children (only 3 tested COVID-19 positive) needing
intensive care support with a hyper-inflammatory shock. One
child died after a massive cerebral infarction. All of them had
features mentioned in RCPCH guidelines with minimal respiratory
symptoms [3]. These children and the two infants with Kawasaki
disease most likely had a similar pathogenesis with varied
consequences, which needs further research to define it.
India is still in the early stage of this
pandemic and has not yet had many children with severe COVID-19.
This 4-month-old child presenting as typical Kawasaki disease
represents a novel presentation among the very young population
with COVID-19.
REFERENCES
1. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang
Z, et al. Epidemiology of covid-19 among children in
China. Pediatrics. 2020; 145. Available from: www.
aappublications.org/news. Accessed May 10, 2020.
2. Jones VG, Mills M, Suarez D, Hogan CA, Yeh
D, Segal JB, et al. COVID-19 and Kawasaki disease: Novel
virus and novel case. Hosp Pediatr. 2020. Available from:
https://hosppeds.aappublications.org/content/hosppeds/early/2020/04/06/
hpeds.2020-0123.full.pdf. Assessed May 10 2020.
3. Riphagen S, Gomez X, Gonzalez-Martinez C,
Wilkinson N, Theocharis P. Hyperinflammatory shock in children
during COVID-19 pandemic. Lancet. 2020 (Epub ahead of print).
Available from: https://www.thelancet.com/journals/
lancet/article/PIIS0140-6736(20)31094-1/fulltext. Accessed
May 11, 2020.
4. Rivera-Figueroa A, Santos R, Simpson S,
Garg P. Incomplete Kawasaki disease in a child with Covid-19.
Indian Pediatr. 2020 May 9 [Epub ahead of print]. Available
from: https://
www.indianpediatrics.net/COVID29.03.2020/CCL-00179. pdf.
Accessed May 21, 2020.
5. Balasubramanian S, Nagendran TM,
Ramachandran B, Ramanan AV. Hyper-inflammatory syndrome in a
child with COVID-19 treated successfully with intravenous
immunoglobulin and tocilizumab. Indian Pediatr. 2020 May 10 [Epub
ahead of print]. Available from: https://
www.indianpediatrics.net/COVID29.03.2020/CCL-00180. pdf.
Accessed May 21, 2020.
6. CDC COVID-19 Response Team. Coronavirus
Disease 2019 in Children - United States, February 12-April 2,
2020. MMWR Morb Mortal Wkly Rep. 2020;69:422 6.
7. Balasubramanian S, Rao NM, Goenka A,
Roderick M, Ramanan AV. Coronavirus disease (covid-19) in
children - What we know so far and what we do not. Indian
Pediatr. 2020 Apr 9 [Epub ahead of print]. Available from:
https://www.indianpediatrics.net/COVID29.03.2020/SA-00159. pdf.
Accessed May 09, 2020.
8. Royal College of Paediatrics and Child Health. COVID-19
guidance for pediatric services. Available from:
https://www.rcpch.ac.uk/resources/guidance-paediatricmulti
systeminflammatory-syndrome-temporally-associated covid19.
Accessed May 11, 2020.
|
|
|
 |
|

