|
|
|
Indian Pediatr 2021;58:568-571 |
 |
Characteristics and
Transmission Dynamics of COVID-19 in Healthcare Workers in a
Pediatric COVID-Care Hospital in Mumbai
|
|
Ambreen Pandrowala,1
Shaheen Shaikh,2 Mahesh
Balsekar,1 Suverna Kirolkar,2
Soonu Udani3
From Departments of 1Pediatrics, 2Microbiology, and 3Critical Care
and Emergency Services, SRCC Children’s Hospital managed by Narayana
Health, Mumbai, Maharashtra.
Correspondence to: Dr Ambreen Pandrowala, Department of Pediatrics,
SRCC Children’s Hospital, Mahalaxmi,
Mumbai 400 034, India.
Email: [email protected]
Received: December 16, 2020;
Initial review: December 27, 2020;
Accepted: February 06, 2021.
Published online: February 19, 2021;
PII: S097475591600288
|
Objective: To evaluate if Healthcare workers
(HCWs) at the frontline of COVID-19 response in a pediatric hospital are
at an increased risk of acquiring SARS-CoV-2. Methods: The
Hospital Infection Control Committee (HICC) and virology testing records
were combined to identify SARS-CoV-2 positive HCWs and study the
transmission dynamics of COVID-19 over 6 months. Results:
COVID-19 cases in our HCWs cohort rose and declined parallel to
community cases. Forty two out of 534 HCWs (8%) were SARS-CoV-2 positive
with no fatalities. No clinical staff in the special COVID ward or ICU
was positive. Significant proportion of non-clinical staff (30%) were
SARS-CoV-2 positive. About 70% of SARS-CoV-2 positive staff had likely
community acquisition, with a significant proportion having travelled by
public transport or having a contact history with a positive case in the
community. Twenty four percent of positive staff were asymptomatic and
detected positive on re-joining test. Conclusions: Sustained
transmission of SARS-CoV-2 did not occur in our cohort beyond community
transmission. Appropriate PPE use, strict and constantly improving
infection control measures and testing of both clinical and non-clinical
staff were essential methods for restricting transmission amongst HCWs.
Keywords: COVID-19, Healthcare workers, Testing, SARS-CoV-2.
|
|
T
he coronavirus disease
2019 (COVID-19) pandemic started in Wuhan, China in
December, 2019. Nosocomial transmission has been a significant
concern right from the start of the pandemic with one-third of
the initial cohort of COVID-19 patients being healthcare workers
(HCWs) and hospitalized patients [1]. In publications so far,
healthcare workers (HCW) infection rates in China, Italy and USA
have been reported as 3.8%, 10% and 19%, respectively with
fatality up to 1.2% [2].
Union health ministry data shows that the
positivity rate amongst HCWs in Maharashtra was 16%. Mumbai was
one of the first cities significantly affected by the pandemic
in India. Our hospital is a 200-bedded tertiary level pediatric
centre. Healthcare workers showing any symptoms were tested for
SARS-CoV-2 from late March, 2020. All routine work was suspended
and only emergencies were managed from 20 March, 2020, when
Mumbai had recorded 50 cases of COVID-19. Our center was
designated as a pediatric COVID care centre from 6 April, 2020
onwards. The present study was aimed to analyze the
characteristics and transmission dynamics of COVID-19 in HCWs
over first 6 months of the pandemic at a tertiary pediatric
COVID care setup in Mumbai.
METHODS
Any employee who was working in hospital
premises with or without direct patient contact was included as
a HCW. This included individuals employed directly by the
hospital or via a company in contract with the hospital. All
HCWs – both clinical and non-clinical, were tested if any of the
following symptoms were present- fever, cough, sore throat, body
ache, headache, vomiting and diarrhoea; or if re-joining work
after a leave of more than 14 days. Testing was done with a
nasopharyngeal swab for SARS-CoV-2 RT-PCR by an ICMR approved
kit having 99% sensitivity and specificity. Healthcare workers
were encouraged to self-test, if required under supervision to
minimize exposure to other HCWs. Self-collection has been found
to be an appropriate and reliable alternative to HCW collection
[3,4]. Awaiting results, HCWs were sent for home isolation or
quarantined in the hospital staff quarters. Healthcare workers
that tested positive were evaluated by a member of the hospital
infection control committee (HICC) for contact tracing. Those at
high risk exposure (exposure >15 min without mask, less than a
meter distance) were quarantined for 14 days with a repeat
SARS-CoV-2 RTPCR done on day 12 or 13 before re-joining work
[5]. All positive HCWs followed Municipal Corporation of Greater
Mumbai (MCGM) guidelines for home or institutional quarantine
and re-joined work after testing negative for SARS-CoV-2. Once
travel restrictions were lifted, details of travel i.e.;
self-driven vs public transport were documented at the time of
contact tracing. The virology laboratory data of HCWs tested and
HICC team data for category of staff and contact tracing from
March, 2020 to August, 2020 was retrospectively analysed after
approval. Exposure was defined as hospital exposure when there
was contact with a SARS-CoV-2 positive patient or staff in
hospital premises and for individuals working in areas of the
hospital like Emergency room, radiology etc. where exposure to
SARS-CoV-2 unknown status is high, and community exposure was
defined as any HCW who was SARS-CoV-2 positive with history of
exposure to SARS-CoV-2 in the community including family members
and during travel. Exposure was consi-dered likely community
acquired if there was no exposure to SARS-CoV-2 positive or
unknown status patient without breach in social distancing
measures with colleagues. Home leave was defined as leave from
work for more than 14 days and new employees. Hostel exposure
included nurses who were residing in the hostel and also staff
who preferred not going home during the pandemic and were
residing in hospital quarters. Individuals exposed to positive
staff residing in the same room/flat were considered as high
risk exposure.
Personal protective equipment (PPE) donning
and doffing training was carried out for HCWs. PPE use was
decided based on location and risk category as per Ministry of
Health and Family Welfare (MOHFW) guidelines [6]. As the
pandemic progressed and we learnt more about the transmission
dynamics, changes were made to infection control protocols and
staff were briefed about it.
RESULTS
Five hundred and thirty four HCWs were tested
during 6 months with 42 HCWs (8%) positive for SARS-CoV-2
without any fatalities. The monthly incidence of SARS-CoV-2
positivity in HCWs is depicted in Fig. 1. Peak incidence
of cases in Mumbai was seen in June [7]. Cases in HCWs rose and
fell parallel to community incidence.
 |
|
Fig. 1 Healthcare workers tested
Monthly for SARS-CoV-2 in the first six months of
the pandemic.
|
Nurses had the highest incidence of
SARS-CoV-2 positivity; 13 out of 42 (31%) although only 3 out of
13 (23%) had direct high risk patient exposure in the emergency
room and day care unit (Fig. 2). Fourteen percent (6 out
of 42) positive cases were seen in cafeteria and human resource
personnel. Clustering of cases was seen in blood bank and
amongst laboratory technicians. Doctors were least positive in
our cohort (2 out of 42).
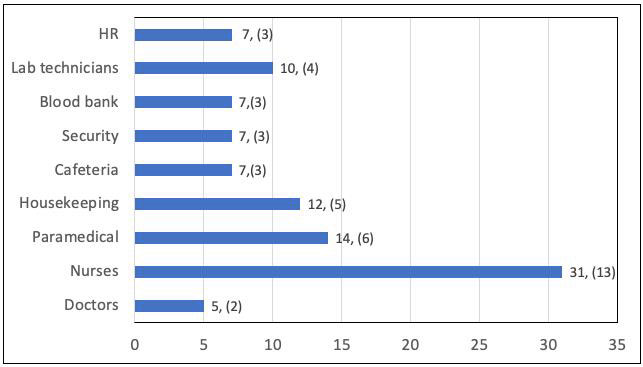
Number of staff positive in brackets. HR-Human resources
personnel
|
|
Fig. 2 Percentage
positivity in the category of staff tested.
|
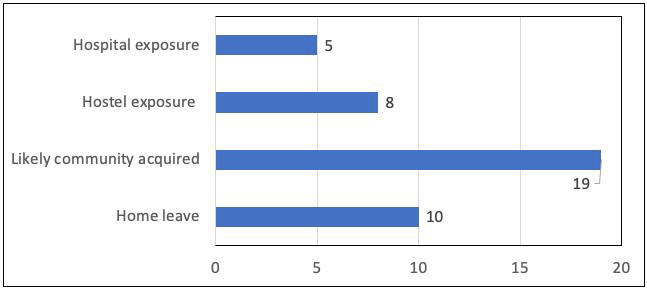
Almost 70% (29 out of 42) of the positive
cases had no high risk exposure in the hospital and were
classified as likely community acquired (Fig. 3). Amongst
high risk exposure areas- day care area, suspected and positive
COVID ward, and COVID ICU had the least SARS-CoV-2 positivity.
No doctor or nursing staff working in COVID wards or ICU tested
positive for SARS-CoV-2. After a nursing staff tested positive
in day care area, PPE used while managing day care patients was
modified with no further cases noted. Two nursing staff working
in the emergency room tested SARS-CoV-2 positive.
 |
|
Fig. 3 Likely source of
SARS-CoV-2 transmission to healthcare workers.
|
Amongst positive staff with likely community
acquired transmission (Fig. 3), 21% (4 out of 19) had
history of SARS-CoV-2 positive contact and 37% (7 out of 19)
travelled by public transport. Nearly one fourth of SARS-CoV-2
positive staff were returning from home leave (10 out of 42) and
almost all were asymptomatic at the time of testing (Fig. 3).
DISCUSSION
The present study analyses the transmission
dynamics of the first HCW cohort from India. In a pediatric
cohort, risk of asymptomatic SARS-CoV-2 carriage is com-pounded
by presence of caregivers. Other risk factors for HCW exposure
include inadequate social distancing between employees and
non-compliance of mask wearing during breaks [8].
Contact tracing for a SARS-CoV-2 positive
HCWs, showed that 2 staff had to be quarantined for having lunch
together. Cafeteria tables were re-arranged to ensure not more
than 2 people could sit at a table at a time at adequate
distance and leaflets emphasising social distancing amongst HCWs
were put up in the staff cafeteria. HCWs were encouraged to have
meals on their own in their respective areas whenever possible,
which was similar to Contejean, et al.
[9]. This significantly reduced the
incidence of high risk exposure amongst HCWs during meals.
Clustering of cases seen in blood bank were considered hospital
acquired as individuals were on same shift and hence in contact.
Zheng, et al. [2] had an incidence of 7.3%
clinical HCWs being SARS-CoV-2 positive and 2.8% of non-clinical
staff. In our cohort, we had similar findings with 2%
non-clinical staff being SARS-CoV-2 positive emphasising the
need of testing non-clinical symptomatic staff (Fig. 2).
Non clinical staff access common areas and testing all staff
groups has key infection control implications. Doctors were
least positive in our cohort.
Twenty percent (8 out of 42) SARS-CoV-2 of
HCWs were positive as a consequence of sharing rooms in the
hostel with a SARS-CoV-2 positive staff despite immediate
isolation of HCWs at symptom onset indicating transmission of
the virus before onset of symptoms. Our findings were similar to
He, et al. [10], who reported that 9% of transmission could
occur 3 days prior to symptom onset and presymptomatic
transmission to be 44%. Nearly one fourth of SARS-CoV-2 positive
staff were returning from home leave and almost all were
asymptomatic at the time of testing. Though highly debatable, we
preferred testing HCWs returning from home leave in view of high
incidence of community transmission during the first few months
of the pandemic. Testing policy on re-joining work was modified
as per community transmission dynamics. HCWs who preferred
travelling by public transport to the hospital had increased
community exposure. Almost 70% of SARS-CoV-2 positive staff had
likely community acquisition with 7 out of 19 (37%) travelling
by public transport and 4 out of 19 (21%) having a contact
history with a positive case in the community.
Implementing infection prevention and control
(IPC) policies can be challenging during a pandemic but in
studies where reinforcement of IPC measures was done, the curve
flattened in HCWs despite ongoing exposure to COVID-19 patients
[8,9].
We improvised infection control measures and
reinforced basic preventive measures throughout the pandemic. In
presence of adequate PPE and good adherence to infection control
practices, nosocomial acquisition or transmission was less
likely, similar to previous reports [2,11]. HCWs face a
significant risk of SARS-CoV-2 exposure while providing care to
suspected or confirmed COVID-19 patients. It is though important
to remember that transmission may occur in non-patient-care
areas while having meals or talking or from the community. Lack
of adequate PPE, inpatients caregivers, high risk departments,
long duty hours and suboptimal hand hygiene have been linked to
COVID-19 infections in HCWs in various studies [12]. Hand
hygiene, inpatient caregivers and duty hours could have
confounded our findings. Doctors tested least positive in our
study which is similar to Zheng, et al. [2]. Doctors in highly
specialized roles who cannot be replaced by other colleagues,
may continue working with mild and non-specific symptoms, which
is a limiting factor in our study too.
Ethics approval: IEC, SRCC-CH; R-202019,
November, 2020.
Contributors: AP, SU: designed the
retrospective study and wrote the manuscript; MB: wrote the
contact tracing guidelines for HCWs; SS, SK: were involved in
testing and tracing positive HCWs. All authors approved the
final version of manuscript, and are accountable for all aspects
related to the study.
Funding: None; Competing interests:
None stated.
|
WHAT THE STUDY ADDS?
• Most SARS-CoV-2 positive healthcare
workers had likely community transmission with public
transport being a possible high-risk exposure.
• Testing nonclinical symptomatic
staff is essential to reduce transmission as they share
common areas.
|
REFERENCES
1. Huang CL, Wang YM, Li XW, et al. Clinical
features of patients infected with 2019 novel coronavirus in
Wuhan, China. Lancet. 2020 [Epub ahead of print]. doi:
10.1016/S0140-6736(20)30183-5.
2. Zheng C, Hafezi-Bakhtiari N, Cooper V, et
al. Character-istics and transmission dynamics of COVID-19 in
health-care workers at a London teaching hospital. J Hosp Infect.
2020;106:325-29.
3. Wehrhahn MC, Robson J, Brown S, et al.
Self-collection: An appropriate alternative during the
SARS-CoV-2 pandemic. J Clin Virol. 2020;128:104417.
4. Rivett L, Sridhar S, Sparkes D, et al.
Screening of health-care workers for SARS-CoV-2 highlights the
role of asymptomatic carriage in COVID-19 transmission. Elife.
2020;9:e58728.
5. MOHFW advisory for managing HCWs working
in COVID and non- COVID areas of the hospital. Accessed May 15,
2020. Available from:https://www.mohfw.gov.in/pdf/Advisoryformanag
ingHealthcareworkersworkingin COVIDandNonCOVID
areasofthehospital.pdf.
6. MOHFW COVID-19: Guidelines on rational use
of Personal Protective Equipment. Available from:
https://www.mohfw.gov.in/pdf/GuidelinesonrationaluseofPerso nal
ProtectiveEquipment.pdf.
7. MCGM stop coronavirus in Mumbai, Daily
updates. Available from: https://stopcoronavirus.mcgm.gov.in.
8. Çelebi G, Piskin N, Çelik Bekleviç A, et
al. Specific risk factors for SARS-CoV-2 transmission among
healthcare workers in a university hospital. Am J Infect
Control. [Epub ahead of print]. 2020:S0196655320307653. doi:
10.1016/j.ajic.2020.07.039
9. Contejean A, Leporrier J, Canoui E, et al.
Comparing dynamics and determinants of SARS-Cov-2 transmissions
among healthcare workers of adult and pediatric settings in
Central Paris. Epidemiology. 2020.doi: 10.1101/2020.
05.19.20106427
10. He X, Lau EHY, Wu P, et al. Temporal
dynamics in viral shedding and transmissibility of COVID-19.
Nat Med 2020. doi: 10.1038/s41591-020-0869-5.
11. Wee LE, Sim XYJ, Conceicao EP, et al.
Containment of COVID-19 cases among healthcare workers: The role
of surveillance, early detection, and outbreak management.
Infect Control Hosp Epidemiol. 2020:1-7. [Epub ahead of
print]
12. Sahu AK, Amrithanand VT, Mathew R, et
al. COVID-19 in health care workers – A systematic review and
meta-analysis. Am J Emerg Med. 2020;38:1727-731.
|
|
|
 |
|

