|
|
|
Indian Pediatr 2011;48: 379-382 |
 |
Introduction Strategy of a Second Dose Measles
Containing Vaccine in India |
|
Satish Kumar Gupta, Stephen Sosler*, Pradeep Haldar†,
Henri van den Hombergh
and Anindya Sekhar Bose*
UNICEF, New Delhi; *World Health Organization, New Delhi,
India; and, †Ministry of Health and
Family Welfare, New Delhi, India.
Correspondence to: Satish Kumar Gupta, Health Specialist
, UNICEF, 73 Lodi Estate, New Delhi, INDIA.
Email: [email protected]
|
|
Measles continues to be a major cause of
childhood morbidity and mortality in India. Although the true burden of
measles is difficult to quantify, only a small proportion of cases seek
treatment in the formal health sector, infection with measles virus is
ubiquitous throughout the country. A recent review of Indian published
literature shows the median case fatality ratio (CFR) of measles to be
1.63% (range: 0%-30.0%) [1]. Deaths from measles occur mainly in infants
and young children and are primarily due to complications of the infection
such as pneumonia and diarrhea. Malnutrition and young age at infection
are risk factors associated with measles mortality. Recent studies
estimate that 80,000 Indian children die each year due to measles and its
complications amounting to 4% of under-5 deaths [2]. The distribution of
these deaths is not homogenous but is concentrated in states with the
poorest performing immunization programs [3-5].
Global Progress to Reduce Measles Associated Mortality
Remarkable progress has been made globally during the
past 10 years to reduce measles mortality. By 2008, the annual number of
measles associated deaths occurring worldwide had reduced by 78% from
733,000 in 2000 to 164,000 [6]. Sub-Saharan Africa in particular, has
demonstrated the impact of increasing routine vaccine coverage while also
providing a second opportunity for measles vaccination through measles
catch-up campaigns [7]. From 2000 to 2008, measles deaths in Africa
declined by 92%. Progress, however, has not been uniform between countries
or regions of the world. South East Asia disproportionately accounts for
more than three-fourths of the remaining measles deaths globally and the
majority of these are in India. It should be noted that prior to 2010,
India was the only country in the world that had not introduced a second
dose of measles vaccine in its national immunization program [3-5].
Rationale for Second Dose Measles Containing Vaccine (MCV2)
Measles vaccination was introduced into India’s
Universal Immunization Program in 1985. As per national guidelines,
measles vaccine is given to children at 9-12 months of age. Although
coverage with single dose measles vaccine has steadily risen over the
years, it is estimated to be only 70% nationally [8-10], with considerable
variation in coverage both between and within states. The combination of
historically low routine vaccination coverage and primary vaccine failure
(measles vaccine effectiveness is estimated to be 85% when given at 9
months of age) results in a substantial number of susceptible children in
successive birth cohorts which fuels measles virus transmission. A crude
but useful calculation demonstrates the number of susceptible children
that result each year with successive birth cohorts. With 70% routine
measles vaccination coverage and 85% vaccine effectiveness with a single
dose given at 9 months of age, real protection to measles is only 60%
(0.70 × 0.85=0.60) and thus approximately 40% of India’s annual birth
cohort of 26 million children remain susceptible to measles. At this rate,
the accumulation of susceptible children in successive annual birth
cohorts would reach the epidemic threshold level every 2-3 years [11].
 |
|
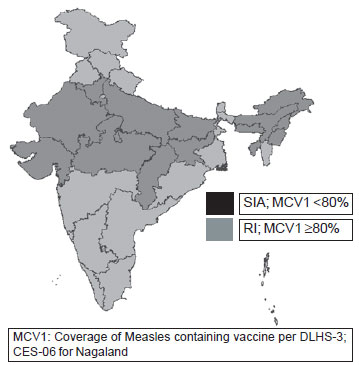
Fig. 1 2nd opportunity of measles vaccine: State specific
delivery strategies.
|
The rationale for providing a second opportunity for
measles vaccination is thus two-fold. The immunological rationale is to
immunize the primary vaccine failures – those children who failed to
respond to the first dose, while the programmatic rationale is to
vaccinate those children who were missed by routine services. Most
children who have failed to respond to the first dose of MCV respond well
to a second dose [12]. MCV2 can be delivered either through existing
routine services or through measles catch-up immunization campaigns, the
choice is determined by the strategy that would attain the highest levels
of coverage. In weak program settings, organized catch-up vaccination
campaigns that benefit from specific planning and intense communication
and coordination efforts have been proven to effectively achieve high
coverage levels in all socio-economic strata [4,6]. Furthermore, numerous
studies from a range of development settings have found two doses of
measles vaccine to be highly cost effective [12]. In settings of low
immunization coverage, the campaign approach has also been found to be
more equitable across wealth quintiles [13].
India’s Decision to Introduce MCV2
Building on global experience and recognizing that
measles represents a significant source of preventable child mortality,
the Government of India announced in May 2010 its decision to implement
the National Technical Advisory Group on Immunization (NTAGI)
recommendation to introduce MCV2 [3,14]. As recommended by the NTAGI, the
implementation strategy of MCV2 at the state level is determined by the
underlying performance of the routine immunization (RI) program. In total,
14 states with measles coverage less than 80% (Arunanchal Pradesh, Assam,
Bihar, Chattisgarh, Gujarat, Haryana, Jharkhand, Madhya Pradesh, Manipur,
Meghalaya, Nagaland, Rajasthan, Tripura and Uttar Pradesh) will introduce
MCV2 through catch-up vaccination campaigns. In the remaining 21 states
with better performing routine immunization systems(i.e.,
≥80%
routine measles coverage) 17 will introduce MCV2 for children aged 16-24
months through the routine program. The remaining four states and union
territories (Delhi, Goa, Puducherry and Sikkim) already use a second dose
of measles vaccine in their RI programme (as mumps-measles-rubella
vaccine) financed with state resources [15].
Measles Catch-up Immunization Campaign
Measles catch-up immunization campaigns benefit from
the extensive experience, human resources and planning templates available
from polio vaccination campaigns. Similar to pulse polio activities,
measles campaigns require meticulous micro-planning, effective vaccine
storage and handling practices as well as appropriate and consistent
advocacy with media, key influencers and social mobilization
interventions.
However, measles is an injectable vaccine and as such,
catch-up campaigns with this vaccine present unique challenges that differ
from polio eradication efforts that utilize oral vaccines. Measles vaccine
must be administered by qualified, trained personnel, the reporting and
management of adverse events following immunization (AEFI) must be
improved and expanded, and the injection waste system should be
sufficiently robust to properly dispose of the large volume of injection
waste to be generated. In addition, measles catch-up vaccination campaigns
target school-aged children with vaccination taking place at schools and
other fixed sites and not door-to-door. This requires strong intersectoral
coordination between the Ministry of Health and Family Welfare, the
Ministry of Education, and the Ministry of Women and Child Development.
Available surveillance data demonstrates that 90% of
confirmed measles cases occurring in outbreak settings in states with low
MCV1 coverage (<80%) are among children less than 10 years of age [5,15].
Hence, measles catch-up campaigns target 134 million children 9 months to
10 years of age in the 14 states (children who have celebrated their 10th
birthday are not eligible), irrespective of previous vaccination status or
measles disease history. The Government of India is providing full
financial support for these activities including the procurement of
vaccine, diluents, injection materials and the operational costs
associated with the human resources, and logistics required to conduct the
3-4 week activity in each state.
As this is a new intervention in India, Government of
India decided to conduct catch-up measles compaign in a phased manner,
with the initial phase targeting 45 districts in 13 states (1 district in
each of the Northeast states of Arunachal Pradesh, Assam, Manipur,
Meghalaya, Nagaland and Tripura, 5 districts in the states of Bihar,
Gujarat, Haryana, Jharkhand, Madhya Pradesh and Rajasthan, and 9 districts
in Chhattisgarh). This approach aims to establish local best practices and
document important lessons learned to be applied during larger subsequent
phases.
Conclusion
The landmark decision to introduce a second opportunity
for measles vaccination is aligned with the draft comprehensive Multi Year
Strategic Immunization Plan of the Government of India (cMYP 2010-2017)
that has among other aims, the target to reduce measles related mortality
by 90% by 2013 compared to 2000 [5,15]. Phase 1 measles catch-up compaign
commenced in November 2010 and will be completed by March 2011. Given the
immunosuppressive impact of measles infection that renders children more
susceptible to secondary pneumonia and diarrheal diseases, the primary
causes of under 5 child mortality in India [16], the provision of MCV2 to
the lowest performing, highest measles burden states will contribute to a
reduction in under-five child mortality and thus provide a needed boost
towards achievement of Millennium Development Goal 4 [17]. Accelerated
measles control remains one of the "best buys" in public health [18].
Competing interests: Authors are staff members of
United Nations Children Fund, World Health Organization* and MoHFW,
Government of India†.
Funding: Nil
References
1. Sudfeld CR, Halsey NA. Measles case fatality ratio
in India: A review of community based studies. Indian Pediatr.
2009;46:983-9.
2. Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I,
Bassani DG, et al. Global, regional, and national causes of child
mortality in 2008: a systematic analysis. Lancet. 2010;375:1969-87.
3. John J, Choudhury P. Accelerating measles control in
India: opportunity and obligation to act now. Indian Pediatr. 2009;46:1-5.
4. van den Ent M, Gupta SK, Hoekstra E. Two doses of
measles vaccine reduce measles deaths. Indian Pediatr. 2009;46:933-8.
5. Strategic pathways for control of measles:
Recommendations of expert consultation 26-28 October 2009. Public health
Foundation of India; New Delhi.
6. Global reductions in measles mortality 2000-2008 and
the risk of measles resurgence. Wkly Epidemiol Rec. 2009;84: 509-16.
7. Progress in global measles control and mortality
reduction, 2000-2006. Wkly Epidemiol Rec. 2007;82:418-24.
8. Coverage Evaluation Survey 2006, All India Report.
New Delhi: UNICEF; 2006. Available at http://www.unicef.org/india/Coverage_Evaluation_Survey_2006.pdf.
Accessed on February 18, 2011.
9. District Level Household Survey, 2007-2008.
Available at http://www.rchiips.org/ARCH-3.html. Accessed on February 17,
2011.
10. World Health Organization, United Nations
Children’s Fund. WHO/UNICEF immunization summary: A statistical reference
containing data through 2009. Available at http://www.childinfo.org/files/32775_
UNICEF.pdf. Accessed February 17, 2011.
11. de Quadros CA, Olive JM, Hersh BS, Strassburg MA,
Henderson DA, Bennett DB, et al. Measles elimination in the
Americas. JAMA. 1996;275:224-9.
12. World Health Organization, Measles vaccines: WHO
position paper. Wkly Epidemiological Rec. 2009; 84: 349-60.
13. Vijayaraghavan M, Martin RM, Sangrujee N, Kimani GN,
Oyombe S, Kalu A, et al. Measles supplemental immunization
activities improve measles vaccine coverage and equity: Evidence from
Kenya, 2002. Health Policy. 2007;83:27-36.
14. Minutes and Recommendations of National Technical
Advisory Group on Immunization (NTAGI), 16th June 2008, Ministry of Health
and Family Welfare, Government of India. Available at http://mohfw.nic.in.
Accessed on 18th February 2011.
15. Measles Catch Up Immunization Campaign- Guidelines
for Planning and Implementation. June 2010 Ministry of Health and Family
Welfare, Government of India.
16. The million death study collaborators. Causes of
neonatal and child mortality in India: a nationally representative
mortality survey. Lancet. 2010;376:1853-60.
17. Millennium Development Goals, Goal 4 Reduce Child
Mortality. Available at http://www.un.org/millennium-goals/childhealth.shtml.
Accessed February 18, 2011.
18. World Health organization, Meeting of the Strategic
Advisory Group of Experts on Immunization, November 2010 – summary,
conclusions and recommendations. Wkly Epidemiol Rec. 2011;86:1-16.
|
|
|
 |
|

