|
|
|
Indian Pediatr 2020;57:
305-309 |
 |
Impact of a Novel Hypothermia Alert Device on Death of Low
Birthweight Babies at Four Weeks: A Non-randomized Controlled
Community-based Trial
|
|
Mona Sharma1, Virginia Morgan1, Murthy
Siddadiah1, Dinesh Songara2, Rahul Dev Bhawsar2
and
Ambey Srivastava2
From 1BEMPU
Health, Bengaluru, Karnataka; and 2The Wadhwani Initiative
for Sustainable Healthcare (WISH Foundation), Jaipur, Rajasthan; India.
Correspondence to: Dr Mona Sharma, Head of Product Design and
Customer Research, BEMPU Health, 3C Alsa Glenridge Apt, 32, Langford Rd,
Shanti Nagar, Bengaluru, Karnataka 560 027, India.
Email:
[email protected]
Received:
March 13, 2019;
Initial review: July 12, 2019;
Accepted:
November 09, 2019.
Published online: February 5, 2020.
PII: S097475591600139
|
|
Objective: To study the effectiveness of a
hypothermia monitoring device in reducing neonatal mortality
and increasing Kangaroo Mother Care compliance.
Design: Non-randomized controlled trial.
Setting: 3 government Sick Newborn
Care Units and 7 Primary Health Centers in Udaipur and
Dungarpur districts of Rajasthan for 4 months. The follow-up
period was 4 weeks for each baby.
Participants: Total 386 neonates were included in
the study. 250 (64.76%) new-borns in the study group (BEMPU
bracelet) and 136 (35.23%) enrolled in the control group.
Clinically stable babies discharged below 2500 grams, whose
parents could be reached by phone, and who could visit the
facility for 4 weekly follow-ups were eligible for
participation. Infants with complications or those leaving
against medical advice were not eligible.
Intervention: The BEMPU Bracelet is a medical
device that provides 4 weeks of continuous hypothermia
monitoring for new-borns, and emits an audio-visual alarm
when the temperature of the newborn is below 36.5įC.
Outcome: Neonatal mortality over the
4-week period.
Results: Mortality
data was obtained for 92% (229 babies) of the study group
and 91% of the control group (124 babies) at the end of the
4-week period. The intervention group had a significantly
lower mortality rate as compared to the control group (6%
vs. 14%, P=0.013). Weight data from 51% of the study group
(128 babies) and 32% of the control group (44 babies) did
not show a significant difference in weight gain between the
groups.
Conclusion: The observed
effect on mortality and qualitative feedback on KMC
compliance suggest the utility of the device in the
community settings.
Keywords: Body
temperature, Kangaroo Mother Care, Neonatal mortality,
Community health.
|
|
Approximately 27 million babies are born in India every
year and out of those 8 million are LBW [1], these include over 3.3
million preterm births per year [2]. Such babies are at a high risk of
experiencing life-threatening illnesses. Neonatal hypothermia and
infection, are among the leading causes of newborn deaths and illness in
low-resource settings [3,4]. Infants who are premature and/or low
birthweight struggle to regulate their own tempe-rature, which may lead
to hypothermia. If untreated, hypothermia may lead to reduced weight
gain, which predisposes newborns to sepsis, pneumonia, and even death.
By providing skin-to-skin care, or Kangaroo Mother Care (KMC),
caregivers can prevent or correct hypothermia in neonates without the
assistance of radiant warmers or incubators [4].The World Health
Organization recommends KMC for all low weight babies. However, despite
national KMC policies, uptake of the practice has been low due to social
and logistic barrier [5].
The Indian state of Rajasthan has an
infant mortality rate of 41 infant deaths per 1000 live births [6],
which is comparable to the national average [7]. The National Health
Mission (NHM) Rajasthan identified BEMPU bracelet, a hypothermia
monitoring device, as an intervention with the potential to address
neonatal mortality through hypothermia prevention. This pilot study was
done to assess the effectiveness of this device on mortality amongst low
birthweight neonates.
Methods
This
non-randomized study was conducted in three government Sick Newborn Care
Units (SNCUs) and seven Primary Health Centers (PHCs) in the Udaipur and
Dungarpur districts of Rajasthan, India. The approval to conduct the
study was sanctioned by the Mission Director of National Health Mission
Rajasthan and the Chief Medical and Health Officer, Udaipur, Rajasthan.
A team from the product developers trained the site doctors, nurses,
data entry operators, and Auxiliary Nurse Midwives (ANMs) on the use of
the bracelet, KMC, and data collection procedures. LEHS|WISH (Lord
Education and Health Society|Wadhwani Initiative for Sustainable
Healthcare) assisted with pilot initiation and oversight of data
collection and analysis.
Staff of the facilities enrolled babies
from 29 September, 2016 to 10 January, 2017. Clinically stable babies
discharged weighing below 2500 grams, whose parents could be reached by
phone, and who could come to the facility for 4-weekly follow-ups were
eligible for participation. Infants with complications or those leaving
against medical advice were not eligible for this study. After obtaining
informed consent from parents, SNCU or PHC nurses enrolled the babies.
Total 386 babies were enrolled, of which 250 (64.76 %) were in the study
(BEMPU bracelet) group, and 136 (35.23%) in the control group (routine
care).
Families of babies in both the study and control groups
received discharge instructions on hypothermia awareness and prevention,
KMC, and swaddling techniques. Parents with babies in the study group
also received instructions on how to use the device.
All
participants were followed up for 4 weeks. Parents were also given a
patient- diary to record hours of KMC. Families were asked to come back
for weekly follow-ups for 4 weeks, so staff could collect
anthro-pometric measurements on the newborns. Transportation charges for
the follow-up visits were reimbursed to ensure regular follow-up.
Parents of newborns enrolled in the study also received three
follow-up phone calls to collect information on the health status of
their newborn, KMC compliance, and the device usage, if applicable.
During this call, they were also reminded weekly about their follow-up
appointment. If parents did not answer phone calls, the local ANM was
called to gather follow-up data on mortality and encourage parents to
attend their weekly follow-up. At the fourth follow-up appointment,
parents submitted their patient diary and final anthropometric
measurements were taken. Interviews with parents were conducted to
gather qualitative evidence on KMC compliance and attitudes towards the
device.
Quantitative data on mortality and weight gain from
patient diaries were entered by data entry operators. All quantitative
data was analyzed using the program tool.
The BEMPU bracelet is a
device that provides 4 weeks of continuous temperature monitoring to a
preterm or LBW newborn. It emits an audio-visual alarm when a babyís
temperature drops below 36.5 degrees, indicating that the infant is
hypothermic and prompting caregivers to provide thermal care in the form
of KMC (Web Fig. 1).
The BEMPU bracelet indicators are explained in
WebTable I. It has a
sensitivity of 98.6% and specificity of 95% for detecting neonatal
hypothermia [8].
The NHM/WISH pilot was completed in two
southern districts of Rajasthan state, Udaipur and Dungarpur. The
districts have predominately tribal populations, which represent 47.9%
of the population in Udaipur and 70.8% in Dungarpur [9]. These are
high-priority districts, having a heavy burden of LBW and neonatal
mortality; 49.5% of babies born in Udaipur are LBW and the neonatal
mortality rate in the district is 40 per 1,000 live births. In
Dungarpur, the rate of LBW is 46.9%, with a neonatal mortality rate of
41 [10].
This pilot study was commissioned by the National
Health Mission (NHM) of Rajasthan to assess the feasibility of the
innovation, to inform potential adoption through state budgets. While
this study was not approved by an Institutional Review Board, the
research questions and methods were reviewed and approved by a panel of
experts including senior NHM officials and Chief Medical Officers in
Rajasthan. The study was conducted as per ethical approval carried out
following Helsinki declaration.
Results
Total of 386 newborns were screened for eligibility, enrolled, and
assigned to one of the two study groups; 35 of these were lost to follow
up after discharge, and 31 died during the 4 weeks of study period (Fig.1).
The baseline characteristics are shown in Table I. The
primary conditions of SNCUs newborns enrolled in the studies are
represented in Fig. 1.
Table I Baseline Characteristics of Newborns Discharged From Special Care Neonatal Units in Rajasthan
|
Control group
(n=136) |
Study group
(n=250) | |
No. |
Mean (SD) |
No. |
Mean (SD) | |
Birthweight (kg) |
132 |
1.94 (0.43) |
243 |
1.87 (0.38) | |
Discharge weight (kg) |
132 |
1.88 (0.41) |
243 |
1.89 (0.37) | |
Gestational age (wk) |
94 |
35.2 (3.1) |
74 |
35 (2.8) |
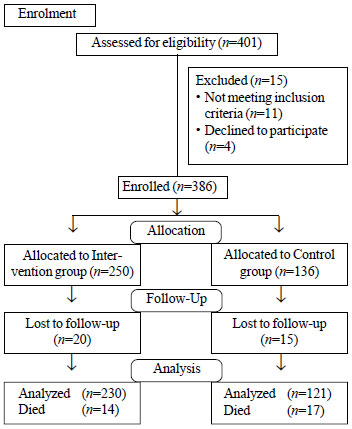 |
| Fig. 1 Study
flow chart. |
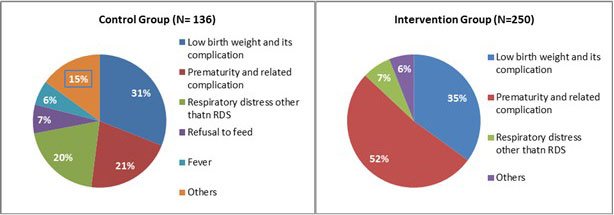 |
| Fig. 1 Primary
conditions of newborns enrolled in the study. |
Mortality data was obtained for 92% of the
study group (229 babies) and 91% of the control group (124
babies) at the end of the 4-week period. Mortality differences
between the groups were statistically significant. The study
group had lower mortality rate (6%) than control group (14%) [OR
(95%CI) = 2.43, (1.59, 5.13); P=0.09]. The characteristics of
the newborns that died are shown in Fig. 2.
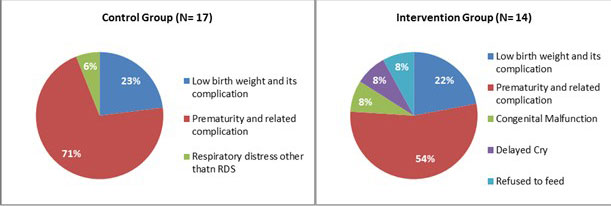 |
| Fig. 2
Characteristics of the low birthweight newborns who died
during the study. |
Due to the low rate of facility-based
follow-up, weight data from only 51% of the study group (128
babies) and 32% of the control group (44 babies) was available
for analysis. The weight gain in the two groups was similar
[2.79 g, 95% CI (2.64, 2.94) vs 2.58 g, 95% CI (2.43, 2.73); P=
0.1019 ].
The KMC tracking charts in patient diaries
were inconsistently filled out making them impossible to be
reliably analyzed; hence, researchers could not perform further
quantitative analysis of this aspect. Web box I shows the
findings of qualitative feedback through semi-structured
interview with 11 parents.
The follow-up rate in BEMPU
group (59.58 %) was higher than the control group (31.34 %),
which indicates that the device promoted a positive behavior
change in the parents on newborn care.
Discussion
Providing appropriate thermal care
can reduce a newbornís risk of hypothermia-related morbidity and
mortality [11]. In this pilot, the study group experienced a
statistically significant lower rate of mortality than did the
control group. Qualitative data collected from interviews with
parents also suggested positive experiences. The follow-up rate
of the study group was almost twice as that of the control
group, suggesting a favorable behavioral change.
The
anthropometric data could not be completely recorded due to
various reasons such as high burden on healthcare staff and many
families living far from the health facilities; and it was a
contributing factor to the loss to follow-up. A larger study is
planned to address these limitations. Probably, due to low
literacy levels, mothers/family members filled out the KMC
tracking chart unsatisfactorily. Other methodologies should be
employed in the future to quantitatively evaluate hours of KMC
performed with and without the BEMPU Bracelet.
The data
for weight gain was difficult to gather and not standardized
between centers and nurses. Some newborns were weighed with
their clothes on, some nurses rounded information to the nearest
half kg, and some centers did not have proper scales.
A
device called ThermoSpot, a non-invasive infant hypothermia
indicator, that adheres to the skin of and indicates infant
hypothermia or a fever by a change of color was studied in the
community to understand the impact of behavior change on newborn
care [12]. The results of the study revealed that there was an
improvements in birth preparedness, hygienic delivery, thermal
care (including skin-to-skin care), umbilical cord care, skin
care, and breastfeeding [12]. There was little change in
care-seeking. Many of the other hypothermia detection devices
have not been studied in the com-munity. BEMPU braceletís
simple, easy to understand audio-visual alarm feature
distinguish it from other similar interventions. The
audio-visual indications can be understood by any mother and
family members across all socio-economic groups.
In
areas where the risk of neonatal hypothermia is high due to the
prevalence of preterm birth and low birth weight, use of the
BEMPU Bracelet among these vulnerable babies could result in
reduced mortality through provision of thermal care. The
observed reduction in mortality and positive parental feedback
on KMC promotion in this study supports the BEMPU braceletís
potential to impact neonatal health outcomes. This warrants
further research to assess the braceletís impact on newborn care
practices.
Acknowledgements: Mission Director of National
Health Mission Rajasthan and the Chief Medical and Health
Officer in Udaipur for their encouragement and guidance. Annika
Gage, Abby Smith, and Kembo Matungulu for their work in revising
the manuscript for intellectual content.
Contributors:
MS: conception and design of the study, VM: data analysis,
drafting manuscript, MS: conception and design of study; DS:
acquisition of data; RDB: implementation of the study, AS: data
analysis. All authors approved the final version of manuscript
and agree to be accountable for all aspects of the work in
ensuring that questions related to the accuracy or integrity of
any part of the work are appropriately investigated and
resolved.
Funding: The cost of the BEMPU bracelets
involved in the study were supplied to the NHM Rajasthan using
the grants of Grand Challenges Canada via BEMPU Health. For the
study, the BEMPU Bracelets were provided free of cost by BEMPU
Health, and the data entry operators responsible for entering
all collected data were compensated by BEMPU Health.
Competing interests: All data collection was overseen by the
National Health Mission Rajasthan and the WISH Foundation. Data
analysis and the authorship of this publication were shared
between BEMPU Health and the WISH Foundation. BEMPU Health team
conducted the training required for the bracelet use. Staff of
the NICUs of the hospitals in the studies carried out the study.
References
1. The United Nations
Childrenís Fund. Low Birth weight: Country, Regional and Global
Estimates, 2019. Available from:
https://www.unicef.org/publications/index_24840. html. Accessed
August 20, 2019.
2. India: Profile of preterm and low
birth weight prevention and care. Available from: https://www.
healthynewborn network.org/hnn-content/uploads/India-1.pdf/
Accessed August 20, 2019.
3. Lunze K, Bloom D, Jamison D,
Hamer, D. The global burden of neonatal hypothermia: Systematic
review of a major challenge for newborn survival. BMC Medicine.
2013;11:24.
4. Lunze K, Hamer D. Thermal protection of
the newborn in resource-limited environments. J Perinatol.
2012;32: 317-24.
5. Chan G, Labar A, Wall S, Atun R.
Kangaroo mother care: a systematic review of barriers and
enablers. Bull World Health Organ. 2015;94:130-41J.
6.
The National Family Health Survey 2015-16. State fact Sheet
Rajasthan. Available from:
http://rchiips.org/NFHS/pdf/NFHS4/RJ_FactSheet.pdf. Accessed
August 20, 2019.
7. National Family Health Survey, 2019.
Available from: http://rchiips.org/nfhs/nfhs4.shtml. Accessed
August 20, 2019.
8. Tanigasalam V, Vishnu Bhat B,
Adhisivam B, Balachander B, Kumar H. Hypothermia detection in
low birth weight neonates using a novel bracelet device. J
Matern Fetal Neonatal Med. 2019;32:2653-6.
9. Census of
India Website: SRS Statistical Report 2015. Available from:
http://www.censusindia.gov.in/vital_
statis-tics/SRS_Reports_2015.html. Accessed August 20, 2019.
10. Census of India: Annual Health Survey 2011 - 12 Fact
Sheet. Available from:
http://www.censusindia.gov.in/vital_statistics/AHSBulletins/AHS_Factsheets_2011_12.
html Accessed August 20, 2019.
11. Rehana S, Tarab M,
Dania M, Zohra L, Das J, Bhutta Z. Essential childbirth and
postnatal interventions for improved maternal and neonatal
health. Reproductive health. 2014;11:S3.
12. Kumar V,
Mohanty S, Kumar A, Misra R, Santosham M, Awasthi S, et al.
Effect of community-based behaviour change management on
neonatal mortality in Shivgarh, Uttar Pradesh, India: A
cluster-randomised controlled trial. Lancet.2008;372:1151-62.
|
|
|
 |
|

