|
|
|
Indian Pediatr 2021;58:542-547 |
 |
Effectiveness of
Child-To-Child Approach in Preventing Unintentional Childhood
Injuries and Their Consequences: A Non-Randomized
Cluster-Controlled Trial
|
|
Bratati Banerjee, Rupsa Banerjee, GK Ingle, Puneet Mishra, Nandini
Sharma, Suneela Garg
From Department of Community Medicine, Maulana Azad Medical
College, New Delhi.
Correspondence to: Dr Rupsa Banerjee, Senior Consultant,
Community Processes/Comprehensive Primary Health Care Division, National
Health Systems Resource Centre, NIHFW campus, Block F, Munirka, New
Delhi 110 067, New Delhi, India. Email:
[email protected]
Received: May 14, 2020;
Initial review: June 02, 2020;
Accepted: February 16, 2021.
Published online: February 19, 2021;
PII: S097475591600291
Trial registration: CTRI/2018/07/014872
|
Background: Child-to-child approach is an innovative strategy for
preventing and reducing the morbidity and mortality burden of
unintentional childhood injuries.
Objectives: To test effectiveness of
Child-to-child Approach in preventing unintentional childhood injuries
and their consequences.
Study design: Community-based non-randomized
cluster-controlled trial of parallel design.
Participants: 397 children and adolescents.
Intervention: Eldest literate adolescent of
selected families of intervention area were trained on prevention of
injuries. They were to implement the knowledge gained to prevent
injuries in themselves and their younger siblings and also disseminate
this knowledge to other members of their families.
Outcome: Data was collected from both
intervention and control areas during pre- and post-intervention phases
on the magnitude of injuries, time for recovery from injuries, place for
seeking treatment, cost of treatment, knowledge and practice of
participants and their families regarding injuries.
Results: During post-intervention phase, the
intervention group experienced a significant reduction in incidence of
injuries, increased preference for institutional treatment of injuries
and increased knowledge and practice regarding injuries, in com-parison
to its pre-intervention data and data of the control group in
post-intervention phase. Total time for recovery and cost of treatment
for injuries also decreased in intervention group in post-intervention
phase, though differences were not statistically significant.
Conclusion: Child-to-child approach is effective
in reducing childhood injuries, improving choice of place for seeking
treatment, increasing knowledge of participants, improving family
practices regarding prevention of injuries and reducing expenditure on
treatment of childhood injuries.
Key words: Accident, Educational intervention, Prevention,
Trauma.
|
|
With a change in
epidemiological pattern
of disease burden in the population,
injuries are rising and contributing to a
major part of morbidity and mortality in the entire population,
including children. Childhood injury is currently an alarming
problem in the world. Injuries constitute a large proportion of
global burden of childhood death, particularly for older
children in whom it accounts for almost half of the deaths.
Analysis conducted using Global Burden of Diseases data revealed
that unintentional injuries accounted for 18% of the estimated
deaths among children between the ages of 1 and 19 years
globally [1] and 11.2% of total DALY’s lost in all age groups
[2]. Cost incurred by families towards treatment of childhood
injuries is also enormous around the world [3].
Strategies need to be worked out and
implemented for prevention and control of the problem of
unintentional childhood injuries. Child-to-child approach is one
such innovative strategy [4], which has earlier been proved to
be effective in health promotion among children [5-8]. However,
this approach has not been tested for prevention and control of
injuries in children.
The study was conducted with the objective of
assessing the effectiveness of child-to-child approach in
preventing unintentional childhood injuries and their
consequences in terms of time taken for recovery and cost
incurred on treatment.
METHODS
A community based non-randomized
cluster-controlled trial of parallel design was conducted in
rural area of Delhi. The study was approved by the Institutional
Ethics Committee and written informed consent was taken from
heads of the families and consent/assent was taken from all
participants as applicable.
The study area comprised of one intervention
and one control village in North-West Delhi, which were widely
separated from each other with another habitation located in
between, to prevent contamination. The villages for intervention
and control groups were selected by purposive sampling
considering logistic and operational feasibility. The main study
was undertaken from August, 2017 to January, 2019 and comprised
of 7 broad phases – recruitment, pre-intervention, intervention,
reinforcement, washout, post-intervention and
intervention in control group.
For operational purposes, injury was defined
as physical damage to the child’s body, caused unintentionally/accidentally.
‘One injury’ was defined as each injury of a different type or
in different body part occurring in a child, even if occurring
at the same time due to the same cause. ‘One injury event’ was
defined as one child injured at one point of time, even if it
resulted in multiple injuries.
Children and adolescents aged 0-19 years
belonging to families having at least one adolescent and two
younger siblings were included in the study. Mentally deranged
or critically ill participants were excluded from the study.
Consecutive families were selected for wide dissemination of the
message which is the crux of child-to-child approach.
Recruitment was done at the initiation of the study.
Sample size calculation was based on a pilot
study which was conducted in a different part of the study area;
50 children aged 0-19 years with a recall period of 3 months
were evaluated and the incidence of injury was observed as 15%.
Expecting a 5% reduction in incidence of injury after the
intervention and keeping alpha and beta errors at 5% and 20%,
respectively, sample size was estimated as 90 as per the WHO
guidelines [9] for a two-sided hypothesis test for an incidence
rate, when the observations are censored at 4 months. As the
study required more than one child from one family for
implementing child-to-child approach, clustering effect was
likely to occur due to similarity of participants within a
family. Keeping this in view and to adjust for design effect,
calculated sample size was multiplied by a factor of 2, making a
size of 180 children. Since the study required follow-up of 20
months, possibility of non-response/attrition was considered and
hence 10% was added to this and rounded off to final sample size
of 200 participants each in intervention and control group.
Training was given to the eldest adolescents
in the families of intervention area during intervention phase
i.e., January-April, 2018. Eldest adolescents of the families of
the control area were trained after the completion of data
collection in post-intervention phase. Eligible adolescents
were trained on various aspects of injuries and their
prevention. Training included three components: (i) First
aid and cardio-pulmonary resuscitation (CPR) by St. John’s
Ambulance Services of Indian Red Cross Society, (ii) road
safety and traffic rules as collaboration between Delhi Traffic
Police and Hero MotoCorp, Hero Honda and (iii) injury
prevention and immediate care by the research team. In addition,
messages were given regularly to adolescents during home visits
for data collection. At the end of training, the trained
adolescents were each given a module highlighting salient points
covered in the trainings regarding common injuries and their prevention, a first aid kit and a box with child lock for safe
storage of items likely to cause injury. Trained adolescents
were told to be vigilant and thus prevent occurrence of injuries
in themselves and their younger siblings. They were also
encouraged to pass on the knowledge they had gained through
trainings to their adolescent siblings and all adult women in
their families including mothers, aunts, grandmothers, elder
sisters or sisters-in-law. Subsequently, weekly visits were made
and reinforcement of information was done for 2 months
(May-June, 2018), followed by washout period of 2 months
(July-August, 2018). Control group was also visited at similar
frequency and interval, but only general health messages were
given with no special mention regarding injuries.
Data was collected using a pre-tested
semi-structured proforma, during pre- and post-intervention
phases of four months each, in same months of the year,
pre-intervention data being collected during September-December,
2017 and post-intervention data collected during
September-December, 2018. Ongoing data collection regarding
injury events continued during intervention, reinforcement and
washout phases. Each family was visited once a week during data
collection periods and details regarding injuries that had
occurred in the previous week were enquired into. Families were
also given a notebook each and were told to note down the
relevant details which were assessed by the field investigators
at their subsequent weekly visit and cross-checked by
investigators. Data variables included details about injuries
that occurred, time for recovery from the injury, health care
facility availed for treatment and expenditure incurred for
treatment. Expenditure incurred for treatment for all injury
events included doctor’s consul-tation fee, medicines,
investigations, operations, bed charges, expenses for travel and
expenses for accom-panying person. Wage loss was also
considered. For calculating cost of treatment in private sector,
information was taken about amount actually paid for availing
services, while that in government sector included the cost of
medicines, investigations and procedures as calculated on the
basis of rate contract of Delhi Government Central Procurement
Agency for medicines and the amount pres-cribed for
reimbursement for investigations and procedures under Delhi
Government Employees’ Health Scheme. In addition, the field
investigators during their weekly visits distributed medications
for symptomatic treatment under guidance of investigators of
this research.
Prior to the intervention, baseline knowledge
of participants and practice of families as reported by
participants was assessed by interview of adolescents eligible
for training, all other adolescents and all women aged 20 years
and above of the families. Family practice was assessed as
reported by respondents, on two aspects i.e. measures taken for
prevention of injuries and treatment seeking behavior in case of
occurrence of injuries. Each response was scored and the total
knowledge and practice (KAP) score was calculated. Maximum
attainable score was 29 for knowledge, 60 for practice and 89
for total KAP score. Higher score implied better knowledge and
safer practice.
Statistical analysis: Primary
outcome measure was magnitude of injuries, while secondary
outcome measures included time taken for recovery from injuries,
choice of health facility for treatment of injuries, cost for
treatment of injuries, knowledge of participants and practice of
families regarding injuries and their prevention. Comparison was
made between data of intervention and control groups during
pre-intervention phase to establish matching, pre- and
post-intervention phases of intervention group to assess changes
following intervention, and intervention and control groups
during the post-intervention phase to establish that changes
occurred mainly due to the intervention. For all comparisons,
t test for difference between means and z test for
difference between pro-portions were used for quantitative and
qualitative data, respectively. Chi-square test with Yates
correction was done for comparison of health care facility
availed. For comparison of mean and median cost, Mann Whitney U
test and median test were done, respectively. P value of
<0.05 was considered significant.
RESULTS
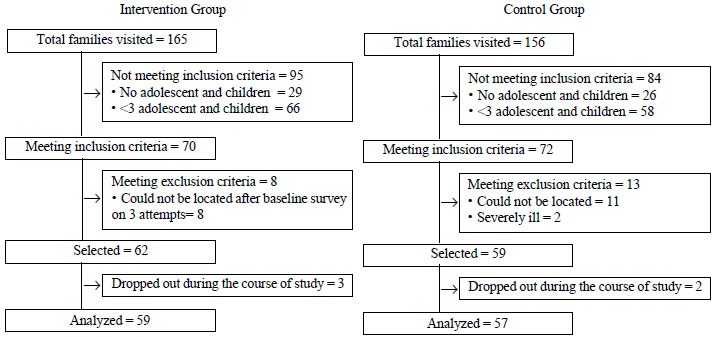
We included 197 and 200 participants each in
the 59 and 57 families, respectively of the intervention and
control groups. Recruitment of participants is shown in Fig.
1. Participants in both the areas were comparable in terms
of sociodemographic profile.
 |
|
Fig. 1 Flow chart showing
recruitment of participants based on eligibility
criteria.
|
Throughout the period of study there was no
fatal injury and none of the injured participants required
hospital admission. Table I shows the incidence of
injuries in the two areas. Annual and monthly incidence of
injury events were calculated as number of injury events
occurring per 100 children per year or month as applicable.
Annual incidence of injury events in the total participants was
32.24 per 100 children per year with average monthly incidence
of 2.69% (2.62 in intervention group and 2.75 in control group),
with no statistically significant difference between the two
groups. In the intervention group, the monthly incidence dropped
significantly in post-intervention phase. Though monthly
incidence had dropped slightly in control area also in the
post-intervention phase, it was still significantly higher than
that in intervention group.
Table I Total Injury Events and Monthly Incidence in the Participants in the Intervention and Control Groups
| Phase of study |
Intervention group (n=197) |
Control group (n=200) |
P value |
Total (N=397) |
| Pre-intervention |
25, 3.17 (0.72-5.6) |
26, 3.25 (0.79-5.7) |
0.86 |
51, 3.21 (1.48-4.9) |
| Post-intervention |
16, 2.03 (0.06-4.0) |
29, 3.62 (1.03-6.2) |
<0.001 |
45, 2.83 (1.2-4.46) |
|
Annual incidents of injuriesa |
62, 31.47 (24.9-37.9) |
66, 33.00 (26.5-39.5) |
0.74 |
128, 32.24 (27.6-36.8) |
| Data expressed as total
injury events, monthly incidence (95% CI). P=0.009 for
pre- and post-intervention periods in intervention group
and P=0.0002 for post-intervention period in
intervention and control groups. aIncludes injuries that
occurred from September, 2017 to August, 2018. |
Table II Type of Health Facility Attended for Treatment of Injury Events
| Type of facility |
Intervention group |
|
|
Control group |
|
Pre-intervention |
Post-intervention |
Pre-intervention |
Post-Intervention |
|
(n=25) |
(n=16) |
(n=26) |
(n=29) |
| Hospital/health centre/clinic |
6 (24.0) |
13 (81.3) |
3 (11.5) |
4 (13.8) |
| RMP/FI/OTC/ home/none |
19 (76.0) |
3 (18.7) |
23 (88.5) |
25 (86.2) |
| Data in no. (%). RMP:
registered medical practitioner; OTC: over the counter. |
The mean time taken for recovery from
injuries in total study participants, which included the total
duration for the wound to heal/ medicines to be stopped/ normal
activities to be resumed (as applicable on a case-to-case
basis), was similar in the two groups in the pre-intervention
phase (P=0.58). Both the intervention group [5.7 (2.4) vs
5.9 (2.9); P=0.79] and control group [7.8 (19.0) vs 7.0
(4.5); P=0.82] did not show any significant differences
in their respective pre- and post-intervention time for
recovery. Total time for recovery from all injuries had reduced
in post-intervention phase in intervention group (143 vs 95
days), while it remained same in control group in both phases
(204 days).
Table II shows the choice of health care
facility by the families for treatment of injuries. Families had
taken treatment from government or private hospital/health
center/clinic, registered medical practitioners (RMP),
over-the-counter treatment by buying medicines from the pharmacy
without consulting a doctor, and home treatment. In the
pre-intervention phase, majority of injured participants in both
groups (>75%) had taken treatment from unqualified providers,
which decreased to 18.1% in the intervention group in
post-intervention phase, in contrast to 86.2% participants in
the control group (P<0.001) (Table II).
The total and the median (IQR) cost of
treatment for injuries in the intervention group decreased from
Rs. 5962.9 to Rs 4949.5, and Rs 90 (102.5) to Rs 19.8 (116.28),
respectively (P=0.84). The corresponding values in
control group were Rs 4734.5 and Rs 7013.4 and Rs. 46.5 (153.75)
and Rs. 40 (135.31), respectively. These differences were
statistically insignificant. The post-intervention median costs
in intervention arm and control arm were comparable.
Table III Knowledge and Practice Scores Regarding Injuries in the Study Groups
|
Intervention group |
|
|
|
|
Control group |
|
No. |
Pre-intervention |
Post-intervention |
No. |
Pre-intervention |
Post-intervention |
| Adolescents for training |
59 |
|
|
57 |
|
|
| Knowledge |
|
8.8 (1.9) |
11.6 (2.6) |
|
9.0 (1.9) |
9.0 (1.6) |
| Practice |
|
39.6 (4.9) |
47.5 (4.8) |
|
37.9 (5.7) |
41.2 (3.7) |
| Total score |
|
48.5 (5.3) |
59.1 (6.4) |
|
46.9 (6.6) |
50.3 (4.2) |
| Other adolescents |
93 |
|
|
81 |
|
|
| Knowledge |
|
7.9 (2.2) |
9.8 (2.3) |
|
8.5 (1.7) |
8.4 (1.4) |
| Practice |
|
38.4 (3.9) |
47.0 (5.2) |
|
37.5 (4.3) |
41.1 (3.8) |
| Total score |
|
46.4 (4.8) |
56.8 (6.5) |
|
46.0 (5.0) |
49.5 (4.2) |
| Adult women |
93 |
|
|
86 |
|
|
| Knowledge |
|
8.0 (1.7) |
10.5 (2.3) |
|
8.2 (1.6) |
8.7 (1.5) |
| Practice |
|
40.4 (4.7) |
48.4 (4.1) |
|
41.4 (4.6) |
44.2 (4.1) |
| Total score |
|
48.5 (5.4) |
58.8 (5.3) |
|
49.6 (5.2) |
52.9 (4.6) |
| Scores expressed as
mean (SD). Data were compared for knowledge scores,
practice scores and total scores for all three groups
viz., adolescent for training, other adolescents and
adult women. For comparison of pre-intervention data of
intervention and control groups, all P>0.05; for pre-
and post-intervention data of intervention group, all
P<0.001; for post-intervention data of
intervention and control groups, all P<0.001. |
Table III depicts the KAP scores of all
three groups of participants. These scores were similar for all
participants during the pre-intervention phase. Mean scores in
all aspects had improved considerably during post-intervention
phase in all participants in the intervention area. Scores had
improved slightly in all groups of control area also. KAP scores
in all groups of participants between pre- and post-intervention
phases in intervention area and between post-intervention phases
in both areas showed statistically significant differences,
indicating dissemination of safety messages.
DISCUSSION
This community based non-randomized
cluster-controlled trial of parallel design was conducted in
rural area of Delhi, to test the effectiveness of child-to-child
approach by training the eldest adolescent members of the
families for preventing unintentional childhood injuries in
themselves and their younger siblings. During post-intervention
phase, the intervention group experienced statistically
significant reduction in incidence of injuries, improvement in
preference for health facilities for seeking treatment, and
increase in knowledge and practice regarding injuries, in
comparison to its pre-intervention data and data of control
group in post-intervention phase. Total time for recovery and
cost of treatment for injuries including out-of-pocket
expenditure also decreased in intervention group in
post-intervention phase, though differences were not
statistically significant.
However, the study had some limitations.
Firstly, a randomized controlled trial could not be done as
study design required consecutive families be included for
dissemination of information and blinding also could not be done
due to obvious reasons. Secondly, the pre- and post-intervention
data collection periods were short due to operational
feasibility. Since data regarding injury and treatment details
was self-reported, these may have been under-reported although
efforts to minimize the same were done by asking participants to
record the events in notebooks which were assessed on a weekly
basis by the research team. Strengths of the study included a
good follow up with an attrition rate of only 4.6%. Frequent
visits by field investigators also resulted in a good rapport-
building and ensured cooperation from the community. A control
group was used that resulted in drawing valid conclusions
regarding outcome. The study groups of both areas at the time of
recruitment were matching in all characteristics of the study
participants and families. Extensive trainings could be given to
the adolescents, two of those being formal trainings from
professional organi-zations. Pre- and post-intervention data
were collected during the same months of the year to rule out
the chance of seasonal variation. Data regarding injuries was
collec-ted by weekly house visits and hence recall period being
very short ensured good quality of data.
Childhood injury is an area of concern in the
entire world, including India. Studies conducted on childhood
injuries in India and abroad have reported various levels of
magnitude [10-20]. Higher annual incidence observed in the
present study was due to weekly active surveillance undertaken
that could capture even minor injuries which are usually
attended at home and hence remain unreported to the health
system. To prevent and control such an alarming problem, various
researchers have reported success of implementing intervention
measures as part of their research on home injury hazards [21],
first aid [5,6], nutrition [7] and health education in general
[8]. Inter-vention in some of these studies was by
implementation of child-to-child approach [5-8]. Though two of
these studies were on improving knowledge regarding injuries and
first aid, there was no study using this approach on injury
pre-vention or cost reduction. Slight decrease in incidence of
injuries and increase in KAP score was obser-ved in the control
area also, probably due to increased awareness through repeated
visits and enquiry regarding injury occurrence.
The present study highlights the need for
introduction of safety education in school curriculum to make
children aware of injuries, their consequences and methods of
prevention. Training on first aid and CPR may be made compulsory
in all schools and colleges, with regular mock drills for injury
management in educational institutions, occupational
institutions and community. Child-to-child program needs to be
implemented by training older adolescents in schools,
encouraging them to take care of their younger siblings at home
and disseminate the messages widely. It can also be implemented
by integrating with other community based health programs and
delivered through primary health care platforms, which will go a
long way in combating the problem of unintentional childhood
injuries in the country.
Acknowledgements: St. John’s Ambulance
Services of Indian Red Cross Society, Delhi Traffic Police and
Hero MotoCorp, Hero Honda, for conducting trainings.
Ethical clearance: Institutional
Ethics Committee, Maulana Azad Medical College; No.
IEC/MAMC/(56)/2/2017/No 74, dated 17 May, 2017.
Contributors: BB contributed to designing
the study, analyzing and interpreting the data, and drafting the
manuscript; RB contributed to analyzing data, and drafting the
manuscript; GKI contributed to designing the study and revising
the manuscript; PM contributed to acquiring and analyzing data;
NS contributed to analyzing data and revising the manuscript; SG
contributed to analyzing data and revising the manuscript. All
authors approved the final manuscript and agreed to be
accountable for the work.
Funding: Indian Council of Medical
Research, New Delhi; Competing interest: None stated.
|
|
WHAT IS ALREADY KNOWN?
•
Implementation of
child-to-child approach is an effective way to improve
awareness of school children regarding unintentional
childhood injury and first aid.
WHAT THIS STUDY ADDS?
•
Child-to-child approach is effective in reducing
number of injury events, total time for recovery from
injuries, cost for treatment of injuries and
out-of-pocket expenses of families, as well as in
improving knowledge of participants and practice of
families regarding injury prevention and control.
|
REFERENCES
1. Alonge O, Hyder AA. Reducing the global
burden of childhood unintentional injuries. Arch Dis Child.
2014; 99:62-9.
2. Murray CJ, Vos T, Lozano R, Naghavi M,
Flaxman AD, Michaud C. Disability-adjusted life years (DALYs)
for 291 diseases and injuries in 21 regions, 1990-2010: A
systematic analysis for the Global Burden of Study 2010. Lancet.
2012;380:2197-223.
3. Lao Z, Gifford M, Dalal K. Economic cost
of childhood unintentional injuries. Int J Prev Med.
2012;3:303-12.
4. Child to child. Our history [Internet].
2019. Accessed on 16 August, 2020. Available from:
http://www.childtochild. org.uk/about/history/
5. Elewa AAA, Saad AM. Effect of child to
child approach educational method on knowledge and practices of
selected ûrst aid measures among primary school children. J Nurs
Educ Pract. 2018;8:69-78.
6. Muneeswari B. A study to assess the
effectiveness of planned health teaching programme using
child-to-child approach on knowledge of selected first aid
measures among school children in selected schools at Dharapuram
in Tamil Nadu, India. Glob J Med Public Health. 2014;3:18.
7. Sajjan J, Kasturiba B, Naik RK, Bharati
PC. Impact of child to child nutrition education intervention on
nutrition knowledge scores and hemoglobin status of rural
adolescent girls. Karnataka J Agric Sci. 2011;24:513-5.
8. Leena KC, D’Souza SJ. Effectiveness of
child to child approach to health education on prevention of
worm infes-tation among children of selected primary schools in
Man-galore. Nitte Univ J Health Science. 2014;4:113-5.
9. Lwanga SK, Lemeshow S. Sample size
determination in health studies: A practical manual. World
Health Organi-zation; 1991. Accessed on 16 August, 2020.
Available from: https://apps.who.int/iris/bitstream/handle/10665/40062/9241544058_%28p1-p22%29.pdf?sequence=1&is
Allowed=y
10. Parmeswaran GG, Kalaivani M, Gupta SK,
Goswami AK, Nongkynrih B. Unintentional childhood injuries in
urban Delhi: A community-based study. Indian J Community Med.
2017;42:8-12.
11. Mathur A, Mehra L, Diwan V, Pathak A.
Unintentional childhood injuries in urban and rural Ujjain,
India: A community-based survey. Children 2018;5:23.
12. Kamal NN. Home unintentional non-fatal
injury among children under 5 years of age in a rural area, El
Minia Governorate, Egypt. J Community Health. 2013;38:873-9.
13. Thein MM, Lee BW, Bun PY. Childhood
injuries in Singa-pore: a community nationwide study. Singapore
Med J. 2005;46:116-21.
14. Lasi S, Rafique G, Peermohamed H.
Childhood injuries in Pakistan: results from two communities. J
Health Popul Nutr. 2010;28:392-8.
15. Howe LD, Huttly SRA, Abramsky T. Risk
factors for injuries in young children in four developing
countries: the Young Lives Study. Trop Med Int Health. 2006;11:
1557-66.
16. Chalageri VH, Suradenapura SP, Nandakumar
BS, Murthy NS. Pattern of child injuries and its economic impact
in Bangalore: a cross-sectional study. National J Community
Medicine. 2016;7:618-23.
17. Mohan D, Kumar A, Varghese M. Childhood
injuries in rural North India. Int J Inj Contr Saf Promot.
2010;17: 45-52.
18. Shriyan P, Prabhu V, Aithal KS, Yadav UN,
Orgochukwu MJ. Profile of unintentional injury among under-five
children in coastal Karnataka, India: A cross-sectional
study.Int J Med Sci Public Health. 2014;3:1317-9.
19. Bhuvaneswari N, Prasuna JG, Goel MK,
Rasania SK. An epidemiological study on home injuries among
children of 0-14 years in South Delhi. Indian J Public Health.
2018;62:4-9.
20. Cameron CM, Spinks AB, Osborne JM, Davey
TM, Sipe N, McClure RJ. Recurrent episodes of injury in
children: an Australian cohort study. Austr Health Rev.
2017;41:485-91.
21. Chandran A, Khan UR, Zia N, et al.
Disseminating childhood home injury risk reduction information
in Pakistan: results from a community-based pilot study. Int J
Environ Res Public Health. 2013;10:1113-24.
|
|
|
 |
|

