|
|
|
Indian Pediatr 2017;54: 105 -111 |
 |
Sunlight Exposure and Vitamin D Status in
Breastfed Infants
|
|
Pinky Meena, Aashima Dabas, Dheeraj Shah,
#Rajeev Kumar Malhotra,
*SV Madhu and Piyush Gupta
From the Departments of Pediatrics, #Biostatistics
and Medical Informatics, and *Medicine (Division of
Endocrinology); University College of Medical Sciences and Guru Teg
Bahadur Hospital, Dilshad Garden, Delhi, India.
Correspondence to: Dr Piyush Gupta, Professor of
Pediatrics, University College of Medical Sciences and GTB Hospital,
Dilshad Garden, Delhi 110 095, India.
Email:
[email protected]
Received: July 18, 2016;
Initial review: August 31, 2016;
Accepted: November 30, 2016.
Published online: December 05, 2016.
PII:S097475591600032
|
Objective: To correlate the
sunlight exposure in first 6 months to vitamin D status at 6 months of
age in predominantly breastfed infants; and to quantify the sunlight
exposure required to achieve serum 25(OH)D level >20 ng/mL, by 6 months
of age
Design: Prospective cohort.
Setting: Tertiary-care hospital
predominantly catering to urban poor population in Delhi.
Participants: 132 healthy
infants, delivered at term, and predominantly breastfed were enrolled at
6-8 weeks of age. Of these, 100 infants were available for final
evaluation at 6 months of age (mean (SD) follow-up: 126 (17) days).
Methods: Baseline maternal
vitamin D (serum 25(OH)D) levels were obtained at enrolment. The mothers
were asked to maintain a daily record of duration of sunlight exposure,
timing of exposure, and body surface area exposed, for the infant, on a
pre-designed proforma, till the child was 6 months of age. Infant’s
serum 25(OH)D was measured at 6 months of age.
Main outcome measures: Cumulative
Sun Index was calculated as a composite measure of overall
duration/time/body surface area exposed to sunlight; and correlated with
the infant serum 25(OH)D after adjusting for baseline maternal serum
25(OH)D levels, season of exposure, and skin color of the infant. Sun
index for exposure in morning (before 10 am) and afternoon (10 am-3 pm)
were also correlated to vitamin D status.
Results: Of 100 mother-infant
pairs completing the study, 90 mothers had vitamin D deficiency (serum
25(OH)D <12 ng/mL). The median duration of exposure of infants to
sunlight was 17 min per week, on 6% of body surface area. Vitamin D
levels of 67 (67%) infants at 6 months were less than 12 ng/mL and
another 23% had insufficient levels (12-20 ng/mL). Cumulative sun index
correlated positively to infant’s serum 25(OH)D level at 6 months of age
(r= 0.461, P<0.001). Increment in afternoon sun index by 1
unit increased the serum 25(OH)D level by 1.07 ng/mL (95% CI 0.37, 1.78;
P= 0.003). A minimum 30 minute weekly afternoon sunlight
exposure, between 10 am and 3 pm, over 40% body area (infant clothed in
diapers, in prone position) for at least 16 weeks, was estimated
requirement to achieve sufficient vitamin D levels (>20 ng/mL) by 6
months of age.
Conclusions: There is a
significant positive correlation between afternoon sunlight exposure and
infant’s vitamin D levels, independent of maternal vitamin D status.
Randomized controlled trials are suggested to explore the effectiveness
of this simple intervention to prevent or treat vitamin D deficiency in
children.
Keywords: Sun index, Rickets, Treatment,
Vitamin D deficiency.
|
|
V
itamin D deficiency has emerged as a pandemic
affecting all ages including infants [1]. The prevalence of vitamin D
deficiency in Indian neonates is reported between 86 to 100% [2],
despite adequate availability of sunlight and adequate maternal calcium
intake during antenatal period. The sources of vitamin D for infants
include cutaneous vitamin D production and breastmilk, with the later
usually deficient in vitamin D. Natural vitamin D synthesis remains
ineffective mostly due to modern lifestyle where infants remain confined
indoors during daytime, which is the prime time for exposure to
ultraviolet B rays [1]. Therefore, the American Academy of Pediatrics
recommends routine supplementation of vitamin D (400 IU daily) to all
infants till 1 year of age [5].
It is not clear whether vitamin D deficiency in
Indian infants is due to lack of exposure to sunlight or some other
factors also play a role. Genetic polymorphisms of vitamin D receptor
and high melanin content of skin may influence the cutaneous production
of vitamin D in Indian infants [6,7]. We conducted this study to
ascertain whether any correlation exists between sunlight exposure and
vitamin D in Indian infants, and if yes, how much of sunlight exposure
is required to achieve sufficient serum 25(OH)D levels (> 20 ng/mL) [8]
by 6 months of age.
Methods
This prospective observational study was conducted in
the Department of Pediatrics and Division of Endocrinology, Department
of Medicine, University College of Medical Sciences and GTB Hospital,
Delhi after approval from the Ethical Committee of the Institute and
obtaining written informed consent from the caregivers.
We enrolled predominantly breastfed, healthy infants
aged 6-8 weeks, born at term, from the immunization clinic of our
hospital. Only those born in a health facility with documented birth
weight and gestation record were included. Low birth weight (birth
weight <2500 g), small for gestational age infants, and NICU graduates
were excluded. Infants with congenital malformations, history of
seizures, clinical evidence of rickets, chronic systemic disorders, past
hospitalization, history of receiving calcium or vitamin D supplements
were also excluded. We also excluded infants born to mothers who had
received supplemental vitamin D (in excess of 1000 IU/day) in antenatal
or postpartum period. Children with a skin disorder such as ichthyosis
or atopic dermatitis or any other condition where topical drug was
applied were also excluded.
The delivery details of the infant – birth weight,
gestational age, and mode of delivery – were noted from the birth
record. Age at enrolment was calculated (in days), from the date of
birth record. Mothers were asked to provide complete details of intake
of calcium/other supplements during antenatal/postnatal period. Weight
and length of all infants were recorded at enrolment, as per standard
techniques. The baby’s skin color was graded according to Fitzpatrick
skin color scale [9]. The season of enrolment was stratified into (a)
March to May, and (b) June to August.
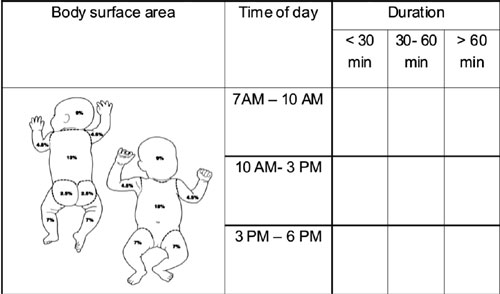
Mothers were asked to maintain a weekly chart to
quantify sunlight exposure. The Lund and Browder Chart [10] was provided
to the mothers to mark all areas that were exposed to sunlight in the
day. The marking was done daily with mention of exact duration (minutes)
and timing (as per clock time) of sun exposure in the performa (Fig.
1). Data of one week were recorded on one sheet. Mothers were
provided with 6 such sheets at a time. The filled performa were
collected from them at 2.5 mo, 3.5 mo, 4.5 mo, and 6 months of age.
Compliance to fill the forms was ensured telephonically on a weekly
basis. The mothers were also counseled to continue exclusive
breastfeeding.
 |
|
Fig. 1 Performa for
documentation of sun exposure in infants.
|
At enrolment, 3 mL of maternal venous blood sample
was collected for estimation of serum 25 hydroxy-vitamin D [25(OH)D].
The venous sample from the infant for estimation of serum 25(OH)D was
obtained at the end of study, at 6 months of age. All samples for
25(OH)D were centrifuged and the sera were stored in a deep freeze at
–20ºC. Serum 25(OH)D was estimated by radioimmunoassay (RIA) with kits
manufactured by DiaSorin, USA (interassay variation: 11%; intra-assay
variation: 12.5%; sensitivity: at or below 1.5 ng/mL). Serum 25(OH)D
values were interpreted as per the following cutoffs – sufficient
³20ng/mL,
insufficient 12-20 ng/mL, and deficient <12 ng/mL [8].
Previous studies [11,12] showed the correlation
between sunlight exposure and vitamin D levels to be around 0.34. For
testing the significant correlation over null correlation taken as 0.1
with 80% power and 95% confidence level (one-sided: r a>r0),
a sample of 98 subjects was sufficient. Adding 30% as follow-up loss
during the follow-up study period, 130 healthy infants were needed to be
enrolled for this study.
Statistical analysis: The data were entered in an
Excel sheet. For each participant, total duration of sun exposure
(minutes) was calculated for the whole day and also separately for
morning hours (before 10 am), and afternoon hours (10 am to 3 pm). Based
on the weekly duration of exposure and skin area exposed to sunlight,
sun index was calculated for each infant as cumulative sun index (for
the whole day exposure), morning sun index (for exposure before 10 am),
and afternoon sun index (exposure between 10 am – 3 pm); as per the
following formula [11]:
Sun index = (minutes of sun exposure per week) ×
(fraction of body surface area (BSA) exposed to sunlight)
Normality of continuous data was checked using
skewness and kurtosis test. The strength of correlation between sun
index and infant’s serum 25(OH)D levels was quantified by
Spearman/Pearson correlation depending upon the distribution pattern.
Multiple linear regression using ‘Enter’ method was performed with
infants’ serum 25(OH)D level as the dependent variable. Independent
variables included cumulative sun index, maternal serum 25(OH)D level,
season during which exposure occurred, skin color of the infant, and
maternal antenatal calcium intake [Model 1]. The analysis was repeated
with morning sun index [Model 2] and afternoon sun index [Model 3],
replacing the cumulative sun index in the Model 1. The models were aimed
at identifying the independent variable that best predicted the infant’s
vitamin D status. Based on the results, the duration of sunlight
exposure and body surface area of exposure required to achieve
sufficient levels of vitamin D (>20 ng/mL) was calculated. Normality of
model residuals was tested using skewness and kurtosis test. Data were
analyzed using IBM SPSS version 20 statistical software.
Results
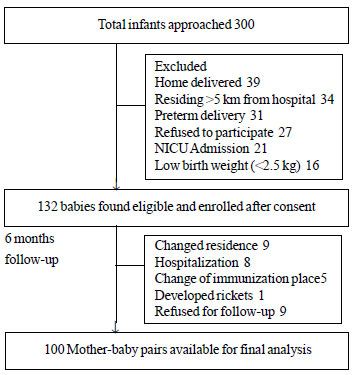
Of 300 infants approached, 132 fulfilled the
inclusion criteria and were enroled between March to August 2015. A
total 100 mother-baby pairs completed the 6 months follow-up (Fig.
2). Of these, 90 mothers had vitamin D deficiency (serum 25(OH)D
<12 ng/mL). Table I compares the baseline characteristics
of the infants who completed the study and those who were lost to
follow-up. Infants who were lost to follow-up were older and had better
anthropometric indices than those who completed the study. The duration
of maternal calcium intake was less among those lost to follow-up
without any difference in maternal serum vitamin D as compared to the
former group. Of children who completed the study, 50 were enroled
between March to May 2015 (exposed to sun between March to October 2015)
and the rest 50 between June to August 2015 (exposed to sun between June
2015 and January 2016).
TABLE I Baseline Characteristics of Study Population
Parameter
|
Infants completed study (n=100) |
Infants lost to follow up (n=32) |
P value
|
|
Age (d) |
48 (46-52) |
51 (50-56) |
0.001 |
|
Parity |
2 (1-2) |
2 (1-2.8) |
0.12 |
|
Gestation (wks) |
39 (38-40) |
38 (38-40) |
0.34 |
|
Birth weight (kg) |
2.8 (2.5-3.0) |
2.8 (2.6-2.8) |
0.78 |
|
Anthropometric characteristics* |
|
|
|
|
Weight (kg) |
4.2 (3.8-4.5) |
4.8 (4.6-5.0) |
<0.001 |
|
Length (cm) |
55 (54-56) |
57 (56.5-57.5) |
<0.001 |
|
Weight-for-age Z-score |
-1.0 (-1.64 to -0.46) |
-0.32 (-0.55 to 0.07) |
<0.001 |
|
Length-for-age Z-score |
-0.35 (-0.97 to 0.19) |
0.28 (-0.20 to 0.68) |
<0.001 |
|
Weight-for-length Z-score |
-1.14 (-1.61 to -0.63) |
-0.55 (-1.09 to -0.06) |
0.002 |
|
Skin Fitzpatrick Score |
|
|
|
|
Score 3 |
74 (74%) |
26 (81%) |
0.48 |
|
Score 4 |
26 (26%) |
6 (19%) |
|
|
Received antenatal calcium supplementation |
93 (93%) |
31 (97%) |
0.68 |
|
Duration of antenatal calcium supplementation (d) |
75 (45-90) |
45 (30-60) |
<0.001 |
|
Maternal 25(OH)D (ng/mL) |
6.30 (4.39 – 8.06) |
3.56 (2.24 – 7.91) |
0.19 |
|
Season of recruitment |
|
|
|
|
June to August |
50 (50%) |
21 (65.6) |
0.155 |
|
March to May |
50 (50%) |
11 (34.4) |
|
|
All values in median (IQR). |
 |
|
Fig. 2 Study flow chart.
|
Median (IQR) number of days for which data on
sunlight exposure (in 100 infants) were available, was 130 (131,136)
days. The median (IQR) weekly sunlight exposure in these infants was 17
(13,23) minutes, including 11 (9,15) minutes of sun exposure before 10
am, and 5 (3,9) minutes between 10 am to 3 pm. Mothers did not expose
the infant to sunlight after 3 pm. Average fraction of body surface area
(BSA) exposed to sunlight was 6.8% (median 6%; IQR: 4.6%, 7.4%). Overall
fraction BSA exposed to sunlight ranged from 2- 40%.
The mean infant serum 25(OH)D level at 6 months of
age was 10.9 (SD 5.66) ng/mL (median 9.2, IQR: 7.34,13.36; range: 1.41
to 27.5 ng/mL). Of 100 infants completing the study, 67 (67%) had serum
25(OH)D levels below 12 ng/mL (deficient), 23 (23%) had insufficient
levels (12-20 ng/mL); and 10 (10%) had levels above 20 ng/mL
(sufficient). The infants’ serum 25(OH)D correlated positively and
significantly with cumulative sun index (Spearman correlation
co-efficient 0.461, P<0.001). Duration of sun exposure and
fraction of body surface area exposed to sunlight, independently also
correlated significantly with infant serum 25(OH)D at 6 months of age (r=0.40
and 0.459, respectively; P< 0.001).
For Model 1, cumulative sun index, maternal vitamin D
levels, and season of exposure were the major determinants of infant’s
vitamin D concentrations. Every unit increase in cumulative sun index
increased the infant’s serum 25(OH)D levels by 0.25 units. Maximum R 2
(0.367) was achieved in Model 3 when afternoon sun
index replaced cumulative sun index in the model (Table II).
Compared to maternal vitamin D concentration, the afternoon sun index
was also a better predictor of infant’s vitamin D level at 6 months of
age. A change in afternoon sun index by 1 unit was able to increase the
infant’s 25(OH)D level by 1.1 units.
TABLE II Regression Analysis of Sun Index as Predictor of Serum 25(OH)D Level of Infant
|
Independent factors |
Cumulative sun index |
Morning sun index |
Afternoon sun index model |
|
model (Model 1) |
model(Model 2) |
(Model 3) |
|
Sun Index |
0.25 (0.062, 0.440)# |
0.23 (0.01, 0.45)* |
1.07 (0.37, 1.78)# |
|
Maternal serum 25OHD |
0.67 (0.44, 0.89)# |
0.68 (0.45, 0.91)# |
0.65 (0.42, 0.87)# |
|
Season of exposure |
2.02 (0.12, 3.91)* |
2.10 (0.18, 4.01)* |
2.24 (0.39, 4.09)* |
|
Antenatal calcium supplementation |
0.10 (-3.56, 3.77) |
0.18 (-3.54, 3.90) |
-0.43 (-4.07, 3.21) |
|
Skin color |
0.33 (-1.82, 2.48) |
0.33 (-1.90, 2.45) |
0.68 (-1.45, 2.81) |
|
R2 |
0.337 |
0.367 |
0.354 |
|
Serum 25(OH)D of the infant is the dependent variable in all
models. Model 1, 2, and 3 reprsent cumulative sun index, morning
sun index and afternoon sun index, respectively. Rest of the
independent variables remain same in all 3 models; Residuals of
all models approximated normal distribution; Values expressed
as: unstandardized coefficient- B (95% confidence interval);*
P<0.05, #P<0.01. |
The 25th percentile of infant’s serum 25(OH)D
concentrations was 7 ng/mL. To achieve an additional 13 ng/mL (to attain
sufficient level of 20 ng/mL), additional 12 units of afternoon sun
index would be required. Assuming minimum fraction of body surface
exposed as 0.4 (if the child lies prone exposed to sun required with
diapers on), the duration of afternoon sunlight to achieve a sun index
of 1 will be 2.5 minutes. Thus, to achieve an increase in sun index by
13 units, one would require to have afternoon sunlight exposure of
approximately 30 minutes per week for at least 16-18 weeks. For the
winter months, if the child is fully clothed with only face and hands
exposed (approximately 10% body surface area), the required exposure is
calculated as 2 hours per week. Table III summarizes the
estimated sun exposures required to achieve sufficient serum 25 (OH)D
level (>20 ng/mL) for different baseline levels.
TABLE III Sunlight Requirement to Achieve Sufficiency Levels for Different Baseline Serum 25 (OH) D Levels
|
Baseline serum 25 (OH) |
Sun index (SI) required* to attain |
Duration of sun exposure per week (min) |
Increase in serum |
|
D levels (ng/mL) |
sufficient level of 20 ng/mL |
at 40% surface area |
at 10% surface area |
25 (OH)D levels (95% CI) |
|
5 |
14 |
35 |
140 |
14.98 (12.96-17.00) |
|
7 |
12 |
30 |
120 |
12.84 (11.11-14.57) |
|
9 |
10 |
25 |
100 |
10.70 (9.26-12.14) |
|
11 |
8 |
20 |
80 |
8.46 (7.30-9.61) |
|
14 |
6 |
15 |
60 |
6.42 (5.55-7.29) |
|
16 |
4 |
10 |
40 |
4.28 (3.67-4.89) |
|
* Sun index 1.07 raises serum 25 (OH) D by 1 unit. We
assumed that relationship between the 6 months serum 25(OH)D
levels and sun index is same as relation between the change (6
months minus baseline vitamin D) and sun index. This assumption
is made because it may not be ethical to follow an infant having
low vitamin D level without giving the supplement. |
Discussion
The present study establishes a correlation between
sun exposure during early infancy and the serum 25(OH)D levels in
infants at 6 months of age from Northern India. Sun exposure between 10
am to 3 pm emerged as the best predictor of infant’s vitamin D status,
ahead of maternal serum 25(OH)D levels. In this study, we could also
estimate the duration of sun exposure required to achieve sufficient
vitamin D levels in brestfed infants at 6 months of age.
These results were obtained in infants born to
vitamin D deficient mothers (90/100 had serum level of 25(OH)D <12 ng/mL).
These children were probably born with a poor vitamin D status. We did
not measure the infant’s vitamin D status at enrolment but presumed it
to be a surrogate reflection of maternal vitamin D status. Earlier
studies have shown a good correlation between maternal vitamin D status
and cord serum 25(OH)D levels at birth and up to 6 months of age
[13,14]. Also, the observed sun exposure during the afternoon (5-6
minutes per week on 6% of body surface area) was markedly deficient as
compared to that required (30 minutes per week on 40% of body surface
area) to achieve sufficient serum level of vitamin D, in the infant, by
6 months of age. Our results showed that only the afternoon sun exposure
could offset the disadvantages set up by low maternal vitamin D levels.
McCarty [15] raised concerns over the poor
correlation on sunlight exposure questionnaire with serum 25(OH)D
levels, owing to recall bias, interviewee fatigue due to long sessions,
and not taking into account of other factors influencing vitamin D
levels; like age variation, sunscreen application, skin color, dye,
clothing and latitude. We tried to neutralize many of these factors by
taking a cohort of same age (infant up to six months) with similar diet
(breastmilk) and of same geographical location. The predesigned sun
exposure charts consisted of easily understandable picture of infant’s
body to mark body surface area exposed to sunlight. The mothers were
asked to fill the chart daily at the time of exposure itself and their
compliance was ensured on telephonic call weekly, and direct visit on
monthly basis. Ideally, to document sun exposure exactly, these charts
should be validated on a daily basis, which was not possible in our
study due to logistic constraints. Moreover, we did not verify the
reported exposure by infant adapted ultraviolet dosimetry. Documentation
of exact UVB exposure and simultaneous correlation with the infant’s
serum 25(OH)D would have also improved the validity of our analysis on
sunlight exposure. Millen, et al. [1] have now shown that the
validity of self-administered questionnaires on sun exposures closely
matches the UV exposure measured by UVB solarmeter.
Earlier studies have also suggested tapping the
potential of exposure to sunlight for increasing vitamin D production in
the body. Few adult studies have also reported similar results and
quantified adequate sunlight exposure required [11,12,16]. Hollick [17]
recommended one minimal erythemal dose (MED) of sunlight to whole body
in young adults to increase vitamin D production to reach 20 ng/mL,
which is comparable to taking oral dose of 10000-25000 IU of
ergocalciferol. In another paper, he suggested exposure of 20% body
surface area to 0.5 MED of sunlight for similar results [18]. Specker,
et al. [19] found that infant serum 25(OH)D was significantly
related to UV exposure and maternal serum 25(OH)D. They also concluded
that an infant wearing a diaper would require 30 minutes outdoor
exposure or 2 hours a week when fully clothed without hat to raise serum
25(OH)D to a level above 11 ng/mL (UV exposure score 2.0) [19]. Despite
a geographical and racial variation, we got similar estimates in Delhi.
Our advantage over the Specker study was a larger cohort size (100 vs
48 participants) and longer period of follow up (mean 126 days vs
7 days). Hall, et al. [20] demonstrated that sufficient exposure
to sunlight was present during routine daily activities, to produce
enough vitamin D in young college students, not considering vacations.
Nurbazlin, et al. [11] found significant correlation of sun index
with serum 25(OH)D levels (r=0.180; P<0.001) in rural and
urban Malaysian women.
The afternoon sun exposure was found to be most
critical in our study instead of morning sun exposure. Alshahrani, et
al. [21] reported maximum UVB exposure during early morning (8-9 AM)
or afternoon hours (2-3 PM) in Riyadh. These differences may be due to
Zenith angle, which is responsible for variable cutaneous UVB absorption
[18].
To conclude, our study reported significant positive
correlation between sunlight exposure and infant’s serum vitamin D,
irrespective of maternal vitamin D levels. This finding holds importance
in the present scenario where much stress is being laid upon
infant/maternal vitamin D supplementation. Though UVB radiation has been
linked to increased risk of skin damage and skin cancer, it is highly
unlikely that the modest exposure suggested in our study can be
considered to increase the risk of skin malignancies. Our study has
estimated the amount of sun exposure required to maintain sufficient
vitamin D levels in infants. Whether this translates into effectiveness,
can only be answered by randomized trials on controlled sun exposure for
adequate duration as the intervention. Further research may highlight
optimal sunlight exposure and minimize excessive commercial and rampant
misuse of unwarranted vitamin D supplementation as a routine in
otherwise healthy children.
Contributors: The study was conceived by
PG. AD, PM, DS, RKM, and SVM contributed to the study design. Data
collection was handled by PM and supervised by AD, DS, SVM and PG. SVM
also supervised the laboratory work-up for vitamin D status. Statistical
analysis was carried by RKM and PG. Literature search was conducted by
AD, PM, and PG. Initial draft of the manuscript was written by PM and AD
which was edited and refined by PG. DS, SVM, and RKM provided critical
inputs to the draft manuscript. The manuscript was approved by all
authors.
Funding: Indian Council of Medical
Research; and University College of Medical Sciences.
Competing interests: None stated.
|
What is Already Known?
• Endogenous vitamin D synthesis occurs
due to ultraviolet B rays of sunlight, which is affected by
season, latitude, timing of day and melanin content.
What this Study Adds?
• There is a
significant correlation between sunlight exposure and serum
vitamin D in breastfed infants at 6 months of age.
• Afternoon sun
exposure of 30 minutes per week for 16-18 weeks (starting from 6
weeks) over 40% exposed body surface can achieve sufficient
vitamin D (20 ng/mL) in infants, at 6 months of age.
|
References
1. Millen AE, Bodnar LM. Vitamin D assessment in
population-based studies: a review of the issues. Am J Clin Nutr.
2008;87:1102S-5S.
2. Jain V, Gupta N, Kalaivani M, Jain A, Sinha A,
Agarwal R. Vitamin D deficiency in healthy breastfed term infants at 3
months and their mothers in India: seasonal variation and determinants.
Indian J Med Res. 2011;133:267-73.
3. Bhalala U, Desai M, Parekh P, Mokal R, Chheda B.
Subclinical Hypovitaminosis D among exclusively breastfed young infants.
Indian Pediatr. 2007;44:897-901.
4. Balasubramanian S, Shivbalan So, Kumar PS.
Hypocalcemia due to vitamin D deficiency in exclusively breastfed
infants. Indian Pediatr. 2006;43: 247-51.
5. Wagner CL, Greer FR. American Academy of
Pediatrics Section on Breastfeeding; American Academy of Pediatrics
Committee on Nutrition. Prevention of Rickets and Vitamin D Deficiency
in Infants, Children, and Adolescents. Pediatrics. 2008;122:1142-52.
6. Armas LA, Dowell S, Akhter M, Duthuluru S, Huerter
C, Hollis BW, et al. Ultraviolet-B radiation increases serum
25-hydroxyvitamin D levels: the effect of UVB dose and skin color. J Am
Acad Dermatol. 2007;57:588-93.
7. Rossberg W, Saternus R, Wagenpfeil S, Kleber M,
März W, Reichrath S, et al. Human pigmentation, cutaneous vitamin
D synthesis and evolution: Variants of genes (SNPs) involved in skin
pigmentation are associated with 25(OH)D serum concentration. Anticancer
Res. 2016;36:1429-37.
8. Institute of Medicine. Dietary reference intakes
for calcium and vitamin D. Washington, DC: The National Academies Press;
2011.
9. Fitzpatrick TB. The validity and practicality of
sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-71.
10. Determining Depth and Percentage of Burn
Injuries. Available from: https://
www.firefighternation.com/forum/topics/889755:Topic:2902596.
Accessed May 24, 2014.
11. Nurbazlin M, Chee WS, Rokiah P, Tan AT, Chew YY,
Nusaibah AR, et al. Effects of sun exposure on 25(OH) vitamin D
concentration in urban and rural women in Malaysia. Asia Pac J Clin Nutr.
2013;22:391-9.
12. Barger-Lux JM, Heaney RP. Effects of above
average summer sun exposure on serum 25 (OH)-D and calcium absorption. J
Clin Endocr Metab. 2002;87:4952-6.
13. Steichen JJ, Tsang RC, Gratton TL, Hamstra A,
DeLuca HF.Vitamin D homeostasis in the perinatal period:
1,25-dihydroxyvitamin D in maternal cord and neonatal blood. N Engl J
Med. 1980;302:315-9.
14. Lamberg-Allardt C, Larjosto M, Schultz E.
25-Hydroxyvitamin D concentrations in maternal and cord blood at
delivery and in maternal blood during lactation in Finland. Hum Nutr
Clin Nutr. 1984;38:261-8.
15. McCarty CA. Sunlight exposure assessment: can we
accurately assess vitamin D exposure from sunlight questionnaires? Am J
Clin Nutr.2008;87:1097S-101S.
16. Goswami R, Saha S, Sreenivas V, Singh N, Lakshmy
R. Vitamin D-binding protein, vitamin D status and serum bioavailable
25(OH)D of young Asian Indian males working in outdoor and indoor
environments. J Bone Miner Metab. 2016 Jan 30. [Epub ahead of print].
17. Holick MF. Environmental factors that influence
the cutaneous production of vitamin D. Am J Clin Nutr. 1995;61:638S-45S.
18. Holick MF. Sunlight and vitamin D for bone health
and prevention of autoimmune diseases, cancers, and cardio-vascular
disease. Am J Clin Nutr. 2004;80:1678S-88S.
19. Specker BL, Valanis B, Hertzberg V, Edwards N,
Tsang RC. Sunshine exposure and serum 25-hydroxyvitamin D concentrations
in exclusively breast-fed infants. J Pediatr. 1985;107:372-6.
20. Hall LM, Kimlin MG, Aronov PA, Hammock BD,
Slusser JR, Woodhouse LR, et al. Vitamin intake needed to
maintain target serum 25-hydroxyvitamin D concentrations in participants
with low sun exposure and dark skin pigmentation is substantially higher
than current recommendations. J Nutr. 2010;140:542-50.
21. Alshahrani FM, Almalki MH, Aljohani N, Alzahrani
A, Alsaleh Y, Holick MF. Vitamin D: Light side and best time of sunshine
in Riyadh, Saudi Arabia. Dermatoendocrinol. 2013;5:177-80.
|
|
|
 |
|

