|
|
|
Indian Pediatr 2021;58: 517-524 |
 |
Descriptive Epidemiology of Unintentional
Childhood Injuries in India: An ICMR Taskforce Multisite Study
|
|
Shalini C Nooyi, 1 KN
Sonaliya,2 Bhavna Dhingra,3
Rabindra Nath Roy,4 P
Indumathy,5 RK Soni,6
Nithin Kumar,7 Rajesh K
Chudasama,8 Ch Satish Kumar,9
Amit Kumar Singh,10 Venkata
Raghava Mohan11
Nanda Kumar BS1 and ICMR
Taskforce on Childhood Injuries*
From 1Ramaiah Medical College, Bangalore, Karnataka; 2GCS Medical
College, Ahmedabad, Gujarat; 3AIIMS, Bhopal, Madhya Pradesh;
4Burdwan
Medical College, Burdwan, West Bengal; 5Vellalar College for Women,
Erode, Tamil Nadu; 6Dayanand Medical College and Hospital, Ludhiana,
Punjab; 7Kasturba Medical College, Mangalore (Manipal Academy of Higher
Education), Karnataka; 8PDU Medical College, Rajkot, Gujarat;
9SRM
University, Sikkim; 10VCSG Medical College, Srinagar, Uttarakhand; and
11CMC, Vellore, Tamil Nadu. *Full list of co-investigators and task
force members provided as annexure.
Correspondence to: Dr Nanda Kumar Bidare Sastry, MS Ramaiah Medical
College, Bangalore, Karnataka, India.
Email:
[email protected]
Received: November 13, 2020;
Initial review: December 31, 2020;
Accepted: March 31, 2021.
|
|
Background: Children 0-14 years
constitute about 31.4% of Indian population, among whom the magnitude
and risk factors of childhood injuries have not been adequately studied.
Objective: To study the
prevalence of and assess the factors associated with unintentional
injuries among children aged 6 month - 18 years in various regions.
Methodology: This multi-centric,
cross-sectional, community-based study was conducted at 11 sites across
India. States included were Gujarat, Karnataka, Madhya Pradesh, Punjab,
Sikkim, Tamil Nadu, Uttarakhand, and West Bengal between March, 2018 and
September, 2020. A total of 2341 urban and rural households from each
site were selected based on probability proportionate to size. The World
Health Organization (WHO) child injury questionnaire adapted to the
Indian settings was used after validation. Information on injuries was
collected for previous 12 months. Definitions for types (road traffic
accidents, falls, burns, poisoning, drowning, animal-related injuries)
and severity of injuries was adapted from the WHO study. Information was
elicited from parents/primary caregivers. Data were collected
electronically, and handled with a management information system.
Results: In the 25751 households
studied, there were 31020 children aged 6 months - 18 years. A total of
1452 children (66.1% males) had 1535 unintentional injuries (excluding
minor injuries) had occurred in the preceding one year. The overall
prevalence of unintentional injuries excluding minor injuries was 4.7%
(95% CI: 4.4-4.9). The commonest type of injury was fall-related (842,
54.8%) and the least common was drowning (3, 0.2%). Injuries in the home
environment accounted for more than 50% of cases.
Conclusions: The findings of the
study provide inputs for developing a comprehensive child injury
prevention policy in the country. Child safe school with age-appropriate
measures, a safe home environment, and road safety measures for children
should be a three-pronged approach in minimizing the number and the
severity of child injuries both in urban and rural areas.
Keywords: Animal-related injuries, Burns,
Falls, Poisoning, Road traffic injuries.
|
|
G lobally, injuries and violence
are major public health problems. Children are at a higher risk for
injuries due to their physical and psychological attributes. Their small
body size and the softness of tissues lead to greater vulnerability for
severe impact. Children’s risk perception is limited, making them more
susceptible to involvement in road accidents, drowning, burns, and
poisoning. Psychological characteristics of children like impulsiveness,
curiosity, experimentation, an inadequate judgment of distance/speed,
and low levels of concentration make them vulnerable to injuries [1].
The precise number of deaths and injuries due to
specific causes or any reliable estimates of injury deaths in India are
not available from a single source. The National Crime Records Bureau
data and a study based on available data reveal that nearly 10-15% of
India’s injury deaths occur among children [2,3]. An examination of
‘years of potential life lost’ indicates that injuries are the second
most common cause of death after 5 years of age in India [2]. While
there are selected studies related to unintentional childhood injuries
from hospital-based data, the true magnitude of the issue with
population-level determinants is mostly lacking.
This study presents the results of a national level
community-based multi-centric task force study of unintentional
childhood injuries in India, commissioned by the Indian Council of
Medical Research (ICMR).
METHODS
This multi-centric community-based cross-sectional
study was conducted at 11 different sites across eight states in India
between March, 2018 and September, 2020. A purposive selection of study
sites was made, ensuring adequate geographical representation. The study
population comprised children aged six months to <18 years from both
rural and urban areas viz. Siddlaghatta, Bangalore, Karnataka; Pauri
Garhwal, Srinagar, Uttarakhand; Vellore, Tamil Nadu; Perundurai, Erode,
Tamil Nadu; Mangalore, Karnataka; Bardhman Sadar North, Bardhman, West
Bengal; Dhoraji, Rajkot Gujarat; East Sikkim, Sikkim; Dholka, Ahmedabad,
Gujarat; East Ludhiana, Ludhiana, Punjab; Huzur, Bhopal, Madhya Pradesh
(Fig. 1).
 |
 |
|
Fig. 1 Map of India with location of
participating institutions and study sites.
|
Sample size and sampling strategy: The
sample size was calculated considering the overall prevalence of
childhood injuries to be 11.0% (including minor injuries) as per the
guidelines for conducting community surveys on injuries and violence by
WHO [4], with a relative precision of 13% and 95% desired confidence
level, with increase in sample size by 10% to allow for non-responses,
design effect of 2 to account for cluster sampling and relative
precision of 13%. Hence, 2341 households from rural and urban areas
(combined) were selected from each site proportionately based on the
population’s rural-urban distribution as per 2011 census [5]. In each
site, the district predominantly served by the participating institution
was selected. Subsequently, one taluk was selected through a simple
random sampling technique. Applying probability proportionate to size
(PPS) sampling, within each taluk, clusters of households in rural areas
and urban areas were selected. Each cluster consisted of 16 houses
(estimated based on the number of households to be covered by four field
workers in a day) both in urban and rural areas.
Further, within the rural areas, all villages in the
selected taluk were in the sampling frame. In each village, each cluster
consisted of 16 households. The number of clusters to be surveyed to
meet the required sample was arrived at.
In the case of urban areas, one town was selected
using a simple random sampling technique from the total number of towns
in the taluk. Like rural areas, 16 households made up one cluster. The
required number of clusters were selected from a randomly chosen
locality in the town.
The inclusion criterion was to have all six months to
<18-year permanent resident children, and visiting children living in
that area for a minimum duration of previous six months. Additionally,
information pertaining to deaths in the above age group due to
unintentional injuries was sought from the government sources. Birth
injuries or injuries consequent to intra-natal complications, and
disabilities due to other conditions were excluded.
After clearance from the institutional ethics
committee (IEC), permissions were obtained from the district and taluk
administrative authorities at all sites, the zilla panchayat CEO, and
the Child Development Project Officer for accessing information of
village panchayats and community health workers.
Data collection: Each site recruited four field
workers (medico-social workers) who underwent standardized training of 5
days, through a workshop conducted at each site. The workshop oriented
the field investigators to undertake an initial pilot study about child
injuries, the tool, rapport building in the community, data collection
procedures and hands-on instructions on using the electronic handheld
device.
Subsequently, field investigators prepared a spot map
of each selected village (rural area) or locality (urban area) and
numbered the houses serially. After explaining the study’s purpose in
the local language, informed written consent was obtained from the
respondent (parent/primary caregiver). Verbal assent was taken from
children more than or equal to 7 years of age. In addition to
interviewing the adult, children 7 years and above were also interviewed
to substantiate parents’ information. A history of previous three months
was used to collect information relating to all injuries whereas
information about fatal injuries was collected for the previous 12
months and verified in the register maintained in the panchayat office.
At the end of every interview, the caregivers were verbally provided
education regarding injury prevention among children.
Tool employed for data collection: The World
Health Organization (WHO) child injury questionnaire adapted to the
Indian settings was used [4]. Definitions for types (road traffic
accidents, falls, burns, poisoning, drowning, animal-related injuries)
and severity of injuries (mild, moderate and severe) was adapted from
the WHO standard definitions [6]. Injuries other than these types were
categorized as miscellaneous. A cloud-based soft-ware was developed
through an external vendor and validated. Each center received four
handheld devices for the field workers and one for the supervisor.
Quality assurance of data was built into the software with features of
valid entries, skip logic and consistency checks.
A robust management information system and dashboard
was developed through which each site could visualize their respective
electronic data on the web and download a copy of their data. Data were
analyzed centrally based on the approved statistical analysis plan.
Quality assurance: An operation manual and a
training manual for field workers were prepared by the coordinating team
and shared with the participating sites to ensure uniformity. Online
monthly meetings were organized by the central and national coordinating
sites with other site investigators and field workers for centralized
monitoring and supportive guidance to ensure regular interaction and
quality of data collected. The coordinating center continuously
monitored data through the dashboard. A team from the coordinating
center and ICMR team visited each of the sites during data collection
for supportive supervision. The investigators in each site revisited 5%
of households randomly and collected information independently to check
data quality and discrepancies if any, were resolved.
Statistical analyses: Data from all sites
were analyzed by the coordinating team using Statistical Package for the
Social Sciences 16.0 (SPSS Inc.). Data were coded according to severity
of injuries. Minor injuries were excluded for subsequent estimates. The
association between factors such as prevalence rate with age, gender,
and other factors was tested for statistical significance by Chi-square
test or Fisher’s exact test. The difference in mean values between two
groups was tested for statistical significance by Student’s t-test.
Probability value <0.05 was considered as cutoff for statistical
significance. Prevalence rates (period prevalence for 3 months) with 95%
confidence intervals were estimated.
RESULTS
The overall prevalence (95% CI) of unintentional
childhood injuries, including minor and trivial was noted to be 14.5%
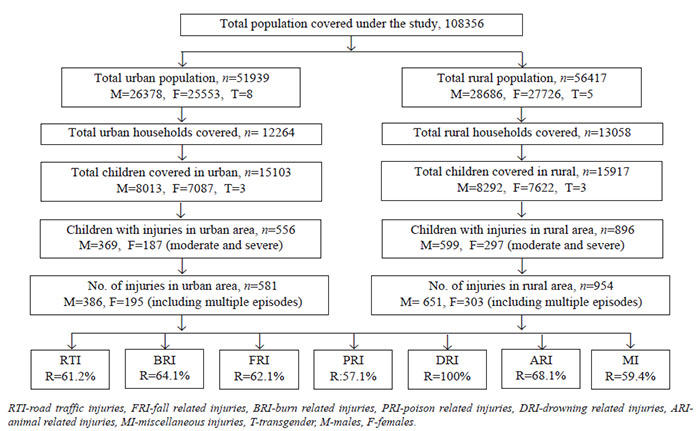
(14.1-14.9). Fig. 2 describes the samples selected and the
distribution of the types of injuries in all sites combined. However,
after excluding minor and trivial injuries, it was noted that 1452
children reported 1535 events of unintentional injuries. The prevalence
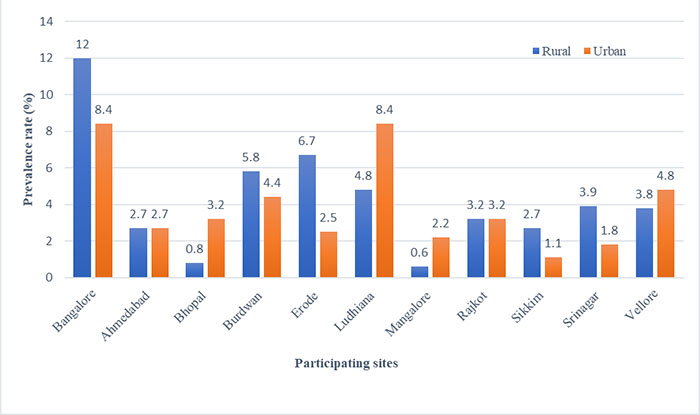
rate of injuries in various sites ranged from 0.6-12.0% (rural areas)
and 1.1-8.4% (urban areas) (Fig. 3). The prevalence was higher
among males as compared to females (5.9% vs 3.3%, P<0.001). The
differences in the prevalence rates between different age groups was
found to be statistically significant (P=0.01), with the lowest
prevalence rate among children below 1 year. The prevalence rate showed
a decreasing trend with increasing socioeconomic status. The difference
in prevalence based on the number of children in the family was minimal
(Table I).
Table I Socio/Demographic Characteristics and Prevalence of Injuries
|
No. of children |
No. with injury |
Prevalence |
|
n=31020 |
n=1452 |
(95% CI) |
| Age group |
|
|
|
| 6 mo - < 1 y |
768 |
2 |
0.3 (0.03-0.9) |
| 1-4 y |
6375 |
266 |
4.2 (3.7-4.7) |
| 5-9 y |
8682 |
449 |
5.2 (4.7-5.7) |
| 10-14 y |
9326 |
471 |
5.1 (4.6-5.5) |
| 15-<18 y |
5869 |
264 |
4.5 (3.9-5.1) |
| Gendera |
|
|
|
| Male |
16305 |
968 |
5.9 (5.5-6.3) |
| Female |
14709 |
484 |
3.3 (3.0-3.6) |
| Area of residence |
|
|
|
| Urban |
15103 |
556 |
3.7 (3.3-4.0) |
| Rural |
15917 |
896 |
5.6 (5.2-6.0) |
| Socioeconomic status |
|
|
|
| Lower |
3879 |
194 |
5.0 (4.3-5.7) |
| Lower middle and Upper lower |
24323 |
1190 |
4.9 (4.8-5.5) |
| Upper middle and Upper |
2818 |
6 |
2.4 (0.8-4.5) |
| Number of children in the family |
|
|
|
| 1-2 |
21313 |
1009 |
4.7 (4.2-5.2) |
| >2 |
9597 |
443 |
4.6 (4.0-5.1) |
| Type of family |
|
|
|
| Nuclear |
19323 |
921 |
4.8 (4.4-5.1) |
| Joint |
6759 |
316 |
4.7 (4.2-5.2) |
| Three generation |
4938 |
215 |
4.3 (3.8-4.9) |
| a6 were transgenders and none of
them had injuries. Comparisons of prevalence rates between
different age group, gender, area of residence, socioeconomic
status, number of children in the family, and type of family
showed all P<0.001. |
 |
|
Fig. 2 Study flow and injury types at all
participating sites (excluding mild/trivial injuries).
|
 |
|
Fig. 3 Site-wise injury prevalence rate
(%) by rural and urban areas.
|
Among the different types of injuries, fall-related
injuries had the highest prevalence rate of 2.7% (95% CI: 2.5-2.9)
followed by road traffic accidents (RTA) (1%; 95% CI: 0.8-1.1). Drowning
related injuries were the least (Table II). As per the World
Health Organization severity grading, burn injuries (44.7%) followed by
fall injuries (30.8%) reported a large number of severe type of
injuries. A total of five fatal injuries were reported across the
different sites (Table III).
Table II Prevalence of Different Types of Injuries (N=31020)
| Type of injury |
Prevalence rate (95% CI) |
| Road traffic injuries, n=304 |
1.0 (0.8-1.1) |
| Falls, n=842 |
2.7 (2.5-2.9) |
| Burns, n=103 |
0.3 (0.2-0.4) |
| Poisoning, n=14 |
0.05 (0.02-0.08) |
| Drowning, n=3 |
0.01 (0-0.03) |
| Animal-related, n= 94 |
0.3 (0.2-0.4) |
| Miscellaneous, n=175 |
0.6 (0.4-0.7) |
Table III Severity of Different Types of Injuries (N=1535)
| Type of injury |
Fatal injury |
Severe injury |
Serious injury |
Major injury |
Moderate injury |
|
n=5 |
n=444 |
n=404 |
n=423 |
n=259 |
| RTI |
1 (0.3) |
76 (25.0) |
81 (26.6) |
95 (31.3) |
51 (16.8) |
| Falls |
1 (0.1) |
259 (30.8) |
224 (26.6) |
20 (19.4) |
151 (17.9) |
| Burns |
1 (0.9) |
46 (44.7) |
32 (31.1) |
20 (19.4) |
4 (3.9) |
| Poisoning |
1 (7.1) |
1 (7.1) |
3 (21.3) |
7 (50.0) |
2 (14.2) |
| Drowning |
0 |
0 |
2 (66.7) |
1 (33.3) |
0 |
| Animal-related |
0 |
15 (15.9) |
20 (21.3) |
39 (41.5) |
20 (21.3) |
| Miscellaneous |
1 (0.6) |
47 (26.9) |
42 (24.0) |
54 (30.9) |
31 (17.7) |
| Values in no. (% of row total).
RTI: road traffic injuries. Classification of injury severity as
per World Health Organization [6]. |
Male children from rural areas in the age group of
5-9 years were commonly involved. The commonest location of injury for
all categories was at home. Age was an important factor associated with
different types of injuries. While road traffic accidents, predominantly
involved rural 10-14 year-old males (61.2%), fall-related injuries were
common among the younger 5-9 year-old children resulting in considerable
impairment (74.8%). However, in case of burn injuries, infants and
toddlers had a higher proportion (45.6%) as compared to their older
counterparts.
More than 80% of respondents with different types of
moderate and higher grades of injuries sought care at private clinics
initially. Most of the respondents reached the facility within one hour
of the occurrence of major injuries. Although activities of daily living
were affected among 88% of children with major injuries, more than 77%
of the children returned to their usual level of activity in a short
time. Less than a quarter of the respondents reported borrowing money
for treatment related to injuries. Although a large proportion of
children with injuries had some disability, most of them were temporary.
Permanent disability was noted in 4.3% in road traffic accidents, 11.8%
in falls, 16.5% in burns, 14.3% in poisoning, 11.7% in animal-related
and 10.3% in miscellaneous injuries.
DISCUSSION
This study was undertaken to obtain the population
estimates of unintentional childhood injures and major factors
associated with them. The all-site prevalence of injury including minor
and trivial was noted to be 14.5%. As per the reports from several
studies done in various parts of India, the prevalence of injury ranges
from 11% to 64% [7-9]. This wide range of prevalence may be attributed
to the variation in the sources of data, definitions used, and selection
criteria for assessing the burden of injuries.
Five deaths due to injuries were reported in one year
of the study recall period (0.16 per 1000 children). According to the
Bangalore Injury Surveillance Program (BISP), the ratio of fatal to
nonfatal injury in children below 18 years was 1:27 and male to female
ratio 3:1 [3]. Lower mortality rate reported in the present study may be
attributed to the poor reporting systems as well as absence of
validation of mortality reports for children below 18 years of age. An
ontological analysis of national programs in India revealed lack of
structured reporting mechanisms for childhood mortality [10].
Occurrence of injury was high among male children
compared to female children (2:1). This could be attributed to the
cultural practice of boys playing more outdoors as compared to girls,
especially in the higher age-groups. Higher prevalence in males was
reported by other studies as well [7, 8]. However, a study done in
Agartala did not find any relation between gender and injury prevalence
[9]. The confounding effect of the socio-cultural factors related to
gender and different activities across various age groups is to be noted
while interpreting the relationship between gender and injuries among
children.
We observed that injuries were more common among
children aged 5-14 years compared to children less than 5 years and 15
years and above, which has also been reported by Peden, et al. [11].
Children younger than 5 years usually have close adult supervision and
children older than 15 are relatively less playful. The age group 5-14
years are associated with independent locomotion with lack of
appreciation of risk of getting injured. Similar results were reported
by two other studies [1,12].
Falls contributed to 55% of injuries and most of them
occurred in the domestic environment. WHO global disease burden report
suggests that in most countries, falls are the most common type of
childhood injury seen in emergency departments, accounting up to 52% of
assessments. In Asia, falls are responsible for 43% of all injuries in
children [13]. Other studies have also reported falls to be the most
common injury which occurs in the home environment [2,7,11,14].
In Bangalore in 2007, 26% of injury deaths were due
to road traffic injuries, 17% due to burns, 13% due to falls, 6% caused
by drowning, and poisoning accounted for 5%. RTAs accounted for 40% of
hospitalizations due to injury. Surveys show that road traffic injuries
are one of the five leading causes of disability among children [2,3].
Burns (6.7% of injuries) were commonly reported due
to electric shock or contact with hot liquids or steam. According to
WHO, fire-related burns are the 11th leading cause of death for children
between the ages of 1-9 years [15]. Children under the age of five years
are at the highest risk of hospitalization from burns [12]. In India,
cooking at floor level and wood fired stoves contribute significantly to
burn injuries. Among older children, carelessness is an important
contributor to burn injuries caused by fireworks [16].
Although this study reports only three cases of
drowning in 5-9-year male children, it remains a health hazard. Fatal
drowning is the 13th cause of death among children. Globally, rate of
death due to drowning is 7.2 per 100000 population among children and
the rate is 6 times higher in low- and middle-income countries compared
to higher income countries [17]. Water storage sumps and ponds require
special attention to make them safe for young children. Poisoning was
reported more in rural areas. Kerosene poisoning is the most common
accidental poisoning among children in India, especially in the age
group of 1-3 years. Most injuries occur due to careless storage and use
of pesticides, insect and mosquito killers, and naphthalene acids [18].
Animal-related injuries were also more common in rural areas and
three-quarters of them were due to dog bites or scratches. The BISP has
reported that 11% of injuries in children were due to animal bites
[3,19]. A large portion of the Indian population live in rural
communities, with likelihood of close contact with animals and hence a
proclivity for animal-related injuries.
Domestic factors like inadequate living conditions,
poor housing, no separate area for washing or cooking, use of smoke
forming fuels, absence of cooking plat-forms, lack of safe storage area,
absence of dedicated recreational area for children are key factors in
the causation of injuries. Inadequate lighting would promote the chances
of accidents at home. These factors are the major cause of falls, burns
and accidental poisonings at home [7].
More than 50% of the children in the present study
had cut injuries and lacerated wounds. In a study on unintentional
injuries in the developing countries [20], cuts/bites and open wounds
(23.9%) were the most common injuries. Bruise/superficial injury and
burns accounted for 15% of all injuries while fracture was responsible
for 19% of the injuries [7]. Another study reported that the most common
physical nature of injury was bruise/superficial injuries (39.3%) and
cut/bite or open wound injuries (35.3%) [12]. Abrasion and contusion
contributed to around 1/3rd of injuries in our study, in contrast to
another study done in Aligarh, which reported superficial injuries among
under-five children and cut injuries among children aged more than 6
years [12].
A longitudinal study using verbal autopsy is helpful
in collecting accurate information on fatal injuries. Logistic problems
led to inability to collect data from all houses in hilly terrains and
during winters and heavy rains. Clusters of 16 houses could not be found
in sparsely populated areas/ hilly terrains and hence there is a need to
develop newer approaches and smaller cluster size in such areas.
The findings of the study point to the facets that
will be needed to formulate a comprehensive child injury prevention
policy in the country. Implementation of the policy should be
underscored at the level of the school and household. Child-safe schools
with age-appropriate measures, a safe home environment and road safety
measures for children should be a three-pronged approach in minimizing
the number and the severity of child injuries. These measures must be
reinforced through adolescent education, by articulating specific
interventions to control risk taking behavior. Focused attention on
‘injury-safe’ rural environments will also curtail the burden of child
injuries.
Acknowledgement: Pankaj Gupta, ICMR, New Delhi.
Kaushal Swaroop S, Kavin Corporation, Bangalore.
Ethical clearance: Institutional Ethics
Committees; Ramaiah Medical College, Bangalore; MSRMC/EC/2018, dated
February 5, 2018; GCS Medical college, Hospital and Research Centre,
Ahmedabad; GCSMC/EC/TRIAL/APPROVE/2018/ 24, dated January 28, 2018;
AIIMS, Bhopal; IHEC-LOP/2018/EF0077, dated January 27, 2018; Vellalar
College for Women, Erode; IEC/VCW/HR/2017/001, dated March 20, 2017;
Kasturba Medical College, Mangalore; IECKMCMLR/03-17/42, dated March 15,
2017; PDU Medical College, Rajkot; PDUMCR/IEC/11097, dated June 16,
2017; SRM university, Sikkim; SRMUS/MS/IEC/2018-01, dated February 10,
2018; VCSG Government Institute of Medical Sciences and Research, Pauri
Garhwal; IEC/VCSGGMSI&R/2018/027, dated January 18, 2018; Christian
Medical College, Vellore; IRB/10648/OBS; April 19, 2017; DMC &
H-Ludhiana, Punjab; IRB/DMC & H XX/2017, and Burdwan Medical College,
West Bengal; IEC/BMCXX/2017.
Contributors: All authors approved the final
version of manuscript and are accountable for all aspects related to the
study.
Funding: Indian Council of Medical Research;
Competing interests: None stated.
Annexure
List of Co-Investigators
Co-investigators from Participating Sites
NS Murthy, Babitha Rajan, Chandrika Rao, Sunil Kumar
BM and Anjana George, Ramaiah Medical College, Bangalore, Karnataka;
Bhavik Rana, Venu Shah and Viral Dave, GCS Medical College,
Ahmedabad, Gujarat; Abhijit Pakhare and Girish Bhatt, AIIMS,
Bhopal, Madhya Pradesh; Prabha Srivastava, Rupali Pitamber Thakur,
Raston Mondal, Somnath Naskar and Sutapa Mandal, Burdwan Medical
College, Burdwan, West Bengal; S Ponne, Vellalar College
for Women, Erode, Tamil Nadu; Siddharth Bhargava, Dayanand
Medical College and Hospital, Ludhiana, Punjab; Bhaskaran
Unnikrishnan, Rekha Thapar, Prasanna Mithra and Ramesh Holla,
Kasturba Medical College (Manipal Academy of Higher Education),
Mangalore, Karnataka; Umed Patel and Vibha Gosaliya, PDU Medical
College, Rajkot, Gujarat; Bhawana Regmi, Ojaswani Dubey and
Praveen Rizal, SRM University, Sikkim; Arjit Kumar and
Janki Bartwal, VCSG Medical College, Srinagar, Garhwal;
Sam Marconi, Anuradha Rose, Jasmin Helan Prasad and Anuradha
Bose, CMC, Vellore, Tamil Nadu.
Co-Investigator ICMR Members
Anju Sinha, Sukanya Sarma and RS Sharma, ICMR, New
Delhi.
ICMR Task-Force subject experts
Devendra Mishra, MAMC, New Delhi; G Gururaj, NIMHANS,
Bangalore, Karnataka; Kiran Aggarwal, Hindu Rao Hospital, New
Delhi; Piyush Gupta, UCMS and GTB Hospital, Delhi; Rakesh
Lodha, AIIMS, New Delhi; YK Sarin, MAMC, New Delhi.
|
WHAT IS ALREADY KNOWN?
• Information on childhood injuries is
largely available from hospital-based studies, with limited
population-based data.
WHAT THIS STUDY ADDS?
• The all-site prevalence of injuries in
children aged <18 years was 14.5% (including minor and trivial
injuries).
• Fall-related injuries were most common (54.8%), and most
injuries occurred in the domestic environment.
|
REFERENCES
1. Dunbar G, Hill R, Lewis V. Children’s attentional
skills and road behavior. J Exp Psychol Appl. 2001;7:227-34.
2. National Crime Record Bureau. Accidental deaths
and suicides in India. 2018.
3. Gururaj G. Injury prevention and care: An
important public health agenda for health, survival and safety of
children. Indian J Pediatr. 2013;80:100-8.
4. World Health Organization. Guidelines for
Conducting Community Surveys on Injuries and Violence. World Health
Organization; 2004.
5. Census of India, 2011. Provisional Population
Totals. New Delhi: Office of the Registrar General and Census
Commissioner. 2011.
6. World Health Organization. International
statistical classification of diseases and related health problems:
Tabular list. World Health Organization; 2004.
7. Majori S, Bonizzato G, Signorelli D, et al.
Epidemiology and prevention of domestic injuries among children in the
Verona area (north-east Italy). Ann. 2002;14:495-502.
8. Mathur A, Mehra L, Diwan V, et al. Unintentional
child-hood injuries in urban and rural Ujjain, India: A comm-unity-based
survey. Children (Basel). 2018;5:23-32.
9. Tripura K, Das R, Datta SS, et al. Prevalence and
manage-ment of domestic injuries among under five children in a peri-urban
area of Agartala, Tripura. Health Agenda. 2015;3:41-5.
10. Nanda Kumar BS, Madhumitha M, Ramaprasad A, et
al. National healthcare programs and policies in India: An ontological
analysis. International Journal of Community Medicine and Public Health.
2017;4:307-13.
11. Peden M, Kayede O, Ozanne-Smith J, et al. World
report on child injury prevention: World Health Organization; 2008-2018.
12. Zaidi SHN, Khan Z, Khalique N. Injury pattern in
children: A population-based study. Indian J Community Health.
2013;25:45-51.
13. Murray CJ, Lopez AD. The global burden of
disease: A comprehensive assessment of mortality and disability from
diseases, injuries, and risk factors in 1990 and projected to 2020:
Summary. World Health Organization; 1996.
14. Parmeswaran GG, Kalaivani M, Gupta SK, et al.
Unintentional childhood injuries in urban Delhi: A community-based
study. Indian J Community Med. 2017;42:8-12.
15. Peden M, Oyegbite K, Ozanne-Smith J, et al. World
report on child injury prevention. World Health Organization; 2009.
16. Bagri N, Saha A, Chandelia S, et al. Fireworks
injuries in children: A prospective study during the festival of lights.
Emerg Med Australas. 2013;25:452-6.
17. Hyder AA, Sugerman DE, Puvanachandra P, et al.
Global childhood unintentional injury surveillance in four cities in
developing countries: A pilot study. Bull World Health Organ.
2009;87:345-52.
18. Pal S, Patra DK, Roy B, et al. Profile of
accidental poisoning in children: Studied at urban based tertiary care
centre. Saudi J Med Pharma Sci. 2019:1110-3.
19. Sudarshan MK, Narayana DHA. Appraisal of
surveillance of human rabies and animal bites in seven states of India.
Indian J Public Health. 2019;63:3-8.
20. Mutto M, Lawoko S, Nansamba C, et al.
Unintentional childhood injury patterns, odds, and outcomes in Kampala
City: An analysis of surveillance data from the National Pediatric
Emergency Unit. J Inj Violence Res. 2011;3:13-8.
|
|
|
 |
|

