|
|
|
Indian Pediatr 2021;58: 383-390 |
 |
IAP Guideline on Practicing Safely During
COVID-19 Era: Clinics and Small Establishments
|
|
GV Basavaraja, 1
Supraja Chandrasekar,2
Arun Bansal,3
Dhiren Gupta,4
Bakul Jayant Parekh,5
SS Kamath,6
Snehal Desai,7
Pritesh Nagar,8
Nitin Shah,9
Atanu Bhadra10 and AJ
Chitkara11 for
Indian Academy of Pediatrics
From 1Paediatric Intensive Care Unit, Indira Gandhi
Institute of Child Health, Bangluru, Karnataka; 2Columbia Asia Referral
Hospital, Yeshwanthpur, Bengaluru; 3Division of Pediatric Critical Care,
Department of Paediatrics, Advanced Paediatrics Centre, Postgraduate
Institute of Medical Education and Research (PGIMER), Chandigarh;
4Pediatric Intensive Care Unit, Sir Ganga Ram Hospital, New Delhi;
5President (2020), Indian Academy of Pediatrics; 6Department of
Pediatrics, Indira Gandhi Cooperative Hospital, Ernakulum, Kerala;7
Amruta Hospital, Surat, Gujarat; 8Consultant Pediatric Intensivist,
Hyderabad, Telangana; 9Department of Pediatrics, PD Hinduja Hospital,
Mumbai, Maharashtra; 10ESI Hospital, Asansol, West Bengal; and
11Department of Pediatrics, Max Superspeciality Hospital, Shalimar Bagh,
New Delhi; India.
Correspondence to: Dr Arun Bansal, Professor,
Department of Pediatrics, Advanced Pediatrics Centre, Postgraduate
Institute of Medical Education and Research (PGIMER), Chandigarh, India.
Email: [email protected]
|
|
Justification: The
unprecedented COVID-19 pandemic has had a formidable impact on
Indian health care. With no sight of its end as yet, various
establishments including the smaller clinics and nursing homes
are restarting full operations. Hence, there is the need for
recommendations to allow safe practice ensuring the safety of
both the heath care worker (HCW) and patients. Process:
Indian Academy of Pediatrics organized an online meeting of
subject experts on 27 July, 2020. A committee was formed
comprising of pediatricians, pediatric and neonatal intensivists,
and hospital administrators. The committee held deliberations
(online and via emails) and a final consensus was reached by
November, 2020. Objectives: To develop recommendations to
provide a safe and practical healthcare facility at clinics and
small establishments during COVID times. Recommendations:
The key recommendation to practise safely in this setting are
enumerated. Firstly, organizing the out-patient department
(OPD). Secondly, appropriate personal protective equipment (PPE)
to provide protection to the individual. Thirdly,
decontamination/disinfection of various common surfaces and
equipment to prevent transmission of infection from fomites.
Next, maintaining the heating ventilation and air conditioning
(HVAC) to provide a stress-free, comfortable, and safe
environment for patients and HCWs. Finally, steps to effectively
manage COVID-19 exposures in a non-COVID-19 facility. All these
measures will ensure safe practice during these unprecedent
times in clinics and smaller establishments.
Keywords: Preparedness, Physical
distancing, Resource-limited setting, SARI.
|
|
T
he healthcare industry not only bears the brunt
of the coronavirus disease (COVID-19) epidemic, but has also to mitigate
its spread too. In this regard, putting strict practices and processes
in place that are suitable to the local needs and resources will be
paramount in fighting this disease effectively.
The Indian Academy of Paediatrics (IAP) has therefore
come out with the following guidelines on practicing safely in clinics
and small establishments during these unprecedented times.
OBJECTIVES
To develop recommendations to provide a safe and
practical health care facility at clinics and small establishments
during COVID times, and to ensure safety of the healthcare workers
(HCW), and patients at clinics and small establishments.
PROCESS
The Indian Academy of Pediatrics organized an online
meeting of subject experts on 27 July, 2020. A committee was formed
comprising of pediatricians, pediatric and neonatal intensivists, and
hospital administrators. The committee held various deliberations
(online and via emails) and a final consensus was reached by November,
2020.
RECOMMENDATIONS
The guidelines are applicable for clinics,
polyclinics, and level 1 hospitals.
A clinic is defined as a clinical establishment
providing examination, consultation, and prescription to outpatients,
including dispensing medicines by a single doctor, general practitioner,
specialist, or a super-specialist doctor. A polyclinic is similar but
managed by more than one doctor, general practitioner, specialist, or a
super-specialist doctor. [2] A Level 1 (A) hospital is a general medical
service with an indoor admission facility, provided by recognized
allopathic medical graduate(s) and may also include general dentistry
services offered by recognized BDS graduates. Example: Primary Health
Care Centre (PHC), government and private hospitals, and nursing homes
run by MBBS doctors. A Level 1 (B) hospital shall include all the
general medical services provided at level 1(A) and indoor and OPD
specialist medical services provided by doctors from one or more basic
specialties, namely general medicine, general surgery, pediatrics,
obstetrics and gynecology, and dentistry. [3]
The guideline will be discussed under these broad
subheadings
• Organising the Out Patient Department [OPD]
• Personal Protective Equipment (PPE) and
Innovation
• Sanitisation Recommendations
• Heating Ventilation and Air Conditioning [HVAC]
• Protocol for post-Covid-19 exposure in a
Non-Covid-19 zone
Organizing The Outpatient Department
1. Staff Skills Training and Education -
The first step in organizing the OPD is the education
of HCW on PPE, disease transmission, screening techniques, cohorting
patients, and newer clinic management protocols. [4] The clinician
should be prepared for HCW’s illness & subsequent quarantine by training
the staff to multitask and alternating their duties. [5] In the Indian
scenario, with constraints in the availability of skilled staff,
prevention is the key.
2. Tele Consultation - With the legalization
of teleconsultations, it is recommended wherever feasible. [6] It helps
to identify patients who can be managed at home and those who need
hospital care. It minimizes patient contact and is a useful triaging
tool. The teleconsultation guidelines laid down by the government need
to be followed [7].
3. Appointments and Patient Scheduling - Limit
the number of patients per day. Walk-In consultations should be
discouraged to avoid overcrowding. Patient segregation & triaging to be
done while scheduling appointments [6].
4. Physical Distancing and Waiting Areas -
Clinics should preferably have no waiting areas. However, when more than
one person arrives, their seats should be at least 1 meter apart. [5,6]
Open ventilation is encouraged here [refer section on HVAC]. In single
room OPD chambers, it would be prudent to call one patient at a time;
others can wait outside in the open air or their vehicles.
5. Patient Segregation - It is prudent to
cohort children who are ill from the well-baby visits. Many clinics are
operated only by the practicing doctor. However, it is recommended to
have a helper who will assist in triaging, maintaining decorum, and
educating patients. Preferably an initial screening should be followed
by separation of those suspected of COVID-19 from others. These cases
should not spend time in the waiting area and should be seen
immediately. A separate entry, consultation place & exit, if feasible,
will help. [4] As not all clinics have the facilities mentioned above,
alternate precautions should be followed:
• Telephonic triaging and schedule appointments
for all suspect cases after routine OPD [6]
• Exclusive days should be allotted for ‘Well
baby’ & Immunization checks once or twice a week. This may even
boost parents’ morale who otherwise would be scared to come to
clinics for vaccinations.
6. Patient Education and Awareness - All
patients should follow respiratory hygiene and cough etiquette. Patients
should be provided with tissues, contactless bins, contactless
sanitizers, and wash areas. Display these instructions in prominent
locations. Patient education is also the physician’s responsibility,
hence putting educative posters, multimedia information at strategic
points is useful. [4,6]
7. One Attendant and Personal Protection -
Allow only one parent or guardian with the child. [5] Everybody,
including children above two years, should wear a mask.
8. Well Ventilated - Follow the ventilation
guidelines provided in this document.
9. Avoid Fomites - Remove toys, magazines, and
any items that are likely to be shared between patients in the waiting
area or consultation chambers. [4]
10. Novel Techniques - Innovative
methods have been tried by various doctors and can be utilized.
• Using transparent physical barriers between the
patient and doctors can help in decreasing direct exposure to
droplets.
• Virtual detailed video interaction followed by
a rapid, focused examination of the patient in another chamber
minimizes the patient contact time.
• Non-Contact Thermal scanners- These are
convenient non-contact devices ideally suited for mass screening in
a pandemic and have wide acceptability. However, they lack robust
evidence. A recent systematic review showed reasonable diagnostic
accuracy in fever detection but may vary with patient
characteristics, setting, index test, and the reference standard
used. These have an excellent negative predictive value. [9]
However, there are more recent studies doubting its accuracy during
screening in a pandemic. [10] Hence, no specific recommendations are
available for or against the use of these devices.
Personal Protective Equipment [11]
PPE, along with other measures like engineering and
administrative protocols, reduces the exposure of HCW to infectious
agents, including the SARV-CoV2 virus. HCW has 11-fold higher chances
of getting infected with the SARS-CoV2 virus than the general
population. The use of PPE can reduce that risk by 60-80% when exposed
to COVID-19 suspected or proven cases. Various components of PPE and its
benefits are given in Supplementary Table I.
Donning and Doffing PPE
An essential part of PPE is the proper way of putting
it on (Donning) and removing (Doffing) as the maximum chances of
contamination and infection occur during doffing. The steps and sequence
of donning and doffing of N-95 masks and PPE are given in
Supplementary Table II. All PPE components, especially face masks
are effective only when used in combination with frequent hand hygiene.
Type of exposure and use of PPE for HCW
Every patient should be taken as a COVID-19 suspect
unless proven otherwise. Appropriate PPE should be universally worn when
attending to any patient, even in a non-COVID-19 centre.
• In non-aerosol generation areas - head cap,
face mask, goggles, and gloves.
• For aerosol generation areas and procedures -
In addition, wear body gowns, shoe cover, and face shield.
• While attending a proven COVID-19 patient -
Full Hazmat suit PPE.
• Nonmedical staff not in direct contact with
patients - triple-layer surgical masks and gloves inside the clinic.
They must maintain physical distancing and frequently use hand
hygiene.
Patient PPE
• All patients and their attendants should wear a
mask.
• Using a triple layer surgical mask or N-95, if
possible, significantly reduces the risk of transmission.
Adjuncts to PPE
• Patients often complain that the doctor is not
audible with PPE. One adjunct is to use a wireless or wired mini
personal voice amplifier
• The use of the mobile phone is inevitable but
often results in the breach of PPE. Hence, using a blue tooth
device, preferably with bone conduction that doesn’t plug the ear,
is advised.
• Rexene covers or disposable paper covers/sheets
for the patient sitting/lying areas.
• Contactless/foot operated dispensers for
soap/sanitizer/water in washbasins.
Sanitization Recommendations
Despite consistent evidence of contamination of
various surfaces with SARS CoV 2 virus, especially in the hospital
setting, there is no direct evidence of fomites being a cause of
transmission. [12] However, it is imperative to follow some necessary
sanitization precautions for the decontamination/disinfection of
COVID-19, as given in Table I. These are based on the Hospital
Infection Prevention and Control guidelines drafted by the National
Centre for Disease Control and the WHO. [13]
Spraying and Fogging
Spraying, fogging, misting, or fumigation of rooms or
surfaces is not recommended for COVID-19. Spraying of chemicals is
harmful, affecting the mucus membrane, skin, and respiratory system. The
recommended method is to wipe with a disinfectant soaked cloth
Hand Hygiene
Patients, attendants, and HCW’s are advised to wash
hands with soap and water in a washbasin with foot-operated or motion
sensor adapted taps. Everyone should use Foot-operated hand sanitizer
dispensers before entering the clinic.
Sanitizers
The composition of sanitizers is 60-70%
ethanol or isopropyl alcohol. Avoid methanol containing or non-alcohol
based sanitizers. Foot operated and Contactless sanitizer delivery
systems are safe and effective.
Heating ventilation and air conditioning (HVAC)
Maintaining the HVAC plays a vital role in providing
a stress-free, comfortable, and safe environment for patients and health
care workers. Maintaining indoor air quality is very important to
prevent cross-contamination and hospital-acquired infections.
Importance of HVAC in the context of COVID 19
1) The SARS (Severe Acute Respiratory Distress
Syndrome) epidemic in the past has taught us that there was an
increased rate of intrahospital spread of infection, and it was
attributed to architectural factors and HVAC systems. The SARS-CoV2
virus is resistant to various temperatures. Unfortunately, people
are switching off air conditioning [AC] facilities to curb the
spread. However, this is ineffective and, in fact, harmful as it
creates adverse working conditions.
2) It is a misconception that if we maintain
moderate humidity, the virus growth and propagation can be
prevented. Unfortunately, this virus seems to be very resistant to
environmental changes like temperature and humidity. It requires an
extreme relative humidity of more than 80 percent and a
temperature of more than 50 degrees Centigrade to control. These
conditions are neither attainable nor acceptable. [14]
Air changes per hour (ACR)
Air changes per hour (ACR) are the number of
total replacements of any room’s air in one hour. If the air supply by
the HVAC system in one hour is equal to the volume of the space, then it
is called one air change per hour. The number of air exchanges required
to clean the air depends on the quantum of infected aerosol production.
For example, a minimum of 12 ACR is needed in the Intensive Care Unit
(ICU). In contrast, only 4 ACR is required for general wards, as the
expected amount of aerosol production is different in both areas.
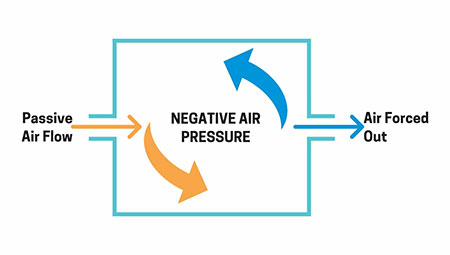
There are two ways to reduce the quantum of infection
in contaminated air, either by ‘diluting’ the pathogen (dilution
ventilation) or by removing the pathogen (exhaust ventilation).
Dilution Ventilation is also called positive pressure isolation,
required to prevent infection in an immunocompromised patient. Exhaust
Ventilation is called negative pressure isolation and is used
primarily to avoid a contaminated patient’s airborne disease [15] (Fig.
1).
 |
|
Fig. 1 Principle of HVAC to prevent
airborne spread.
|
Ways To Create Air Exchanges Via Exhaust Ventilation:
1) Cross Ventilation by opening up doors
and windows: This is the cheapest way, but by this method, we cannot
control the thermal and pollution level.
2) Exhaust Fan: The exhaust fan creates a
negative pressure in the room, which sucks the dirty and
contaminated air out of the room, and fresh air is pulled to replace
it.
3) Fully Controlled Air: Air inlet, as
well as exhaust air, is fully controlled, including the temperature
and filtration. This requires a lot of resources, including
technology, and is best suited for negative pressure isolation wards
and ICUs.
4) Air Purifying Systems: This cleans the
air either via filtration (e.g., HEPA) or via other techniques like
ultraviolet rays. Recirculation of air has to be prevented for this
system to be effective.
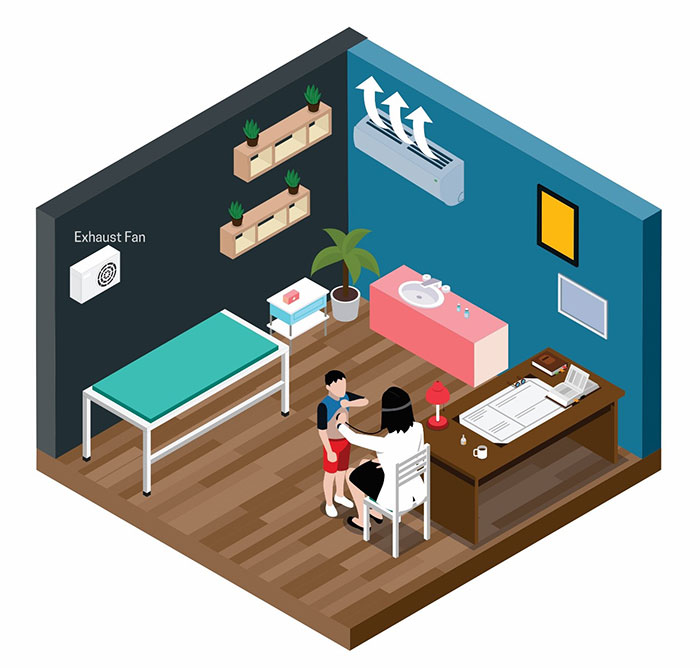
The airflow should be in the direction of clean to
dirty and should not be directed towards the patient as it causes
turbulence. (Fig. 2)
 |
|
Fig. 2 Clinic setting - Placement of
exhaust fan, one feet above the ground. Direction of air should
be from clean to dirty (patient side). Flow of AC air should be
directed towards celling.
|
Plasma Purifiers
Plasma purifiers are specialized newer technology
air purifiers. Originally these purifiers were very large and
cumbersome, however, with significant advancements in technology, they
have become compact and a part of the HVAC with the ionization tubes
mounted in the air conditioning, either in the unit itself or in the
ductwork. These ionization tubes form ions (negatively or positively
charged particles) as air circulates over them. The ions that are
produced act in three ways to purify the air:
1) Sterilize bacteria and mould. When
bacteria, virus and spores of mould come in contact with the ions,
they are oxidized and destroyed. They can no longer multiply and are
eliminated from the air.
2) Reduce particles in the air. The ions
produced by the system bond with the toxins in the air, causing
these particles to become larger. That makes them easier to be
capture in the filters, reducing the number of toxin particles in
the air.
3) Control odors. Odors associated with
household aerosols or cleaning products are "captured" by the ions,
oxidized, and eliminated.
The viricidal properties of the Plasma purifiers may
be used while installing the HAVAC in the clinics and small
establishments. However further evidence is required regarding its
efficacy during this pandemic.
Recommended HVAC Modifications For Healthcare
Facilities:
Different recommendations for HVAC for various
healthcare facilities are given in Supplementary Table III and
Figs. 1,2 & 3.
Covid-19 Exposure In A Non-Covid Health Facility
There are various situations where a Non-COVID-19
facility is faced with a COVID- 19 challenge. The possible problems and
recommendations are enumerated.
When patients admitted for unrelated/non-respiratory
illness turn out to be COVID-19 positive
1. Inform the local health authorities
2. Assign anyone dedicated HCW, wearing a full
PPE, to attend to this case
3. The patient should be shifted to a separate
designated isolation area.
4. Arrange for transfer to a COVID-19 isolation
facility after due communication
5. Follow appropriate standard precautions while
transporting the patient
6. Followed by disinfection procedures at the
facility and the ambulance
7. All contacts (see below) should be identified,
risk assessment is done and subsequently follow the testing and
quarantine recommendations.
8. All high-risk contacts should be put on
Hydroxychloroquine [HCQ] chemoprophylaxis for seven weeks, keeping
in mind the contraindications of HCQ.
HCW turn out to be positive for COVID-19 [16]
1. HCWs developing respiratory symptoms (e.g.,
fever, cough, shortness of breath) should be considered a suspected
case of COVID-19.
2. Should immediately inform his supervisor.
3. Should be isolated, and arrangements must be
made to refer to a COVID-19 designated hospital (if not already
working in such a facility) for isolation and further management.
However, asymptomatic, and mildly symptomatic HCW’s need to be home
isolated under supervision.
4. Should be immediately taken off the roster
5. All health facilities must have a staffing
plan in place for such an event to maintain continuity of operations
6. Ensure that the disinfection procedures are
strictly followed
The decision on further /continued use of
non-COVID-19 facilities where a single/multiple
COVID-19 case has been reported [16]
1. If the hospital authorities are reasonably
satisfied that the source case/s have been identified and isolated,
all contacts have been traced and quarantined, and adequate
disinfection has been achieved, the hospital will continue to
function.
2. In addition to the steps taken above, if the
health facility continues to report new hospital-acquired COVID-19
cases in the following days, it would be advisable to temporarily
close the health facility’s defined section where the maximum number
of patients are being reported.
3. After thorough cleaning and disinfection, it
can be put to use again.
4. Local guidelines for the region should be
followed
Standard Operating Procedure to be followed in case
HCW reports exposure/breach of PPE [17]
1. All the HCW must report every exposure to
COVID-19 to the concerned nodal officer and Head of the concerned
department immediately
Definition of Contacts
A contact is a person who is likely to get the
infection from a positive case through any of the following modes of
transmission
• Anyone exposed to a COVID -19 positive case 2
days before and 14 days after the onset of symptoms or date of
testing
• The duration (>15 minutes) and proximity (<
1meter) of exposure and the use of appropriate PPE during exposure
are an important consideration in defining the contact
Primary /High-Risk Contact
• Anyone with proximity within a 1-meter distance
of the confirmed case
• Anyone who touched or cleaned the linens,
clothes, utensils of the patient
• Had direct physical contact with the patient
including examination or touched the body secretions including blood
saliva, urine, etc. without appropriate PPE
• Anyone who has come in contact with
aerosol-generating procedures is considered to be high-risk contact
Secondary/Low-Risk contact
• Any contact not fitting into the above
description
• Low-Risk contacts also can be spreaders of
infection hence need monitoring
Risk Assessment
The risk assessment of close contacts with COVID-19
patients is given in Table II.
Table II Risk Assessment of Close Contacts
| Prolonged close
contact with a COVID-19 patient who was not wearing a
facemask (i.e., no source control) |
| Epidemiological Risk Factor |
Risk |
| HCP PPE: None |
High |
| HCP PPE: Not wearing a surgical
facemask or |
High |
| N95 mask |
|
| HCP PPE: Not wearing eye
protection |
Medium |
| HCP PPE: Not wearing a gown or
gloves |
Low |
| HCP PPE: Wearing all
recommended PPE (except |
Low |
| wearing a surgical
facemask instead of an N95 mask) |
|
| Prolonged close contact with a
COVID-19patient who was wearing a facemask (i.e., source
control |
|
| Epidemiological Risk Factor |
Risk |
| HCP PPE: None |
Medium |
| HCP PPE: Not wearing a surgical
facemask |
Medium |
| or N95 mask |
|
| HCP PPE: Not wearing eye
protection |
Low |
| HCP PPE: Not wearing a gown or
gloves |
Low |
| HCP PPE: Wearing all
recommended PPE |
Low |
| HCP – Healthcare
professional; PPE – Personal protective equipment. |
Recommendations for Monitoring Based on COVID-19
Exposure Risk [17]
High- and Medium-risk Exposure Category
• HCW in the high- or medium-risk category should
undergo active monitoring, including restriction from work in any
healthcare setting until seven days after their last exposure. [18]
• High-risk contacts will be quarantined for
seven days
• Test for COVID-19 done on day 0 of exposure and
if negative day 7 of exposure
• If they test positive but are asymptomatic,
they will follow the protocol for mild/pre-symptomatic cases
• If they test negative and are asymptomatic,
they should complete a 7-day quarantine from the last date of
exposure and then return to work. Further, they should be in
self-reporting observation at work for another minimum of 7 days and
strictly abide by the mask and physical distancing rules.
• If they develop a fever (measured temperature >
100F or subjective fever) OR respiratory symptoms consistent with
COVID-19 (e.g., cough, shortness of breath, sore throat), they
should immediately test and self-isolate and notify the senior staff
to take further action.
Low-risk Exposure Category
• HCW in the low-risk category should perform
self-monitoring with delegated supervision until 14 days after the
last potential exposure.
• Asymptomatic HCW in this category are not
restricted from work.
• They should check their temperature twice daily
and remain alert for respiratory symptoms consistent with COVID-19
(e.g., cough, shortness of breath, sore throat)
• Test for COVID-19 between day 5 and 14 of
exposure
• Suppose they develop a fever (measured
temperature > 100F or subjective fever) OR respiratory symptoms. In
that case, they should immediately self-isolate (separate themselves
from others) and notify the staff physician promptly so that they
can coordinate consultation and referral to a healthcare provider
for further evaluation.
Disclaimer: This practice guideline is intended
to assist pediatricians and their support staff in safely practicing
during the COVID-19 pandemic. The guideline at best serves as a quick
reference providing practical advice on continuing medical practice in a
safe way in clinics and small establishments. This is a broad advisory
and is not intended to override any local or national government
policies. This guideline is based on the currently available evidence on
COVID-19 and its applicability in the Indian context. With any further
developments, the guideline will be subjected to change.
Contributors: SC, DG, AB, GVB: conception
and design of the work and drafting the work; BJP, SSK, SD, PN, NS, AB,
AJC: substantial contributions to the acquisition and interpretation of
data for the work, and revising it critically for important intellectual
content. All authors provided approval for the final version to be
published.
Funding: None; Competing
Interests: None stated.
Annexure I
Members of National Expert Committee
Dr Bakul Jayant Parekh, President IAP 2020, Dr Basavaraja G -
Chairperson; Prof Arun Bansal – Coordinator; Dr Dhiren Gupta – Convenor;
Dr Supraja Chandrasekar, Dr SS Kamath, Dr Snehal Desai, Dr Pritesh
Nagar, Dr Nitin Shah, Dr Atanu Bhadra, Dr AJ Chitkara.
REFERENCES
1. Clinical Establishment Act Standards for Clinic /
Polyclinic with Dispensary CEA /Clinic- 009 Accessed November 8, 2020.
Available from http://clinicalestablishments.gov.in/WriteRead
Data/5541.pdf
2. Clinical Establishment Act Standards for Hospital
(LEVEL 1A &1B))/ CEA/Hospital – 001. Accessed November 8, 2020.
Available from: http://clinicalestablishments.gov.in/WriteRead
Data/147.pdf
3. American Academy of Family Physicians. Checklist
to Prepare Physician Offices for COVID-19. Accessed July 28, 2020.
Available from
https://www.aafp.org/dam/AAFP/documents/patient_care/publichealth/COVID-19%20Office%20Prep%20
Checklist. pdf
4. Centers for Disease Control. Healthcare
Facilities: Get Your Clinic for Corona Virus 2019 (Covid-19). Published
March 11, 2020. Accessed July 28, 2020. Available from https://www.
cdc.gov/coronavirus/2019-ncov/hcp/clinic-preparedness.html
5. Indian Academy of Pediatrics. Covid-19 Bulletin
2nd Edition. Accessed July 28, 2020. Available from
https://iapindia.org/pdf/Final-Edited-Version-of-IAP-COVID19-Bulletin.pdf
6. Ministry of Health and Family Welfare.
Telemedicine Practice Guidelines. Published March 25, 2020. Accessed
August 1, 2020. Available from
https://www.mohfw.gov.in/pdf/Telemedicine. pdf
7. Indian Academy of Pediatrics. COVID-19 Bulletin
2nd Edition. Accessed July 28, 2020. Available from
https://iapindia.org/pdf/Final-Edited-Version-of-IAP-COVID19-Bulletin.pdf
8. Aggarwal N, Garg M, Dwarakanathan V, et al.
Diagnostic accuracy of non-contact infrared thermometers and thermal
scanners: A systematic review and meta-analysis. J Travel Med.
2020;27:taaa193.
9. Khan S, Saultr, B, Adams S, et al. Comparative
accuracy testing of non-contact infrared thermometers and temporal
artery thermometers in an adult hospital setting. Am J Infect Control.
2020; S0196-6553(20)30892-0. [Epub ahead of print]
10. Guidelines on rational use of personal protective
equipment. Ministry of Health and Family Welfare Directorate General of
Health Services [Emergency Medical Relief]. Accessed October 25, 2020.
Available fromhttps://www.mohfw.gov.in/pdf/Guide
linesonrationaluseofPersonalProtectiveEquipment.pdf
11. National Guidelines for Infection Prevention and
Control in Healthcare Facilities, Ministry of Health and Family Welfare
Directorate General of Health Services, Government of India. Accessed
October 25, 2020. https://ncdc.gov.in/index1.php? lang=1&level=1&sublinkid=692&lid=546.
12. World health Organization, Transmission of
SARS-CoV-2: implications for infection prevention precautions.
Scientific Brief. Accessed October 24, 2020. Available from
https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions
13. How to operate air conditioning and ventilation
systems to control the spread of coronavirus disease (COVID-19) in
Residences, Workspaces, and Healthcare Facilities: IMA HBI- Indian
Society of Heating, Refrigerating & Air Conditioning Engineers COVID-19
GUIDANCE DOCUMENT. Accessed August 11, 2020. Available from https://ishrae.in/mailer/ISHRAE_COVID-19_Guidelines.pdf
14. World health Organization, Natural Ventilation
for Infection Control in Health-Care Settings: Edited by Atkinson J,
Chartier Y, Lúcia Pessoa-Silva C, Jensen P, Yuguo Li, Wing-Hong.
Accessed August 11, 2020. Available from
https://www.who.int/water_sanitation_health /publications /natural
_ventilation
15. Interim United States Guidance for Risk
Assessment and Work Restrictions for Healthcare Personnel with Potential
Exposure to COVID-19. Accessed October 25, 2020. Available from
hhttps://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html
16. Guidelines to be followed on detection of
suspect/confirmed COVID-19 case in a non COVID Health Facility. Ministry
of Health & Family Welfare Directorate General of Health Services
Emergency Medical Relief Division. Accessed October 25, 2020. Available
from https://www.mohfw.gov.in/pdf/Guide
linestobefollowedondetectionofsuspectorconfirmedCOVID19 case.pdf
17. Revised quarantine and testing protocol for
primary/high risk contacts and secondary/low risk contacts.
Commissionerate Health & Family Welfare Services, Government of
Karnataka 15-09-20, No DD/SSU/Circular-06/2020-21.
|
|
|
 |
|

