After many years of battling
with poliomyelitis, India was finally declared polio-free in 2014 [1].
With an annual birth cohort of 27 million and a total 170 million
children below 5 to be reached in every polio round, this victory was
hard won and was a result of years of concerted efforts led by the
Government of India with strong support of partners and tireless efforts
by the millions of frontline workers [2]. India’s Polio program is a
remarkable public health achievement that overcame programmatic,
economic, social and cultural challenges by constantly innovating and
seeking out-of-the box solutions combined with unrelenting focus and
rigor that allowed the program to reach every child.
One of the innovation and major contributing factors
to the elimination of polio transmission in India was a social
mobilization network (SMNet) managed by UNICEF in the two States with
the highest burden; Uttar Pradesh (UP) and Bihar [3]. West Bengal has a
similar structure that started as an emergency preparedness response in
2011 in wake of the Howrah wild poliovirus (WPV) case.
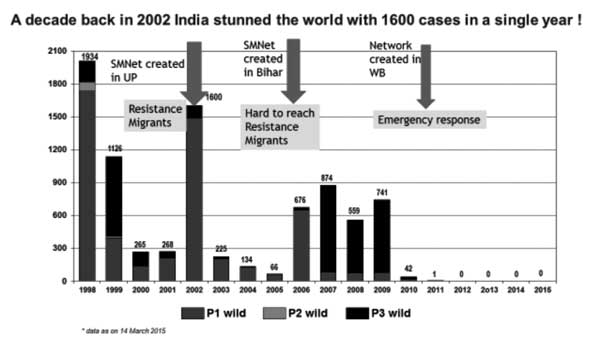
The decision to set up a social mobilization network
had its origins in the analysis of the epidemiological data of wild
poliovirus cases. An unprecedented outbreak in 2002 gave rise to 1600
polio cases. More than 80% of the polio cases in the world were in India
and 86% of WPV cases in India occurred in two States - Uttar Pradesh and
Bihar [4]. Further analysis revealed that over 59% of cases in Uttar
Pradesh belonged to the Muslim community, while according to 2001 census
Muslims comprise approximately 18% of the population in the State [5].
Data showed that a Muslim child was 5 times more likely not to receive
even one dose of OPV [5,6]. Studies and refusal analysis also showed
that there was deep rooted mistrust within the community that resulted
in misconceptions and refusals of OPV. Caregivers also complained about
the lack of trust in the health system and misbehavior of service
providers towards them [5,7,8].
This article is based on a review of primary and
secondary data sources that include SMNet MIS, various researches,
evaluations and technical reports, as well as working papers that
document communication efforts for polio eradication in India. NID/SNID
monitoring data was also reviewed and used. Other sources of information
analysed include country data presented at India Expert Advisory Group
(IEAG) meetings and Polio communi-cation reviews. Reports on Polio
eradication efforts in other countries were also reviewed.
This review examines social mobilization efforts for
polio eradication program in India with following objectives:
• To describe social mobilization strategies and
models which have resulted in polio eradication in India.
• To acknowledge the role of social and community
mobilizers in addressing community resistance and enhancing
community participation for improving public health programmes
through an enabling environment for immunization.
Polio Communication Challenges
The polio eradication campaign initially used a media
heavy approach through celebrity endorsements and branded IEC materials.
In the early stages, mass media was effective in reaching out to the
public - the early and late majority as defined by the Diffusion of
Innovations [9]. But despite the reach of the campaign, some resistant
pockets remained. These pockets tended to be reservoirs of not just
polio viruses but also circulating myths and misconceptions [8].
A social mobilization network was a felt need to
complement the communication activities being undertaken through mass
media channels and use of IEC materials. It was intended that a network
of community based mobilizers could be best suited to counsel and
convince resistant families to accept polio immunization. The mobilizers
had to be persons of trust from within the community who could open
closed doors and were acceptable locally [8].
The Social Mobilization Network (SMNet): Objectives
and Adaptive Models
The SMNet was conceived as a strategic mobilization
ground cadre that used the conventional principles of community
mobilization in an accelerated framework. It was first established in UP
in 2002 and then expanded to Bihar in 2005-06 with the objective of
increasing OPV uptake among children under 5 years of age in these
states. In West Bengal, following the last polio case in 2011, the SMNet
was established for emergency preparedness in response to the wild
poliovirus case in Howrah (Fig. 1) [10].
 |
|
Fig. 1 Wild Polio Virus cases in India
and Social Mobilization Network [10] (Source- GOI/NPSP-WHO Polio
Update).
|
Apart from families that refused immunization, there
were other children who lacked access to services. Belonging to mobile,
migrant and hard to reach families, these were the missing children that
needed to be mapped and brought back into the polio immunization net.
The Social Mobilization Network (SMNet) thus gained shape as a cadre of
mobilizers that could strategically reach out to resistant or left out
families to ensure polio immunization.
Surveillance data were used to systematically map and
identify pockets of underserved and high risk areas/ groups to determine
areas for the SMNet operation. The selection of appropriate advocates
was based on negotiations and discussions with several implementing
partners as well as beneficiaries. The surveillance and supplementary
immunization activity (SIA) data provided case profiles, AFP non polio
cases, X marked houses and houses that reported no eligible children.
For example, a row of 10 or more houses reporting no eligible children
under the age of five were considered suspicious and eligible for
intensified mobilization and advocacy efforts. These were known as P0
(zero) houses, and during monitoring it was often seen that when in
clusters, most houses actually had children in them, indicating a silent
or passive refusal in that the houses did not reject the vaccine
outright but merely claimed to have no children. WHO then modified
monitoring analysis to capture this as a risk area.
In UP, the factors that contributed towards its high
polio burden included poor hygiene and sanitation with high rates of
diarrhea, a dense population with a high birth rate, low uptake of
breastfeeding, and resistance to vaccination among many of the Muslim
communities. Bihar contained pockets of resistance and the same
sanitation and health challenges, but an additional barrier in Bihar was
the difficult geographical terrain (i.e. the Kosi river basin,
which is prone to flooding), which leads to hard-to-reach populations
and migrants, including brick kiln and construction workers, and slum
dwellers [11].
The SMNet deploys community mobilizers in areas
identified as high risk to work with resistant communities and to
encourage uptake of the oral polio vaccine (OPV) during supplementary
immunization activities (SIA). The objectives are to:
• Maximize the impact of communication efforts at
the national state, district and block level through strengthened
coordination amongst partners and effective advocacy.
• Ensure that children most at risk -
particularly those under the age of two, Muslim and boys - are
adequately protected from polio by intensifying efforts in blocks
where wild polio virus (WPV) transmission is sustained.
• Increase the total number of children immunized
and turnout at the booth by achieving a critical mass of
communication activities in all high-risk areas of priority blocks
in states with on-going wild poliovirus transmission.
• Ensure polio eradication by strengthening
communication for routine immunization especially in polio-endemic
states.
Using a three tiered structure, the 7300 strong SMNet
works at district, block and community levels. The community mobilizer
coordinators (CMCs) of the SMNet belong to the communities that they
serve. Responsible for 350-500 households, they go house to house to
engage families through interpersonal communication and counseling
sessions - addressing myths and misconceptions and ensuring correct
knowledge about polio [12,13]. They also mobilize families before every
SIA round to ensure that all children below 5 years get OPV. Holding
mothers’ meetings and religious meetings to advocate for repeated polio
immunization, coordinating temple and mosque announcements and
conducting polio classes in schools, madrasas and other
congregations are just some of the mobilization activities that a CMC
regularly undertakes. In between rounds, they counsel families where
children were missed, tracking pregnant women, registering newborn and
tracking them for polio and routine immunization.
SMNet also includes strong supervisory structures at
block, district, division and state levels. Block mobilization
coordinators (BMCs) are for mentorship and supportive supervision of
CMCs (1 BMC per 10-15 CMCs); District mobilization coordinators (DMCs)
and District undeserved coordinators (DUCs) are responsible for
monitoring district level data and for forming partnerships;
Sub-Regional coordinators (SRCs) provide regional leadership and report
to the state level polio units.
The SMNet also reaches out to community assets to
extend their footprint – an army of 31,000 community influencers to
build trust and goodwill for the polio program while its 26,650
informers help notify movement of migrant communities. [12,13]. Today,
UNICEF’s SMNet reaches over 2.2 million under 5 children in some 3
million households of Uttar Pradesh, Bihar and West Bengal [12, 13].
A. SMNet: Strategies that Delivered Results
SMNet focuses on reaching the most vulnerable,
migrant, mobile, underserved and marginalized children in high risk and
hard to reach communities using a range of strategies in response to the
data and evolving issues:
1. Underserved strategy
The underserved strategy was initially conceptualized
to actively reach Muslim populations and was later expanded from
including Muslim sub-sects to also including hard to reach and migratory
communities who had limited access to information or health services.
These included groups like nomads, brickkiln and construction workers,
slum dwellers etc. This strategy comprises both ground-up community and
social mobilization and a top down advocacy component. Religious leaders
and mosques were actively engaged to disseminate positive information
and address myths. Over 31,000 community influencers are regularly
tapped to build community trust and goodwill for the polio program while
some 26,650 informers help notify movement of migrant communities
[12,13]. These influencers help in mobilization and also accompany
vaccination teams during biphasic/ follow-up activities. Influencers
include religious leaders, doctors, rural medical practioners (RMPs),
shopkeepers and even housewives – each with their own perspectives and
experiences who are able to counsel resistant households for acceptance
[14].
2. Tracking of beneficiaries and high risk groups
WHO and UNICEF jointly identified 400,000 high risk
areas using specific criteria and some 17 indicators [14]. Community
mobilizers track immunization status of all 0-5 years old children and
pregnant women in these high risk areas with special focus on newborns
and guest children. The ‘X’ code used to mark missed households, has
been expanded to allow CMCs to identify the causes for not immunizing a
child. This has allowed a targeted strategy for converting ‘X’
households to households where all children have received OPV in the
current immunization round. CMCs also record information about these
beneficiaries and their immunization status in the field book.
3. Counseling and mobilization activities
CMCs visit every household before the polio round and
provide counseling focussing on previously resistant households. Each
CMC conducts monthly mothers’ meetings, Polio classes in schools,
children’s calling groups (bulwa tolis) and coordinates with
mosques and other institutions for regular announcements. The CMC is
also responsible for display of IEC materials during polio rounds
ensuring high visibility for the program.
4. Evidence based planning at block and district
level
Evidence based planning using real time monitoring
data is used to develop and update house-level microplans for tracking
the immunization progress of every single child. Communication micro
plans are developed at block and district level using evidence generated
through CMCs field book and monitoring data.
5. Capacity building and supportive supervision
The supportive supervisory structure provides
supportive supervision and handholding. These block and district level
mobilizers visit each CMC area on regular basis and mentor them, provide
on job training and jointly solve problems related to their job.
Refresher trainings ensure that the mobilizers are always updated with
the latest tools and techniques.
6. Monitoring and MIS management information
system (MIS)
UNICEF supports a robust monitoring system for polio
communication activities and social mobilization activities using many
indicators by various partners at the local, state and national level to
continually adapt plans and strategies, address bottlenecks and monitor
progress.
7. Strengthening routine immunization and
convergent health issues
The SMNet has been supporting polio end game
strategy, by focusing on routine immunization RI and other convergent
health issues. In addition to the polio messages, the SMNet mobilizers
dovetail convergent child survival messages on routine immunization,
exclusive breast feeding, ORS and zinc and handwashing at critical
times.
B. SMNet: Social Impact
At the core of SMNet lies co-opting the community.
The SMNet uses the members of the community to seed networks with
change. The acceptability of the CMC as she is a part of the community
that she seeks to change is key to the success of the SMNet. In the
context of India, with its socio-cultural complexities, this in itself,
is a mammoth and complex task requiring different approaches for
different groups. The SMNet also triggered sociological changes as
welcome by-products of the polio program and has proved to be an entry
point to larger social and health benefits:
1. Empowering women
Several women, in particular, those from minority or
underprivileged communities gained livelihoods and social confidence
through interacting with community members outside of their initially
circumscribed circumstances. Increased awareness, particularly of health
and hygiene issues has equipped them better not just to improve the
health and well-being of their own families, but also to champion these
in their communities.
2. Empowering children
In the traditional Indian social setup, children
usually do not have agency to act on their own. The SMNet programme,
through its bulawa tolis which co-opts children, has not only
helped them gain their voice, but also established the groundwork and
consciousness for their future participation in similar programs.
3. Mobile and migrant populations
Migrant populations have typically been the toughest
outreach category to access during any program. The SMNet has
established a network of informers conscious of their social
responsibilities and a process that allows migrant families access to
polio vaccines. The network can be further leveraged for several other
uses also – like other healthcare outreach programs, education etc.
4. Religious leaders
SMNet has served to create and intensify a larger
social, public role for religious leaders through their co-option into
the program. This should subsequently, not only broaden their role to
intensify a focus on public health, but also other social good programs
and serve as agencies for repudiating myths that form obstacles to
public health and development programs.
C. SMNet: Results
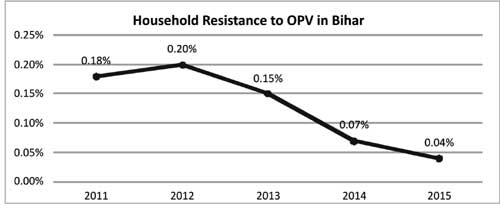
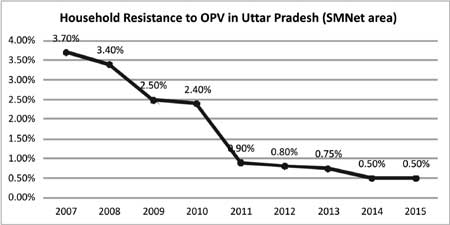
An independent assessment of SMNet in 2013 concluded
that it has been "effective and efficient" at achieving its goals of
increasing the total number of children immunized against polio and
ensuring that those most at risk are protected. Between 2007 and 2015,
resistant households declined 77% in Bihar and 86% in UP, where now less
than 0.5% of households resist vaccination (Fig. 2 and
3) [13,15].
 |
|
Fig. 2 Household resistance to OPV in
Uttar Pradesh (SMNet Area) [13,15].
|
 |
|
Fig. 3 Household resistance to OPV in
Bihar (SMNet Area) [13,15].
|
About 76% of the children less than five years of age
in CMC areas of Uttar Pradesh (no booth activity in Bihar) were
vaccinated at booths in every round, in comparison to this only 43% of
the children vaccinated at booth in non-CMC areas. The average number of
children vaccinated at booth was consistently above 268 in CMC area
almost double of non-CMC areas (148) [16].
Findings and analyses also suggested a high relevance
of the network, SMNet design and interventions are aligned with
community needs. The approach has been relevant to achieve the results
of the polio eradication program by reducing resistance to vaccination
and reaching the unreached in polio endemic states of UP and Bihar.
A value for money (VfM) analysis that was undertaken
in 2014 revealed that SMNet has utilized funds in an economical manner
and has indicated allocative efficiencies. The outputs of SMNet in terms
of coverage and unit costs indicate a cost-efficient and fairly
economical program. Forecasted costs of SMNet for the next decade
support a strong case for continuing eradication interventions as the
most cost-effective option [3].
Analysis of knowledge attitude, behavior and
practices (KABP) through a study for polio eradication, 2009 revealed
that the SMNet has led to consistent and significant increase in
knowledge attitude behaviour practices with the access of communities to
FLWs and CMC visits. (Meta-Analysis of KABP studies showed a strong
linear relationship (Correlation coefficient (r) =0.51 for KA and r=0.90
for BP [17].
D. SMNet: Replication and Similar Programs
The SMNet is already supporting routine immunization
program and other convergent health issues like diarrhea, handwashing
and exclusive breastfeeding – areas that converge with its core
programming. The polio program is naturally transitioning in scope
programmatically, geographically, financially and in its human resources
management. The Indian Government is already applying the polio assets
and learnings in routine immunization (RI) and other convergent
activities. Recognized by the global polio eradication initiative (GPEI)
for its effectiveness, SMNet has been replicated in other Indian states
and polio-endemic countries.
• Vertical health system strengthening model:
In Uttar Pradesh, a parallel outreach system was established to work
alongside and more intensively with government efforts considered
sub-scale (or even non-existent), similar to models applied in parts
of Pakistan, Nigeria and Afghanistan.
• HIV programming: In the context
of the complexities involved in the uptake of intervention services
in HIV prevention, particularly in Asia, social mobilization
evidence has demonstrated that service needs to be driven by people
rather than targets. An example is the shift in focus from "for the
community" to "by the community" the AVAHAN program by the Bill and
Melinda Gates Foundation which has been able to achieve a
significant increase in the uptake of condoms and reduction in STIs
[18].
• Sanitation in Odisha: Engagement with
the treatment villages targeted to increase routine latrine use and
acceptance was done through community mobilization, leveraging a
combination of shaming and subsidy techniques. Findings over the
baseline indicate a significant influence on routine latrine use and
acceptance [19].
• Immunization in Southern Sudan:
In the highly underserved county of Kajo Kenji, an accelerated
immunization program was carried out over three months with the goal
of doubling the county’s immunization coverage of 13% - this, within
a limited budget of USD 6000. In addition to radio spots, each field
supervisor was partnered with one community mobilizer who travelled
to churches, markets, and individual houses to inform the community
about the immunization campaign, using megaphones in some areas.
After the three month acceleration campaign, vaccine coverage
increased to 35.1%, up from 13.8% [20].
Conclusion and Way Forward
The SMNet made significant contributions to India’s
polio eradication by addressing community resistance. The network not
only helped in achieving in an accelerated time line, an impossible task
of interrupting transmission of polioviruses in high risk areas but also
seeded change in the communities. Community mobilizers helped bring
change by being a part of the change process themselves. Community
influencers, religious leaders, teachers, managers and other such
influential groups can be important allies in change. Human resource
management techniques and an ongoing capacity development can lead to
building up of social capital that can be harnessed for social change.
Vertical programs can be successfully expanded to convergent areas once
initial strategic objectives are achieved. And possibly the most
important universal take-away from the SMNet programme is that the
community trust is critical to the success of any behavior change
programs. Externally imposed agencies fail to bring about long term
change without the trust of the community and this trust can be built
only if the members of the network are integral to the community.
Contributors: ARS: conception and design of the
work; drafting the work; PS: drafting few sections; revising it
critically for important intellectual content; GT: drafting few
sections; revising it critically for important intellectual content.
Funding: None. Competing Interest: None
stated.
References
1. Centers for Disease Control and Prevention.
Updates on CDC’s Polio Eradication Efforts. Atlanta: Centers for Disease
Control and Prevention; 2016. Available from:
www.cdc.gov/polio/updates/updates-2016.htm . Accessed January 20,
2016.
2. United Nations Children’s Fund (UNICEF). India’s
story of Triumph over Polio. India: United Nations Children’s Fund
(UNICEF); 2014; 12-13. Available from: www. iple.in/files/ckuploads/files/Polio_Book.pdf.
Accessed February 3, 2016.
3. Deloitte. Evaluation of Social Mobilization
Network (SMNet). India: United Nations Children’s Fund (UNICEF); 2014;
45, 68-81. Available from:
http://www.unicef.org/evaldatabase/files/India_2013-001_Evaluation_of_Social_Mobilization_Network_Final_
Report.pdf. Accessed February 3, 2016.
4. Centers for Disease Control and Prevention.
Morbidity and Mortality Report. Atlanta: Centers for Disease Control and
Prevention; 2003, 52 (09); 172-175. Available from
http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5209a2.htm. Accessed
February 3, 2016.
5. United Nations Children’s Fund. When every child
counts- Engaging the Underserved Communities for Polio Eradication in
Uttar Pradesh, India. Regional Office for South Asia: United Nations
Children’s Fund; 2004. Available from
http://www.unicef.org/rosa/everychild.pdf. Accessed February 3,
2016.
6. India: Ministry of Health and Family Welfare,
World Health Organization-National Polio Surveillance Project. AFP
Surveillance Immunity gap data. New Delhi: Government of India; 2002.
7. Chaturvedi Gitanjali. The Vital Drop –
Communication for Polio Eradication in India. India: SAGE Publication;
2008. 96-8.
8. United Nations Children’s Fund. Critical Leap to
Polio Era-dication. Regional Office for South Asia: United Nations
Children’s Fund; 2003. Available from
www.unicef.org/rosa/critical.pdf. Accessed on February 5, 2016.
9. Everett M. Rogers. Diffusion of Innovations. 5th
ed. New York: The Free Press; 1984.
10. India: Ministry of Health and Family Welfare,
World Health Organization-National Polio Surveillance Project. Polio
Update. New Delhi: Government of India; 2015
11. Grassly N, LaForce M, Modlin J, Murthy N, Rohde
J, Sarma N, et al. Independent Evaluation of Major Barriers to
Interrupting Poliovirus Transmission in India; Report.
http://www.polioeradication.org/ ;2009. Available from:
www.polioeradication.org/content/general/Polio_ Evaluation_IND.pdf.
Accessed February 5, 2016.
12. United Nations Children’s Fund. Communication and
social mobilization to keep India Polio Free. India Country Office:
United Nations Children’s Fund; 2015. Available from:
www.iple.in/documents/download/3557. Accessed February 9, 2016.
13. United Nations Children’s Fund. SMNet MIS. India
Country Office: United Nations Children’s Fund, 2015.
14. United Nations Children’s Fund. Successful
Strategies for Stopping Polio in India-Overview of the key strategies;
India Country Office: United Nations Children’s Fund; 2015. Available
from: www.iple.in/documents/download/3555 . Accessed February 9,
2016.
15. India: Ministry of Health and Family Welfare,
Polio National Immunization Day (NID)/ Sub National Immunization Day
(SNID) data. New Delhi: Government of India; 2007-15.
16. India: Ministry of Health and Family Welfare,
Polio National Immunization Day (NID)/ Sub National Immunization Day
(SNID) data. New Delhi: Government of India; 2015.
17. United Nations Children’s Fund. Concurrent
Knowledge, Attitude, Behaviour and Practices (KABP) Study for Polio
Eradication. India Country Office: United Nations Children’s Fund; 2009.
18. Sarkar S. Community engagement in HIV prevention
in Asia: going from ‘for the community’ to ‘by the community’ – must we
wait for more evidence? Sexually Transmitted Infections, 2010; vol. 86,
no. 1, Available from:
www.uniteforsight.org/social-marketing/social-mobilization. Accessed
July 29, 2015.
19. Pattanayak SK, Yang JC, Dickinson KL, Poulos C,
Patil SR, Mallick RK, et al. Shame or subsidy revisited: social
mobilization for sanitation in Orissa, India. Bull World Health Organ.
2009; vol. 87, no. 8:580-7.
20. Makamba YT. Immunization Activities in
Post-Conflict Settings: Field Notes from Southern Sudan. The Journal of
Global Health. 2011. Available from:
www.ghjournal.org/immunization-activities-in-post-conflict-settings-field-notes-from-southern-sudan/.
Accessed on July 29, 2015.

