|
|
|
Indian Pediatr 2015;52:
297-301 |
 |
Predictors of Myocardial Dysfunction in
Children with Indian Red Scorpion
(Mesobuthus tamulus) Sting Envenomation
|
|
PM Ananda Kumar,
Sriram
Krishnamurthy, Rangan Srinivasaraghavan,
Subramanian Mahadevan
and *KT
Harichandrakumar
From the Departments of Pediatrics and
*Biostatistics, Jawaharlal Institute of Postgraduate Medical Education
and Research (JIPMER), Pondicherry, India
Correspondence to: Dr Subramanian Mahadevan,
Professor, Department of Pediatrics,
JIPMER, Pondicherry 605 006, India.
Email:
[email protected]
Received: September 30, 2014;
Initial review: December 30, 2014;
Accepted: January 29, 2015.
|
Objective: To identify
predictive risk factors for myocardial dysfunction in children with
scorpion sting envenomation and to evaluate the effects of Scorpion
antivenom and prazosin combination therapy on occurrence of myocardial
dysfunction.
Design: Observational.
Setting: Tertiary care hospital in Southern
India.
Participants: 85 children aged <13 years
with scorpion sting envenomation.
Outcome measures: Frequency of myocardial
dysfunction; predictors of myocardial dysfunction.
Results: 24 children (28.2%) developed myocardial
dysfunction. Hypotension at admission (P=0.003) and increased
time (>4h) between sting and administration of appropriate therapy (P=0.001)
were independent predictors of myocardial dysfunction on logistic
regression. Scorpion antivenom plus prazosin combination therapy led to
an increase in cumulative proportion of children without myocardial
dysfunction.
Conclusion: Early (<4 hours) administration of
Scorpion antivenom along with prazosin increases the cumulative
percentage of children not developing myocardial dysfunction.
Keywords: Children, Myocardial dysfunction, Scorpion sting
envenomation, Scorpion antivenom.
|
|
S
corpion sting envenomation is an acute medical
emergency which can be potentially life-threatening in children.
Significant reduction in morbidity and mortality due to scorpion sting
envenomation has been achieved by use of prazosin [1]. Recently,
Scorpion antivenom (SAV) use in children along with prazosin was shown
to accelerate recovery times [2,3]. Having achieved significant
reduction in mortality in scorpion sting envenomation, the need of the
hour is to reduce morbidity due to scorpion sting envenomation, among
which myocardial dysfunction is most important [4]. Identification of
factors that could potentially predict myocardial dysfunction could be
helpful in providing appropriate and timely management, thereby reducing
the morbidity due to the condition. We planned this study to identify
predictors for myocardial dysfunction in children presenting with Indian
red scorpion envenomation, and to study the effect of SAV plus prazosin
combination therapy.
Methods
This prospective observational study was conducted in
the Department of Pediatrics at a tertiary-care health center in
Pondicherry, Southern India, from November 2012 to May 2014. Approval
from the Institute Ethics Committee was obtained prior to the conduct of
the study, and written informed consent was taken from the parents.
Children aged less than 13 years presenting to the
Emergency medical services or outpatient services of the hospital with
features of scorpion sting envenomation or unknown bite with clinical
features consistent with scorpion sting envenomation (local pain,
sweating, priapism, cold extremities etc) were included. The term
‘Definite scorpion sting’ was used when there was history of sting with
features consistent with scorpion sting envenomation, and the bystanders
had seen the red scorpion and brought the killed scorpion for
identification, or identified the same on pictures shown to them. The
term ‘Consistent with scorpion sting’ was used when there was an
unknown bite with features suggestive of Indian red scorpion
envenomation. Myocardial dysfunction was diagnosed when the
following criteria were met: (i) congestive cardiac failure or
cardiomegaly, (ii) hemodynamic compromise that required a
vasopressor ( ł5
µg/kg/min of dobutamine or dopamine), (iii) left ventricular
dysfunction identified by echocardiography without previous
cardiomyopathy, (iv) elevated CPK-MB levels in the blood and (v)
abnormal electrocardiogram [5].
Children were managed as per the existing
departmental protocol for management of scorpion sting envenomation.
Severity of clinical manifestations at the time of arrival to hospital
was categorized between grade 1 to 4 [2,3]. Grade 1 envenomation was
managed with supportive treatment like local anesthetic injection for
acute pain and paracetamol for mild persistent pain. These patients were
observed for 24 hours for any deterioration. Children with Grade 2
envenomation were managed with prazosin (30 µg/kg every 3 hourly), and
monitored in a high dependency unit till resolution of symptoms.
Prazosin was continued until the extremities were warm. Additionally,
SAV was administered at admission (subject to availability) according to
the protocol followed by Bawaskar, et al. [2]. A single 30 mL
dose of monovalent antivenom (Haffkine Biopharma) was added to 100 mL of
normal saline, and infused intravenously over 30 minutes. During
infusions, the patients were closely observed for anaphylaxis or
allergic reactions. Patients with Grade 3 and Grade 4 envenomation
were managed in the Pediatric intensive care unit (PICU). In
addition to prazosin and SAV management was based on other
complications. Myocardial dysfunction was managed with oxygen, and
intravenous dobutamine infusion at the rate of 6-20 µg/kg/min. Pulmonary
edema was managed with oxygen, mechanical ventilation, sodium
nitroprusside intravenous infusion (0.3-5 µg/kg/min) or freshly prepared
sunlight-protected infusion of intravenous nitroglycerine (2-6
µg/kg/min). Encephalopathy was managed with oxygen, mechanical
ventilation, midazolam and/or phenytoin for control of convulsions.
Children with complications were discharged only after they were stable
without drugs for 24 hours. Children who were administered SAV were
observed for a minimum period of 24 hours post-antivenom administration.
The selection of patients for SAV therapy was based on the availability
of SAV in the hospital at that particular point-of-time.
A 12-lead electrocardiogram (ECG) was done in all
patients at admission, and after six hours. In children who developed
myocardial dysfunction, ECG was repeated before discharge.
Echocardiography and serum levels of CPK-MB were done within 24 hours in
all the patients. In patients with grade 3 or grade 4 envenomation,
echocardiography was repeated before discharge.
Clinical and laboratory data that were recorded
included age, gender, time between sting and hospital admission, history
of any medication before admission, and history of vomiting soon after
sting. Blood pressure, heart rate, respiratory rate, and oxygen
saturation were monitored at regular intervals (on admission, at 30
minutes, at 1, 2, 4, 6, 8, 10, 14, 18, and 24 hours). Normal values of
heart rate, respiratory rate, blood pressure and oxygen saturation were
defined based on normative data charts [6]. Children were followed up
till discharge or death. Assuming the frequency of myocardial
dysfunction as 24% [3], degree of variability at 10%, error of 0.05 and
beta error of 0.2, the sample size calculated was 70 children. To allow
for a 20% attrition, we decided to recruit 85 children. Chi-square test
was used for comparing categorical variables and Student t test for
continuous variables between children with or without myocardial
dysfunction. Predictive risk factors for myocardial dysfunction were
determined by logistic regression. Kaplan Meier survival analysis was
used to evaluate the cumulative proportion of children without
myocardial dysfunction in scorpion sting envenomation in children
receiving SAV plus prazosin therapy versus those receiving
prazosin alone. Analysis was done using SPSS (Statistical Package for
the Social Sciences) Version 19.0.
Results
During the study period, 85 children (52 males), aged
less than 13 years with scorpion sting envenomation were admitted. The
mean (SD) age was 5.4 (3.7) years. Half (n=43) of the children
were aged less than 5 yrs. Many children received inappropriate
pre-referral treatment such as steroids, diuretics and anti-histamines (Table
I). Nine children had grade 1 envenomation. Among 76 children
with higher grade of envenomation, 40 received SAV plus prazosin therapy
while 36 received only prazosin. Ten children (25%) developed myocardial
dysfunction in the SAV plus prazosin group, whereas 14 children (48%)
developed myocardial dysfunction in the treatment group receiving
prazosin alone. All children completed treatment and were followed up
until discharge.
TABLE I Baseline Characteristics in Children with Scorpion Sting Envenomation (N=85)
|
Characteristic |
No. (%) |
|
Definite Scorpion sting |
65 (76) |
|
Site of sting |
|
Upper limbs |
32 (37.6) |
|
Lower limbs |
38 (44.7) |
|
Back |
5 (5.8) |
|
Head and neck |
2 (2.3) |
|
Unknown |
8 (9.4) |
|
Admitted within 4 h of sting |
48 (56) |
|
Severity of envenomation at admission
|
|
Grade 1 |
9 (10.5) |
|
Grade 2 |
65 (76.4) |
|
Grade 3 |
9 (10.5) |
|
Grade 4 |
2 (2.3) |
|
Symptoms and signs |
|
Local pain |
67 (78.8) |
|
Vomiting |
59 (69.4) |
|
Sweating |
72 (84.7) |
|
Salivation |
34 (40) |
|
Cold extremities |
76 (89.4) |
|
Priapism |
35 (41.2) |
|
Bradycardia |
8 (9.4) |
|
Tachycardia |
41 (48.2) |
|
Hypotension |
9 (10.6) |
|
Hypertension |
8 (9.4) |
|
Seizures |
3 (3.5) |
|
Echocardiography evidence of LV dysfunction |
24 (28.2) |
|
ECG changes |
36 (42.4) |
Twenty-four (28.2%) children had myocardial
dysfunction secondary to scorpion sting envenomation; 11 of them had the
features at admission. Children who developed myocardial dysfunction (n=24)
had a longer time gap between sting and admission in comparison to those
who did not develop myocardial dysfunction (n=61). In children
who were admitted late (>4 hours) to the hospital, higher proportion of
myocardial dysfunction (79.2%) was detected (Table II).
TABLE II Characteristics of Children With (N=24) or Without (N=61) Myocardial Dysfunction.
|
Characteristic |
Myocardial |
Nomyocardial |
|
dysfunction
(n=24) |
dysfunction
(n=61) |
|
Age <5 years |
10 (41.6%) |
33 (54.1%) |
|
Male gender |
14 (58.3%) |
38 (62.3%) |
|
*Admission within 4 h |
5 (20.9%) |
43 (70.5%) |
|
†$Delay in admission (h) |
5.62 (2.74) |
2.84 (1.74) |
|
#Antihistamine administration |
13 (54.1%) |
28 (45.9%) |
|
#Steroid administration |
9 (37.5%) |
24 (39.3%) |
|
*CPK (Total) ( IU/L) |
1006 (63) |
333 (27) |
|
*CPK MB (IU/L) |
105 (59) |
40 (30) |
|
*Ventilator requirement |
6 (25%) |
0 |
|
Encephalopathy |
1 (4.1%) |
0 |
|
Death |
1 (4.1%) |
0 |
|
All continuous variables are depicted as mean (SD) while all
categorical variables are depicted as n (%) #Received before
admission; $Time between sting and hospital admission; * P =
0.001; † P = 0.012. |
Thirteen of the 65 children, who presented with grade
2 envenomation at admission, deteriorated to grade 3 or grade 4. The
proportion of children deteriorating to higher grades was significantly
more in children receiving prazosin alone as compared to children who
received SAV along with prazosin (11/33 vs 2/32, P=0.006).
In the sub-group where SAV was used (n=40), all the 18 children
who presented within 4 hours of sting, did not develop myocardial
dysfunction after treatment with SAV whereas 10 out of 22 children who
presented after 4 hours of sting developed myocardial dysfunction
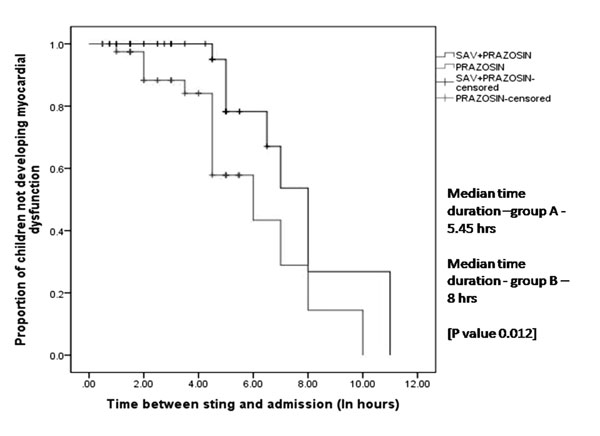
despite treatment with SAV. Kaplan Meier survival analysis showed that
usage of SAV plus prazosin therapy led to an increase in cumulative
proportion of children without myocardial dysfunction (Fig. 1).
 |
|
Fig. 1 Kaplan Meier curve showing
cumulative percentage of subjects not developing myocardial
dysfunction in the two treatment groups: group A (prazosin
therapy alone) and group B (SAV plus prazosin therapy)
(P=0.012).
|
Univariate analysis showed that admission to hospital
more than 4 hours after the sting (P<0.001), hypotension at
admission (P<0.001) and not using SAV in grade 2 envenomation (P<0.006)
were associated with myocardial dysfunction (Table III).
The independent predictors of myocardial dysfunction as determined by
multivariate logistic regression included longer time between sting and
admission, and hypotension (Table IV).
TABLE III Univariate Analysis for Predictors of Myocardial Dysfunction in Children with
Scorpion Envenomation (n=85)
|
Myocardial dysfunction (n=24) |
OR (95% CI)
|
P value
|
|
Age <5 years |
10 |
1.7(0.6 – 4.3) |
0.342 |
|
Male gender |
14 |
2.3(0.9 – 6.1) |
0.736 |
|
Time between sting and admission.>4 hours |
5 |
9.1(2.9 – 28.6) |
0.001 |
|
Hypotension |
8 |
30(3.5 – 258) |
0.001 |
|
Hypertension |
0 |
0.1(0.01 – 2.4) |
0.09 |
|
Received antihistamines prior to admission |
13 |
1.4(0.5 – 3.6) |
0.492 |
|
Received steroids prior to admission |
9 |
0.9(0.4 – 2.5) |
0.875 |
|
Prazosin monotherapy in patients with grade 2 scorpion sting
envenomation at admission |
11 |
7.5(1.3 – 54.8) |
0.006 |
TABLE IV Predictors of Myocardial Dysfunction in Children with Scorpion Sting Envenomation as
Determined by Multivariate Logistic Regression Analysis.
|
Determinants |
Adjusted OR |
P value |
|
(95 % CI) |
|
|
Time between sting and admission > 4 h |
13.8(3.3 – 58.7) |
0.001 |
|
Hypotension |
8.9(3.4 – 36.8) |
0.003 |
|
Treatment with Prazosin without SAV |
2.0(0.1 – 14.4) |
0.160 |
Discussion
The present study demonstrates the beneficial effects
of SAV plus prazosin therapy in prevention of myocardial dysfunction.
Administration of therapy more than 4 hours after the sting, hypotension
at admission and non-usage of SAV for treatment were associated with
myocardial dysfunction in the current study. Although SAV usage in grade
2 envenomation was not found to be an independent predictor of
myocardial dysfunction, therapy with SAV resulted in an increase in the
cumulative proportion of children without myocardial dysfunction.
It has been opined that late administration of SAV
may have no beneficial effect as the venom might have already reached
the target site of action and may not be accessible to the antivenom for
neutralization (due to its short half-life) [7,8]. However, apart from
the action on neutralizing circulating unbound venom, the antivenom also
creates a concentration gradient between plasma and target tissue. The
venom bound to antivenom gets continuously excreted and the toxin in the
tissues moves down the concentration gradient into the blood, where the
redistributed venom is bound by the antivenom. Thus, even if the venom
is not immediately neutralized by antibodies, its removal from tissue
may cause rapid regression of symptoms. This has been proven by in
vitro experimental studies [9-11].
Some other studies have evaluated the risk factors
for adverse outcomes after scorpion sting envenomation, but have not
specifically focused on predictors of myocardial dysfunction. Bouaziz,
et al. [15] documented that age less than 5 years, sweating,
agitation, leukocyosis and elevated plasma proteins were predictors of
pulmonary edema after scorpion sting envenomation. The limitations of
our study include fewer patients with higher grades of envenomation, and
unavailability of ELISA test for detection of venom antigen and
antivenom in the blood. This precluded a correlation between amount of
venom and response to treatment in children who were treated with SAV.
The present study suggests that early appropriate
therapy and referral of patients with scorpion sting envenomation with
autonomic features is vital in preventing myocardial dysfunction, and
optimal treatment with SAV and prazosin combination therapy reduces the
risk of myocardial dysfunction and prevents clinical deterioration in
children presenting with grade 2 envenomations. We recommend similar
adequately powered studies for children presenting with higher grades of
envenomations.
Contributors: PMAK: collected the data,
reviewed the literature and drafted the first version of the manuscript;
SK, RS: reviewed the literature and contributed towards drafting of the
manuscript; SM: conceptualized the study, reviewed the literature and
critically reviewed the manuscript; KTH: performed the statistical
analysis. All authors approved the final version of the manuscript. SM
shall act as guarantor.
Funding: None; Competing interests: None
stated.
|
What is Already Known?
• Scorpion antivenom along with prazosin
accelerates recovery from autonomia dysfunction associated with
scorpion sting envenomation.
What This Study Adds?
• Early (<4 hours) administration of Scorpion
antivenom along with prazosin prevents myocardial dysfunction in
scropion sting envenomation.
|
References
1. Bawaskar HS, Bawaskar PH. Prazosin in management
of cardiovascular manifestations of scorpion sting. Lancet.
1986;1:510-1.
2. Bawaskar HS, Bawaskar PH. Efficacy and safety of
scorpion antivenom plus prazosin compared with prazosin alone for
venomous scorpion (Mesobuthus tamulus) sting: Randomised open
label clinical trial. BMJ. 2011;342:c7136.
3. Pandi K, Krishnamurthy S, Srinivasaraghavan R,
Mahadevan S. Efficacy of scorpion antivenom plus prazosin versus
prazosin alone for Mesobuthus tamulus scorpion sting envenomation in
children: a randomised controlled trial. Arch Dis Child. 2014;99:575-80.
4. Bawaskar HS, Bawaskar PH. Indian red scorpion
envenoming. Indian J Pediatr. 1998;65:383-91.
5. Kumar M, Krishnamurthy S, Delhikumar CG, Narayanan
P, Biswal N, Srinivasan S. Scrub typhus in children at a tertiary
hospital in southern India: clinical profile and complications. J Infect
Public Health. 2012;5:82-8.
6. Kliegman RM, Stanton BF, St Geme JW, Schor NF,
Behrman RE. Nelson Textbook of Pediatrics. 18th edition. Philadelphia:
Saunders Elsevier; 2007. p. 389-91.
7. Boyer LV, Theodorou AA, Berg RA, Mallie J, Arizona
Envenomation Investigators, Chávez-Méndez A, et al. Antivenom for
critically ill children with neurotoxicity from scorpion stings. N Engl
J Med. 2009;360:2090-8.
8. Cupo P, Hering SE. Cardiac troponin I release
after severe scorpion envenoming by Tityusserrulatus. Toxicon.
2002;40:823-30.
9. Ghalim N, El-Hafny B, Sebti F, Heikel J, Lazar N,
Moustanir R, et al. Scorpion envenomation and serotherapy in
Morocco. Am J Trop Med Hyg. 2000;62:277-83.
10. Hammoudi-Triki D, Ferquel E, Robbe-Vincent A, Bon
C, Choumet V, Laraba-Djebari F. Epidemiological data, clinical admission
gradation and biological quantification by ELISA of scorpion
envenomations in Algeria: effect of immunotherapy. Trans R Soc Trop Med
Hyg. 2004;98:240-50.
11. Sevcik C, D’Suze G, Díaz P, Salazar V, Hidalgo C,
Azpúrua H, et al. Modelling Tityus scorpion venom and antivenom
pharmacokinetics. Evidence of active immunoglobulin G’s F(ab’)2
extrusion mechanism from blood to tissues. Toxicon. 2004;44:731-41.
12. Prasad R, Mishra OP, Pandey N, Singh TB. Scorpion
sting envenomation in children: Factors affecting the outcome. Indian J
Pediatr. 2011;78:544-8.
13. Bouaziz M, Bahloul M, Kallel H, Samet M, Ksibi H,
Dammak H, et al. Epidemiological, clinical characteristics and
outcome of severe scorpion envenomation in South Tunisia: Multivariate
analysis of 951 cases. Toxicon. 2008;52:918-26.
14. Bahloul M, Chabchoub I, Chaari A, Chtara K,
Kallel H, Dammak H, et al. Scorpion envenomation among children:
Clinical manifestations and outcome (analysis of 685 cases). Am J Trop
Med Hyg. 2010;83:1084-92.
15. Bouaziz M, Bahloul M, Hergafi L, Kallel H, Chaari
L, Hamida CB, et al. Factors associated with pulmonary edema in
severe scorpion sting patients – A multivariate analysis of 428 cases.
ClinToxicol. 2006;44:293-300.
|
|
|
 |
|

