|
|
|
Indian Pediatr 2018;55:
341-342 |
 |
Primary
Pleural Inflammatory Pseudotumor in a Child
|
|
Jayalaxmi S Aihole 1,
Hemalatha Lokanath2
and Narendra Babu Munianjinappa1
From Departments of 1Pediatric Surgery and 2Pathology,
IGICH, Bangalore, Karnataka, India.
Correspondence to: Dr Jayalaxmi S Aihole, Assistant Professor,
Department of Pediatric Surgery, IGICH, Bangalore, Karnataka, India.
Email:
[email protected]
Received: March 23, 2017;
Initial review: June 19, 2017;
Accepted: January 29, 2018.
|
Background: Inflammatory pseudo tumor, a rare
non-neoplastic lesion, commonly presents as slow growing solid lesion in
the lung, but many extra-pulmonary locations have been described.
Case characteristics: A 4-year-old girl who presented with
respiratory distress due to massive pleural effusion. Computed
tomography revealed large hypodense non-enhancing lesion in the left
hemi thorax. Surgical exploration revealed large semisolid pleural
collection filled with gelatinous material with normal underlying lung.
Outcome: Histopathology revealed spindle shaped cells with
abundant myxoid stroma. Child recovered after surgery and was
asymptomatic at 5 years follow-up. Message: Primary pleural
inflammatory pseudotumor may be a rare cause of pleural effusion in a
child.
Keywords: Myxomatous tumor, Plasma cell granuloma, Pleural
effusion.
|
|
I
nflammatory pseudotumors are rare non-malignant
lesions; lung is a common site that can cause secondary pleural
effusion. Primary involvement of pleura is extremely rare. We report
primary pleural inflammatory pseudotumor in a child.
Case Report
A 4-year-old girl was referred to our center for
massive pleural effusion. She was treated for left sided empyema 5
months previously, with thoracotomy and decortication. In view of
presence of myxomatous lesion in the pleural cavity, she was referred to
us for further management. At the time of admission, she was febrile and
tachypneic; trachea was shifted to right side with reduced air entry on
left side. In view of previous operative details and recurrence of
pleural effusion, a possibility of neoplastic lesion was considered.
Pleural fluid analysis did not show any malignant cells.
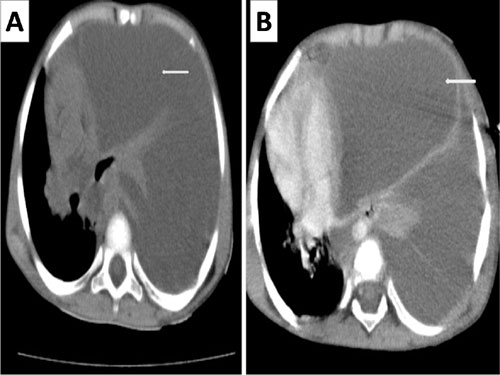
Computed tomography of chest revealed large hypodense,
non-enhancing lesion occupying the entire left hemithorax with collapse
of the underlying lung with mediastinal shift to opposite side (Fig.
1). During thoracotomy, left pleural cavity was found to be
filled with extensive gelatinous, nodular, jelly-like lesion involving
whole of the parietal pleura with partial involvement of visceral
pleura, with normal underlying lung. Evacuation of the jelly like lesion
with partial decortication was performed; post-operative period was
uneventful. Histopathology revealed spindle shaped cells in an abundant
myxoid stroma (Web Fig. 1). The cells exhibited mild
atypia, wavy nuclei and abundant cytoplasm with occasional mitotic
figures (Web Fig. 1). Immuno-histochemistry
revealed myxoid neoplasm positive for vimentin, CK, S100, desmin,
myogenin, and negative for CD117 suggestive of inflammatory pseudotumor
of the pleura. Histopathology of lung tissue was unremarkable (Web
Fig. 1). Patient was doing well at 5 years follow-up.
 |
|
Fig.1 Contrast-enhanced computed
tomography of thorax (mediastinal window) showing large
hypodense non enhancing mass occupying the entire left
hemithorax, causing mediastinal shift to opposite side with
underlying collapsed lung (arrow).
|
Discussion
Inflammatory pseudotumor, also called plasma cell
granuloma, is a rare benign tumor, accounting for 0.7% of all lung
tumors [1,2]. It has a
propensity to clinically and radiologically mimic a malignant disease.
More than one-third of cases are closely related to recurrent
respiratory infections caused by microorganisms such as Mycoplasma,
Nocardia, Actinomycetes, Epstein Barr virus and human herpes virus
[3]. These are most commonly seen in the lung and
orbit, but have been reported from nearly every site in the body.
Primary tumor arising from the pleura is rare, especially in children
and in most cases pleura is involved secondarily [4].
Inflammatory pseudotumor has been reported in all
ages, though less common in children, with slight predominance in
females. Most patients present with nonspecific symptoms, and the tumor
is discovered incidentally on a chest X-ray performed for other
reasons [3]. In our patient,
the initial presentation was like para-pneumonic effusion with fever,
cough and breathlessness, and the patient underwent initial surgery for
suspected empyema. Radiological findings were suggestive of massive
pleural collection with collapse of underlying lung. Our patient had
exclusive pleural involvement, without involving underlying lung
parenchyma or mediastinal structures. Evacuation of gelatinous material
with pluerectomy resulted in complete cure.
Diagnosis of inflammatory pseudotumor is mainly by
histology that is characterized by myofibroblastic spindle cells mixed
with a hyalinized stroma with inflammatory infiltrates. The presence of
abundant myxoid stroma in our patient was unusual.
Surgical excision of the tumor remains the standard
treatment as most tumors are amenable for complete removal. Reports of
recurrence of tumor have been noted as late as 11 years after surgery,
and this highlights the need for long-term follow-up [5]. Other
modalities of treatment include chemotherapy with steroids,
non-steroidal anti-inflammatory drugs, immunomodulation and radiotherapy
[6].
Contributors: JSA: Management of
the patient and writing the Manuscript. HL: histopathological
examination and diagnosis; NBM: patient management and critical inputs
to manuscript writing.
Funding: None; Competing interest:
None stated.
References
1. Umiker WO, Iverson L. Post inflammatory tumor of
the lung: Report of four cases simulating xanthoma, fibroma or plasma
cell granuloma. J Thorac Surg. 1954;28:55-63.
2. Alam M, Morehead RS, Weinstein MH. Dermatomyositis
as a presentation of pulmonary inflammatory pseudotumor. Chest.
2000;117:1793-5.
3. Hammas N, Chbani L, Rami M, Boubbou M, Benmiloud
S, Bouabdellah Y, et al. A rare tumor of the lung: Inflammatory
myofibroblastic tumor. Diagn Pathol. 2012; 7:83.
4. Girdhar A, Singh A, Bajwa A, Shujaat A.
Inflammatory pseudotumor of the pleura. J Bronchology Interv Pulmonol.
2014;21:154-7.
5. Weinberg PB, Bromberg PA, Askin FB. Recurrence of
a plasma cell granuloma 11 years after initial resection. South Med J.
1987;80:519-21.
6. Symon Z, Schneebaum N, Eyal A, Tal S, Rozen V,
Shoenfeld Y, Successful intravenous immunoglobulin therapy for resistant
inflammatory pseudotumor of the orbit. Thyroid. 2005;15:398-9.
|
|
|
 |
|

